November 28, 2025 • min read
How to prevent hip joint pain in menopause
Learn why menopause can cause hip joint pain and discover evidence-backed ways to ease stiffness, build strength, and move comfortably again.
Written by

Evidence-based healthcare insights
The Sword summary warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Hip discomfort is common during menopause because declining estrogen affects collagen, joint lubrication, and muscle balance¹².
- These changes are normal and manageable, and many women find meaningful relief with steady movement, supportive habits, and guided musculoskeletal care.
- Move, Sword Health’s digital musculoskeletal program, helps women build strength, improve joint comfort, and move with confidence through personalized sessions completed at home.
Why does hip pain become more noticeable during menopause?
Many women begin to feel new sensations around their hips during menopause, such as stiffness in the morning, soreness after sitting, or a deep ache after walking. These changes can feel unsettling, especially if movement once felt easy and predictable.
Menopause affects several parts of the body, including the tissues that support your joints. Estrogen helps maintain collagen, fiber elasticity, and the natural lubrication your joints rely on to move comfortably¹. When estrogen levels fluctuate and then decrease, those tissues can feel less flexible and more sensitive, especially during movements that require stability, like standing up from a chair or walking briskly.
These changes do not mean your joints are deteriorating. They indicate that your tissues are adapting to a new hormonal environment. Once you understand this connection, hip discomfort becomes easier to navigate, and you can begin to take steps that support lasting comfort.
What changes in the body can cause hip discomfort in menopause?
Hip discomfort often has more than one cause during menopause. Hormonal changes, muscle imbalances, and lifestyle factors all play a role. Understanding these influences can help you make sense of your symptoms. Some of the most common changes include:
- less collagen and flexibility in the tissues supporting your hip²
- changes in natural joint lubrication that make movement feel stiff
- slower muscle recovery after activity
- mild increases in inflammation that can make hips feel tender after rest or movement²
- uneven muscle strength or tightness that shifts pressure onto the joint³
These changes are reversible. With movement, balanced strength, and supportive habits, most women feel improvement within weeks.
How muscle balance and pelvic support affect hip comfort
Your hips are part of a connected system that includes your core, your back, your glutes, and the pelvic floor. When these muscles work together, they help stabilize your hips and keep movement comfortable.
During menopause, these muscles can weaken, tighten, or work less efficiently, especially if you spend long hours sitting³. This can increase pressure on the hip joints and the tissues around them, which can make everyday movements feel more difficult.
Strengthening and rebalancing these muscles helps support the hips. Many women notice significant relief once the core, glutes, and pelvic floor begin working together again.

How to tell if hip discomfort is related to menopause
Because hip discomfort can come from many sources, noticing patterns can help you understand what your body may be communicating. Your symptoms may be related to menopause if you notice:
- stiffness that improves with gentle movement
- aching on both sides rather than one
- discomfort that appears alongside menopause symptoms like sleep changes
- soreness after long periods of sitting
If pain is sharp, constant, or focused on one side, especially if it interferes with walking or rest, check with a clinician to rule out bursitis, arthritis, or injury⁵.
Everyday factors that can worsen hip stiffness
It helps to understand how lifestyle factors influence hip comfort. These patterns are common, especially during midlife when responsibilities and routines may limit movement.
Long periods of sitting can shorten the hip flexors and reduce activation of the glutes and core, which places more strain on the hips. Lower daily activity levels can weaken supporting muscles, and poor posture can shift pressure onto the joint.
The encouraging part is that these patterns can be changed. Even small posture adjustments, mobility breaks, and gentle stretching throughout the day can help restore comfort and reduce strain.
How to relieve and prevent hip discomfort during menopause
Menopause-related hip discomfort often improves with consistent, gentle habits. You do not need high-intensity workouts for relief. Your hip tissues respond well to steady, supportive movement.
Before exploring these strategies, remember that hip discomfort is often a signal that tissues need movement, nourishment, and balanced support. These suggestions are starting points you can adapt to your daily routine.
1. Keep your hips moving throughout the day
Movement helps lubricate joints, increase circulation, and ease stiffness. Walking, gentle stretching, or mobility routines can help your hips feel smoother and more flexible. Even 10 minutes of gentle movement can make a difference⁶.
2. Strengthen the muscles that support your hips
Strong glutes, core, and pelvic floor muscles help stabilize your hips and reduce strain³. Simple exercises such as bridges, wall sits, or side-lying leg lifts can help rebuild strength. Strengthening consistently, even twice a week, often leads to noticeable improvement. If you want structure or guidance, Move offers personalized strength and mobility plans that adjust to your comfort level.
3. Support your tissues with nourishing foods and hydration
Anti-inflammatory foods can help reduce stiffness. Omega 3-rich foods such as salmon or walnuts support tissue comfort⁷. Calcium and vitamin D help maintain bone strength, and magnesium supports muscle relaxation. Staying hydrated helps keep tissues elastic and reduces tightness⁸.
4. Protect recovery and reduce daily stress
Sleep is essential for tissue repair. Hormonal changes can influence inflammation and pain sensitivity, so good rest supports comfort⁹. Short relaxation routines such as breathing exercises, light yoga, or bedtime stretching can help your hips feel calmer.
How Move helps women reduce hip discomfort in menopause
Move is Sword Health’s digital musculoskeletal program designed to reduce pain, improve mobility, and help women stay active with confidence. It brings expert guidance into your home and provides personalized exercises that support hip comfort.
Move helps people regain strength, mobility, and daily comfort through structured support. For women in menopause, Move offers gentle, tailored guidance that adapts to changes in recovery, flexibility, and energy during this phase.
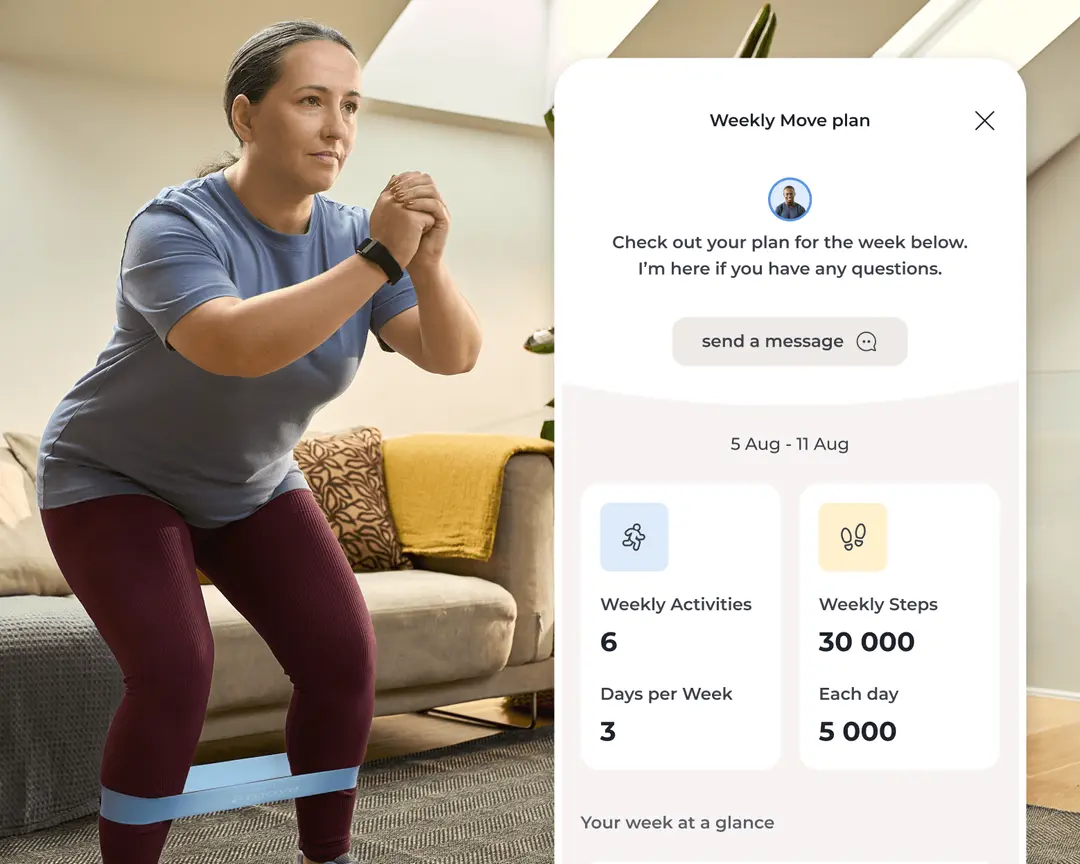
Every member works one-on-one with a Physical Health Specialist who holds a Doctor of Physical Therapy degree. Your specialist learns about your hip symptoms, movement patterns, and daily routines, then builds a plan to support your hip joint and the muscles that stabilize it. You can access your care plan whenever and wherever you like through the Sword mobile app. All you need is your Move wearable, to track progress for your matched specialist, and you can easily complete your exercises within a 10-15 minute block.
Get started with Sword Move for whole-body strength
1. Tell us about you
We’ll learn about your goals, job type, lifestyle, and movement history.

2. Match with a Physical Health Specialist
Your dedicated Sword Move specialist will create a personalized plan just for you.

3. Receive your Move kit
You’ll get a free Move wearable and resistance bands delivered to your door.
4. Start moving with your personalized plan
Pair your Move wearable and begin weekly goals built around your activity level, routines, and progress.
Why digital care helps to reduce hip pain
A clinical study from Sword Health looked at how people with chronic hip pain responded to a fully remote digital care program⁵. Although this study was not specific to Move, it shows why digital support can be so effective. People in the study reported less pain and better hip function after completing the program. Many also felt more confident in their daily movement and were less certain they needed hip surgery.
One of the reasons digital care works well is consistency. Because sessions can be done from home, people completed nearly three sessions per week on average⁵, and most finished their full program. When care is easy to access and fits into daily life, it becomes much easier to stick with.
Move is built on these principles. Personalized guidance, real-time feedback, and flexible sessions help women strengthen the muscles that support the hips and move more comfortably during menopause. Move outcomes show similarly strong results. Among Move members:
- 67 percent report feeling better or much better overall¹⁰
- 74 percent report improvement in self-rated health quality¹⁰
- 49 percent show reduced risk for developing anxiety disorders¹⁰
How to take your next step and prevent pain with Move
If your hips and joints have been feeling sore or less stable during menopause, don't worry. You are not alone. These experiences are common during menopause and often improve with consistent, guided support.
Move provides a simple way to stay active without complicated routines or long workouts. With consistent support from your Physical Health Specialist, you can strengthen the muscles around your hips, improve mobility, and feel steadier in your daily life.
Many employers and health plans offer Move as a covered benefit. Check your eligibility (it only takes a moment), and you might already have coverage in your plan at $0 cost to you.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Avis NE, et al. JAMA Internal Medicine. 2015;175(4):531–539. https://doi.org/10.1001/jamainternmed.2014.806
Roman-Blas JA, et al. Arthritis Research and Therapy. 2009;11(5):241. https://doi.org/10.1186/ar2791
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Warburton DE, et al. CMAJ. 2006;174(6):801–809. https://doi.org/10.1503/cmaj.051351
Janela D, et al. Digital care programs for chronic hip pain. Healthcare. 2022;10(8):1595. https://doi.org/10.3390/healthcare10081595
Finan PH, et al. The Journal of Pain. 2013;14(12):1539–1552. https://doi.org/10.1016/j.jpain.2013.07.005
Calder PC. Nutrients. 2021;13(1):146. https://doi.org/10.3390/nu13010146
Kenefick RW. Sports Medicine. 2018;48(S1):31–37. https://doi.org/10.1007/s40279-017-0845-3
Irwin MR. Physiological Reviews. 2015;95(2):553–605. https://doi.org/10.1152/physrev.00032.2014
Sword Health. Move Outcomes Data, Book of Business 2024. Internal proprietary data.