February 19, 2026 • min read
Value-based payment models explained for healthcare buyers
Understand the major value-based payment models in healthcare and what they mean for cash flow, risk, forecasting and beyond.
Written by

Evidence-based healthcare insights
Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Value-based payment aligns reimbursement with outcomes, quality, or efficiency rather than service volume.³
- Shared savings, bundled payments, capitation, and outcome-based pricing shift financial risk, cash flow timing, and accountability in different ways.³
- MSK is a strong proving ground because procedure rates vary widely, low-value utilization can still occur, and outcomes can be tracked at scale using validated measures.⁴ ⁵ ⁶ ⁷ ⁸
Why value-based payment simplifies forecasting
MSK spend is hard to forecast because costs do not behave like a steady trend line. They can show up as regional variation in procedures, uneven utilization, and late-arriving claims that create reserve volatility.⁴ ⁵ When incentives reward volume, it becomes harder to separate what is necessary from what is simply billable.
Value-based payment (VBP) changes that equation by tying reimbursement to performance, not just activity. The goal is not to pick the most complex model. It is to choose a structure that creates the right level of accountability without adding operational friction you cannot support.³
Comparing value-based payment models
The value-based care payment is a term used to describe a reimbursement models that shift incentives for healthcare providers toward outcomes, quality, or efficiency. In comparison, the more traditional 'fee-for-service' model incentivizes volume and quantity of care. These are the most common structures and what they typically mean for cash flow and forecasting.
| Healthcare model | What triggers payment | Cash flow timing | Where it can break |
|---|---|---|---|
Pay-for-performance | Bonus for quality metrics | Add-on bonus | Too small to change MSK cost behavior on its own |
Shared savings | Spend below a benchmark | Retrospective reconciliation | Benchmarks and attribution can be difficult when variation is high |
Bundled payments | Fixed price per episode | Predictable per episode | Does not address pre-episode escalation and chronic MSK patterns |
Capitation | Fixed PMPM for a population | Very predictable | Requires strong risk adjustment and guardrails |
Outcome-based pricing | Verified improvement | Milestone-based | Requires clear measures and auditable reporting |
Pay-for-performance is often a quality add-on. It rarely changes MSK spend on its own. Shared savings can work, but this depends heavily on benchmark design and reconciliation, which can be harder to defend in musculoskeletal healthcare.³ ⁴ ⁵
Bundles are useful for defined procedures like joint replacement, but they do not solve upstream escalation and variation.⁴
Capitation can stabilize budgeting, but it requires mature risk adjustment and quality oversight.
Outcome-based pricing: the superior accountability signal
Outcome-based pricing ties a meaningful portion of payment to verified healthcrare improvements. The best value-based care providers ensure that clients have clear data to validate performance. When the model is designed well, it creates a clear and auditable structure:
- Outcomes and thresholds are defined upfront
- Payment triggers are transparent
- Reporting supports verification
- Cash flow follows predictable milestones rather than claim volume
This is what buyers should seek during vendor evalution to ensure any value-based care delivery or outcome-linked pricing is genuine and sustainable. Instead of debating what counts as value after the fact, the contract should define what improvement means and when payment is earned.⁹ ¹⁰
If you are comparing potential healthcare partners, a short contract walkthrough is often the fastest way to evaluate the best fit. Keep the above considerations in mind when you set up a call and ask to see billing triggers, outcome thresholds, mechanisms for measurement, and how your team can validate reporting.⁹ ¹⁰
Sword’s industry-first outcome pricing simplifies healthcare success
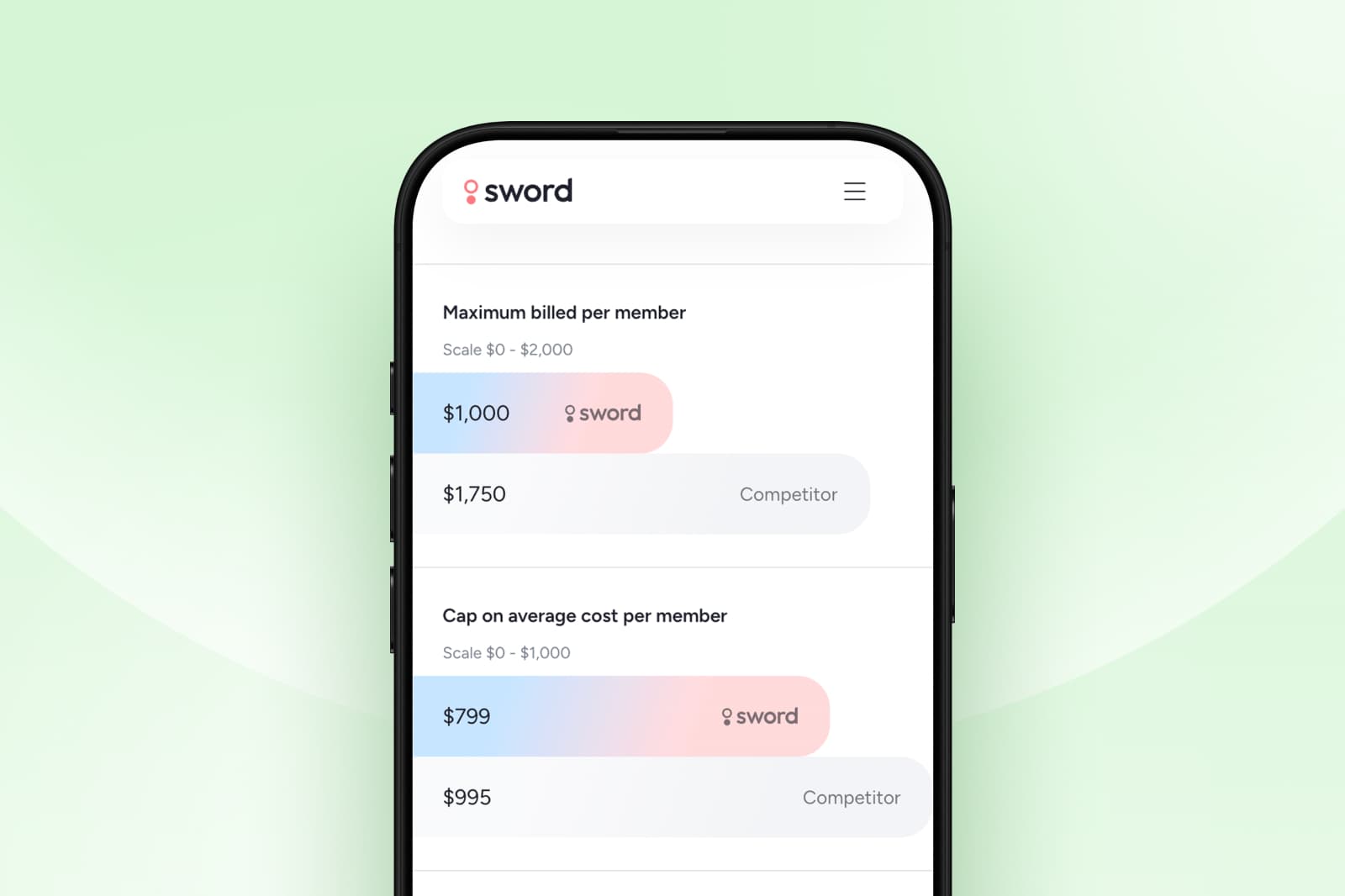
Sword Health introduced Outcome-based pricing as a contract structure that ties payment to measurable healthcare improvements. This makes billing triggers clear, predictable, and transparent.⁹
- Payment triggers are tied to predefined outcome thresholds
- Reporting supports auditability and verification
- Pricing is structured to be predictable and transparent for teams evaluating ROI and trend impact ⁹ ¹⁰
How cash flow patterns differ between healthcare payment models
Different models create different financial signatures and understanding the unique elements will help finance teams anticipate budget impact and governance requirements before renewal or expansion.
- Fee-for-service: variability that follows claim volume, coding, and utilization spikes
- Shared savings: retrospective reconciliation that can vary year to year
- Bundles: predictable within defined episodes
- Capitation: steady PMPM budgeting
- Outcome-based pricing: milestone-driven payments tied to measurable thresholds
Administrative work can also be a hidden driver of cost and complexity in volume-based reimbursement environments. The fee-for-service healthcare model tends to make tracking and analysis very difficult, which is one reason many buyers look for models that simplify what must be billed, tracked, and reconciled.¹ ²
Risk distribution between payer and vendor
| Model | Payer risk | Provider or vendor risk |
|---|---|---|
Fee-for-service | High | Low |
Pay-for-performance | High | Low |
Shared savings | Medium | Medium |
Bundled payments | Medium | Medium |
Capitation | Low | High |
Outcome-based pricing | Low | Meaningful |
No model is universally best. The right choice depends on the behavior you are trying to change, the maturity of your measurement infrastructure, and how much accountability you want from the vendor or provider group.³
Why MSK is a strong proving ground for value-based healthcare
Analysis of musculoskeletal healthcare insurance often shows value-based performance clearly because several conditions are true at once:
- Procedure rates vary widely across regions for common MSK interventions, which signals inconsistent practice patterns and uneven costs.⁴ ⁵
- Avoidable imaging and low-value procedures can still occur, creating waste and member friction.⁶ ⁷
- Clinical guidance for many common MSK conditions supports conservative approaches like physical therapy to avoid more costly interventions like injections, opiods or surgery
- Recovery and progress with musculoskeleta problems can be tracked with validated pain and function measures more explicitly than for other healthcare line items⁸
- Digital MSK programs can standardize care pathways and produce consistent outcome reporting at scale, which makes outcome-linked contracts easier to govern.⁹ ¹⁰
What to look for in an effective value-based MSK contract
Most value-based claims sound similar in a pitch. The differentiator is whether the contract and reporting make accountability real in finance terms.
Look for the following checks from value-based healthcare providers:
- Validated outcome measures that reflect functional change
- Clear improvement thresholds so payment triggers are easy to understand
- Simple financial components that map to member milestones
- Meaningful shared risk that reinforces accountability
- Reporting that supports verification for QBRs and forecasting
- Access standards that reduce the risk of selection bias
How Sword’s outcome pricing simplifies healthcare success
Sword Health introduced Outcome Pricing as a contract structure that ties payment to measurable healthcare improvements. This makes billing triggers clear, predictable, and transparent.⁹
- Payment triggers are tied to predefined outcome thresholds
- Reporting supports auditability and verification
- Pricing is structured to be predictable and transparent for teams evaluating ROI and trend impact ⁹ ¹⁰
GUARANTEED SAVINGS
Get the industry's highest ROI and slash MSK spend with Sword
3.2x
Average ROI (the industry's highest independently-validated rate)
70%
reduction in surgery intent
41%
fewer ancillary services
10%
drop in MSK-related MRIs
35%
reduction in spine surgeries
Choose the right model for your MSK strategy
Value-based payment is a spectrum. Shared savings, bundles, capitation, and outcome-based pricing can all align spending with value, but they carry different tradeoffs in operational lift and financial predictability.
For MSK, outcome-based pricing can be one of the clearest paths forward when you want a clean financial signal. This pricing structure rewards measurable success and realigns the financial incemntives for the healthcare provider to focus on quality and effectiveness of service rather than volume. This mechanism means buyers can expect validated improvements, earlier intervention, and clearer analysis that is easier to verify than models that rely heavily on benchmarks and retrospective reconciliation.³ ⁹ ¹⁰
If you are evaluating MSK partners this year, the most useful next step is a short contract walkthrough that shows how outcomes are measured, what triggers payment, and what your team can verify in reporting. Sword delivers the industry’s highest independently-validated ROI of 3.2x with an outcome-based pricing model that guarantees savings within plan year.
Set up a chat with a Sword expert to see what outcome pricing would look like for your population, plan design, and procurement requirements.¹⁰
Start saving $3,177 per member per year
Slash MSK costs and get the industry’s top validated ROI of 3.2:1.
Footnotes
Cutler DM, Ly DP. The (Paper)Work of Medicine: Understanding International Medical Costs. Journal of Economic Perspectives. 2011;25(2):3-25. https://www.aeaweb.org/articles?id=10.1257/jep.25.2.3
Jiwani A, Himmelstein DU, Woolhandler S, Kahn JG. Billing and insurance-related administrative costs in United States’ health care: synthesis of micro-costing evidence. BMC Health Services Research. 2014;14:556. https://link.springer.com/article/10.1186/s12913-014-0556-7
Health Care Payment Learning & Action Network (HCP-LAN). 2023 APM Measurement Effort Methodology and Results Report (CY 2022 data). 2023. https://hcp-lan.org/wp-content/uploads/2025/12/2023-APM-Measurement-Effort-Methodology-Report.pdf
Fisher ES, Bell J-E, Tomek IM, Esty AR, Goodman DC. Trends and Regional Variation in Hip, Knee, and Shoulder Replacement. A Dartmouth Atlas Surgery Report. 2010. https://data.dartmouthatlas.org/downloads/reports/Joint_Replacement_0410.pdf
Ward MM, Dasgupta A. Regional Variation in Rates of Total Knee Arthroplasty Among Medicare Beneficiaries. JAMA Network Open. 2020;3(4):e203717. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2765054
Mohammed HT, Yoon S, Hupel T, Payson L-A. Unnecessary ordering of magnetic resonance imaging of the knee: A retrospective chart review of referrals to orthopedic surgeons. PLOS ONE. 2020;15(11):e0241645. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0241645
Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. https://www.bmj.com/content/357/bmj.j1982.full.pdf
Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care & Research. 2020. https://www.arthritis.org/getmedia/d57cf9f5-e096-43a2-832d-dbc174065a58/Kolasinski-2020-american-college-of-rheumatology-a.pdf
Sword Health. How outcome pricing aligns costs with measurable results. https://swordhealth.com/newsroom/outcome-pricing
Peikes D, Dale SB, Ghosh A, et al. The Comprehensive Primary Care Plus Model and Health Care Spending, Service Use, and Quality. JAMA. 2023. https://jamanetwork.com/journals/jama/fullarticle/2813197
Risk Strategies Consulting (hosted by Sword Health). Cut MSK costs with predictive care: Risk report. https://swordhealth.com/reports-and-guides/risk-strategies-consulting-analysis
Sword Health. Transparent, Outcome-Based Pricing in healthcare. https://swordhealth.com/value/fair-pricing