February 19, 2026 • min read
Value-based care programs: 3 examples in practice
Three value-based care program examples in practice, with buyer lessons employers and health plans can use in MSK to make outcomes auditable and pricing clear.
Written by

Evidence-based healthcare insights
Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- The “value-based” care model only delivers on its promise when there’s a clear outcome, a clear price, and a clear way to verify both.
- In MSK, programs work best when they move care upstream, reduce low-value escalation, and make results auditable.¹ ³
- Transparency is the unlock: when you can see what you are paying for and when payment triggers, you can finally compare vendors with confidence and security ⁶
Why skeptical buyers are right to ask for “real-world examples”
If you sit in benefits, finance, or health plan administration, you have seen the word “value-based” stretched well beyond it's promise. A program claims value, but the contract reads like fee-for-service. Reporting looks polished, but you cannot reconcile it to billing. Outcomes are talked about as the focus, but the definition moves the moment performance is questioned.
That skepticism is healthy. In healthcare, incentives are powerful. If you can align the financial incentives of the care provider with a payment model that ties your fees to measurable health outcomes, you can expect accountability to those outcomes.
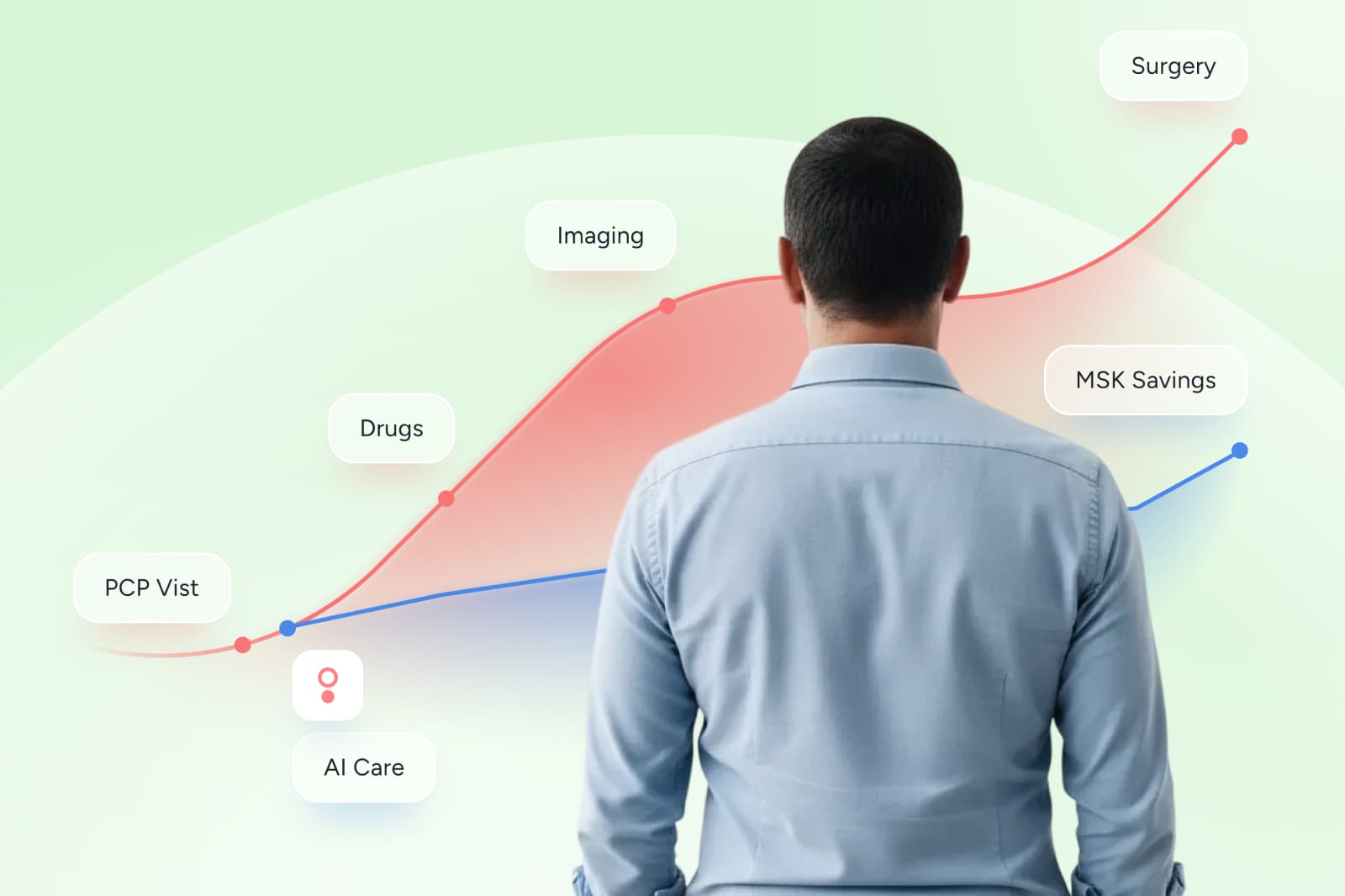
Musculoskeletal care is one of the clearest places to consider a transition to value-based care standard because MSK spend is high, escalation can be fast, and the difference between “more care” and “better care” shows up in function, quality of life, and downstream utilization.¹ ⁸
What makes a value-based care program credible
Across industries and geographies, the programs that hold up under scrutiny tend to share four important design features:
1. A defined outcome (not a vague promise)
Look for validated measures of improvement, not satisfaction scores alone. In MSK, that often means patient-reported outcome measures tied to function and quality of life, tracked consistently over time.⁶
2. A defined scope
The contract should state who is included, when they qualify, and what happens when a member disengages or has incomplete data. If scope is fuzzy, spend will be, too.
3. A defined payment trigger
You should be able to point to a clause and say: “This is what must be true for billing to happen.” If you cannot, you are still in a fee-for-service world, just with nicer branding.⁶ ⁷
4. Verification rights
Value-based programs earn trust when buyers can audit outcomes and reconcile performance reporting to financial reporting. That is how you avoid hidden fees dressed up as “implementation,” “care navigation,” or “clinical support.”
3 value-based care program examples to consider
Below are three program types that have demonstrated measurable impact in MSK healthcare and adjacent categories. They are not perfect, but buyers can take inspiration and some learnings from these in-practice examples to help separate value-based care promises from results.
Example 1: Bundled payments that make the episode the unit of accountability
Bundled payments can work when the episode is defined clearly and the payment creates true accountability for complications and rework.
In Stockholm, Sweden, a bundled payment model for elective hip and knee replacement was associated with improvements such as a reduction in reoperations after implementation, alongside cost reductions over the full cycle of care reported in the evaluation.¹ A separate quasi-experimental analysis in the same setting examined how competition and bundled payment related to performance measures like length of stay and adverse events.²
The lesson for buyers is not just to “copy this model.” Instead, the message is more generalized. Bundles become meaningful when they force the healthcare vendors to standardize care, manage avoidable variation, and own the downstream consequences.¹ ²
- The buyer lesson: predictable spend starts with a clear “unit of purchase”
- How to apply it: contract for the episode, not the billing trail
Value-based care becomes real when the “unit of purchase” is clearly defined and priced up front. Instead of paying for a long trail of bills, employers and plans set expectations for what the episode includes, what it costs, and how performance is tracked. For a benefits or finance leader, that clarity is the point: it makes MSK spend easier to forecast, easier to explain internally, and harder for low-value variation to hide in the noise.³
Example 2: Programs that move MSK upstream, before escalation becomes spend
MSK is where “more care” can easily become “more utilization.” Low-value procedures and low-value imaging are well-documented problems in degenerative MSK pathways.³
Value-based MSK programs win when they create a reliable early pathway that is easier to access than escalation. That is where structured exercise and behavior change support can be so effective. This preventative care can reduce the demand for the high-cost branch of the tree.

A longitudinal comparison study of a digital MSK program for acute and subacute pain found greater improvements in pain scores among participants than among a comparison group over short follow-up windows.⁴ And a randomized controlled trial in chronic low back pain found a remote digital intervention produced similar improvements to evidence-based in-person physiotherapy, with lower dropout in the digital group.⁵
When deciphering the clinical language, the lesson is that you do not need to debate “digital versus traditional” to use the insight. Look for programs that scale consistent care, matche objective guidelines, and measure change frequently. They are easier to contract around because the outcomes are clear and trackable.⁴ ⁵
- The buyer lesson: reduce variation before you chase savings
- How to apply it: measure progress early and standardize pathways
Payment reform works best when it is paired with operational discipline. Outcomes improve when care is designed to be consistent, measurable, and repeatable, not dependent on which door a member walks through.
For MSK buyers, this is a reminder to ask how a vendor reduces pathway variation at scale, how often they measure progress, and what they do when someone is not improving.²
Example 3: Outcome-based pricing that makes spend defensible and forecastable
The most buyer-friendly value-based programs do something that is surprisingly rare in healthcare: they make billing legible.
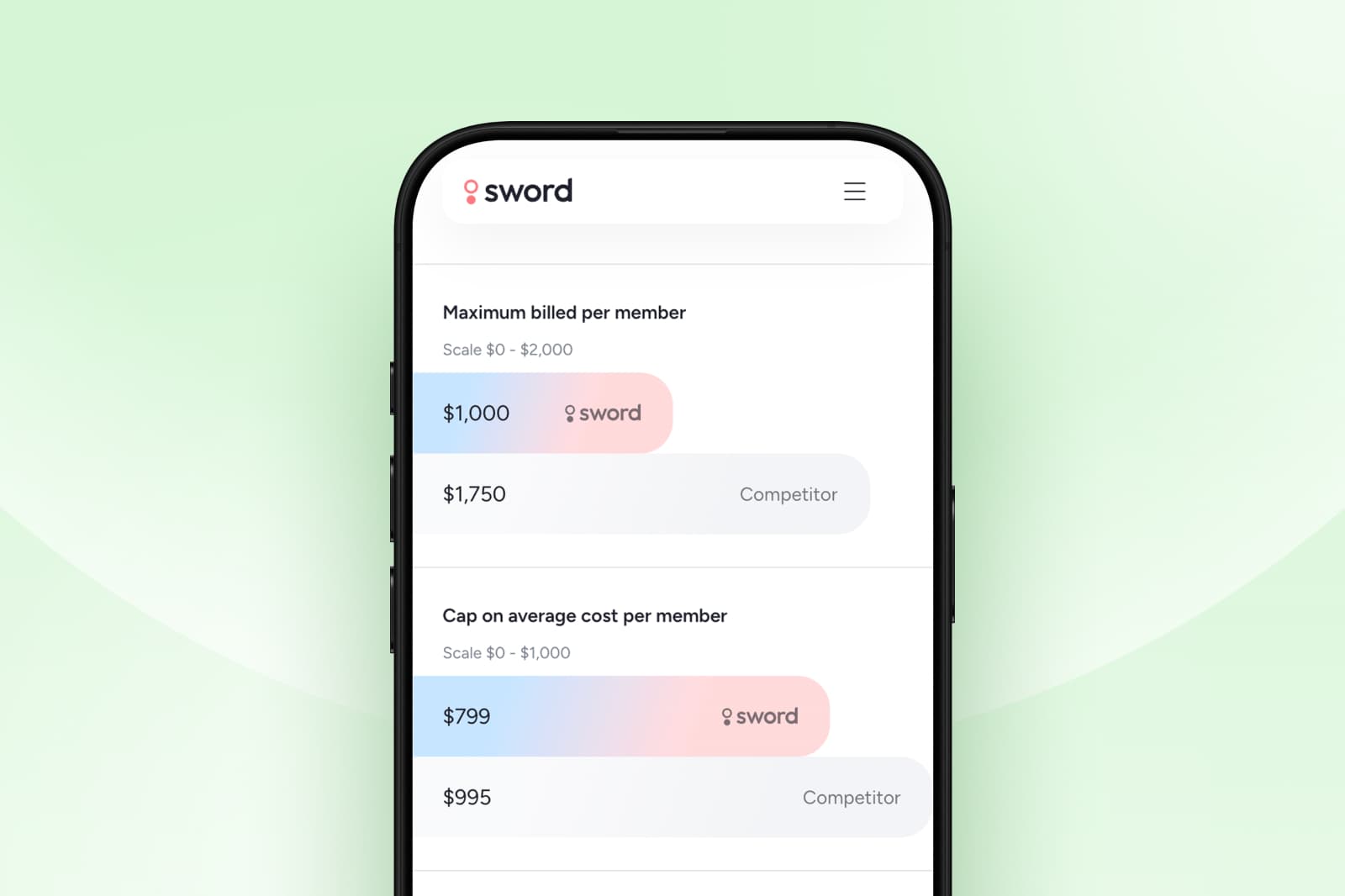
Sword Health’s Outcome Pricing is designed so clients do not pay in full unless members achieve meaningful, predefined improvement.⁶ It is a model built for governance: outcomes are defined, triggers are explicit, and reporting is designed to be auditable.⁶
For finance leaders, the practical value is that predictable triggers create predictable forecasting. For benefits leaders, it means you can finally separate “engagement” from “impact” in contract language and stop paying for activity that does not translate into recovery.
Sword has also published third-party ROI validation, including an independent analysis by Risk Strategies Consulting to confirm Sword’s methodology.⁷
GUARANTEED SAVINGS
Get the industry's highest ROI rate with Sword
70%
reduction in surgery intent
41.6%
fewer ancillary services
10%
drop in MSK-related MRIs
35%
reduction in spine surgeries
Changing the payment model can improve some aspects of performance, but “value” is not automatic unless outcomes are defined and tracked in a way that holds the system accountable.
- The buyer lesson: make billing legible and accountability enforceable
- How to apply it: tie payment to auditable improvement, not activity
For benefits leaders and health plan managers, the transferable lesson is to separate operational improvements from recovery outcomes, and to work off contracts that make both visible.
Simply, aim for a program than can show measurable improvements and match these to payments.⁴ ⁵
Inspiration you should take from the best healthcare programs
You do not have to adopt any single program structure to raise your standard. You can take the best design constraints and apply them to every vendor conversation.
Here is the operator mindset shift that matters most: stop asking vendors to describe value, and start asking them to operationalize it with measurable outcomes. That change alone makes hidden fees harder to defend.
10-question checklist to evaluate “value-based” MSK programs
Use these questions to pressure-test contracts and dig deeper than sales decks. You can come armed with this list to the conversations you have throughout the research process:
- What exact outcome measures define success, and are they validated? ⁶
- What threshold counts as “meaningful improvement,” and is it the same across cohorts? ⁶
- What triggers payment, and what explicitly does not trigger payment? ⁶
- How is missing outcome data handled, and how does that affect billing?
- Can you provide a sample report that reconciles outcomes to invoices?
- What audit rights do we have, and what is the dispute process?
- Are there caps, risk corridors, or stop-loss terms that protect forecasting?
- How do you prevent low-value escalation and avoidable procedures? ³ ⁸
- How do you ensure equitable access so value does not depend on “easy” members?
- What implementation lift is required, and what is included versus billed separately?
If a vendor struggles to answer these, it is usually a sign that the model is not truly value-based. Instead, you could be dealing with a similar experience to a fee-for-service care provider with an inability to track and measure value and outcomes.
Price transparency only helps when outcomes and payment triggers are clear
Price transparency is not just a compliance topic. For buyers, it is the difference between managing MSK as a controllable investment versus absorbing it as an unpredictable tax.
When outcomes and pricing are transparent together, you can:
- Compare MSK partners on shared definitions, not competing narratives
- Forecast spend based on known triggers rather than claims volatility
- Defend purchasing decisions in procurement and governance
- Push the system away from billing complexity and toward recovery
That is the deeper reason MSK is such an important proving ground. Movement is measurable. Recovery is measurable. When you pair measurable outcomes with measurable payment triggers, the healthcare system has fewer places to hide.
See why Sword’s outcome pricing delivers industry-leading ROI
By this point, the pattern should feel clear: the programs that hold up in the real world are not “value-based” because they say they are. Effective vendors earn that label because they make two things unavoidably concrete, what improvement means and what, exactly, you pay for when improvement happens.
That is also where most MSK evaluations break down. Vendors can show engagement charts and compelling stories, but procurement and finance teams still need contract terms they can defend, forecast, and govern. The fastest way to cut through the noise is to review the mechanics side by side, in plain language, with the reporting you would actually use in QBRs.
Sword pioneered Outcome Pricing in digital MSK, and we built it for the exact moment you’re in now: when “value-based” claims have to survive procurement, finance review, and renewal scrutiny. With independently validated ROI and clear, auditable payment triggers, Sword gives you a straightforward way to pressure-test outcomes, compare models, and move forward with confidence instead of assumptions.⁶⁷
Set up a call with a Sword expert and we will walk through:
- The outcome measures and improvement thresholds that define success⁶
- The billing triggers and non-triggers, so you can see what gets paid for and what does not⁶
- What reporting looks like for finance, consultants, and governance, including how results reconcile to invoices⁶
If you want to explore the model first, you can also review Sword’s transparent, outcome-based pricing before you jump on the call.
Start saving $3,177 per member per year
Slash MSK costs and get the industry’s top validated ROI of 3.2:1.
Footnotes
Karolinska Institutet. Effects of introducing bundled payment and patients' choice of provider for elective hip and knee replacements in Stockholm county. (PDF)https://ki.se/media/95244/download
Goude F, et al. Effects of competition and bundled payment on the performance of hip replacement surgery in Stockholm, Sweden: results from a quasi-experimental study. BMJ Open. 2022;12:e061077.https://bmjopen.bmj.com/content/12/7/e061077
Siemieniuk RAC, et al. Knee arthroscopy versus conservative management in patients with degenerative knee disease: systematic review. BMJ Open. 2017;7:e016114. (PDF)https://bmjopen.bmj.com/content/7/5/e016114.full.pdf
Wang G, et al. Clinical Outcomes After a Digital Musculoskeletal Program for Acute and Subacute Pain: Observational, Longitudinal Study With Comparison Group. JMIR.https://doi.org/10.2196/38214
Cui D, et al. Randomized-controlled trial assessing a digital care program versus conventional physiotherapy for chronic low back pain. npj Digital Medicine. 2023;6:121. (PDF)https://www.nature.com/articles/s41746-023-00870-3.pdf
Sword Health. How outcome pricing aligns costs with measurable results.https://swordhealth.com/newsroom/outcome-pricing
Sword Health. Cut MSK costs with predictive care: Risk report (Risk Strategies Consulting analysis).https://swordhealth.com/reports-and-guides/risk-strategies-consulting-analysis
Sword Health. The MSK Money Pit: Low-value care in MSK. https://swordhealth.com/reports-and-guides/risk-strategies-consulting-analysis