August 27, 2025 • min read
Employer’s guide to pelvic health benefits
Written by

Evidence-based healthcare insights
Almost no one talks about pelvic health at work, yet its impact quietly shows up on every health plan balance sheet.
From missed meetings to rising surgery claims, conditions like urinary incontinence, pelvic pain, and prolapse drain billions in productivity and medical spend each year.¹ Still, most benefit plans have limited specific offerings in this area. That gap is increasingly expensive as women now represent nearly half the labor force.
Forward-thinking employers and benefits plan managers are shifting course and turning pelvic health from an oversight to a top healthcare priority. This change is overdue, and now there are discrete and scalable solutions available to help women eradicate pelvic pain and manage pelvic health conditions from home.
This guide will help you understand how to build pelvic health management options into an employee benefits plan to help women bring their best self to the workplace.
The silent pelvic health cost employers can’t ignore
Pelvic-floor dysfunction (PFD) affects roughly 40-50 % of post-menopausal women and one in three women overall.² ³ Those numbers scale quickly inside large populations. A 10,000-employee company likely has 1,600 workers coping with pelvic conditions like leakage, prolapse, or chronic pelvic pain.
The personal toll is steep for women with PFDs. A 2023 JAMA Network Open paper⁴ reports that women with pelvic floor disorders are 3.6 times more likely to experience depression, which clearly has a debilitating impact on their life and their work.
The costs of PFDs are hidden but significant
Employers pay higher direct costs for patient claims related to specialist visits, imaging, and pelvic floor surgeries that can average $30,000 per case⁵. Indirect costs are often left uncalculated, but women affected by pelvic health conditions face real difficulties at work when symptoms develop. Pelvic pain and related symptoms can force schedule changes, last-minute PTO, or talent attrition. This is especially important for women working during prime leadership years.³
Employers are realizing that pelvic healthcare benefits are not a niche consideration. So many women are affected, and support in this area can be an inexpensive way to attract and retain elite female employees.
Menopause amplifies the risk (and spend) for pelvic health conditions
Twenty percent of the U.S. workforce, or approximately 27 million people, are in some stage of menopause.⁶ Estrogen decline weakens pelvic tissue, leading to an increased incidence of incontinence problems, urgency, and prolapse rates. The prevalence of pelvic floor issues among women going through menopause is staggering:
- One in five women has quit or considered leaving a job because of symptom severity⁷
- Total productivity loss related to menopause tops $150 billion annually⁷
- 61% of affected women never seek care⁸
- Women wait an average of 6.5 years before speaking with a clinician⁸
The barriers preventing women from seeking care are more expected. Unfortunately, stigma is an issue. Geography, time, and a national shortage of pelvic health specialists are other important factors. The resulting unmanaged symptoms escalate, downstream claims rise, and employers foot the bill.
Meanwhile, women are left to suffer in silence with the pain of their condition, the impact on their quality of life, and the stress associated with managing their commitments at work.
It doesn’t have to be this way. Employers can offer accessible, discrete, digital care solutions, allowing them to recover from pelvic health issues from the comfort of their own home.
Digital pelvic care is a more accessible alternative
Traditional in-clinic pelvic physical therapy often works. But this doesn’t overcome the barriers preventing women from accessing care. Traditional therapy is only useful for the small proportion of women who can get to a clinic weekly, can afford to pay cash rates of $150-$300 per visit, and are prepared to overcome the discomfort of discussing intimate symptoms face-to-face.⁹
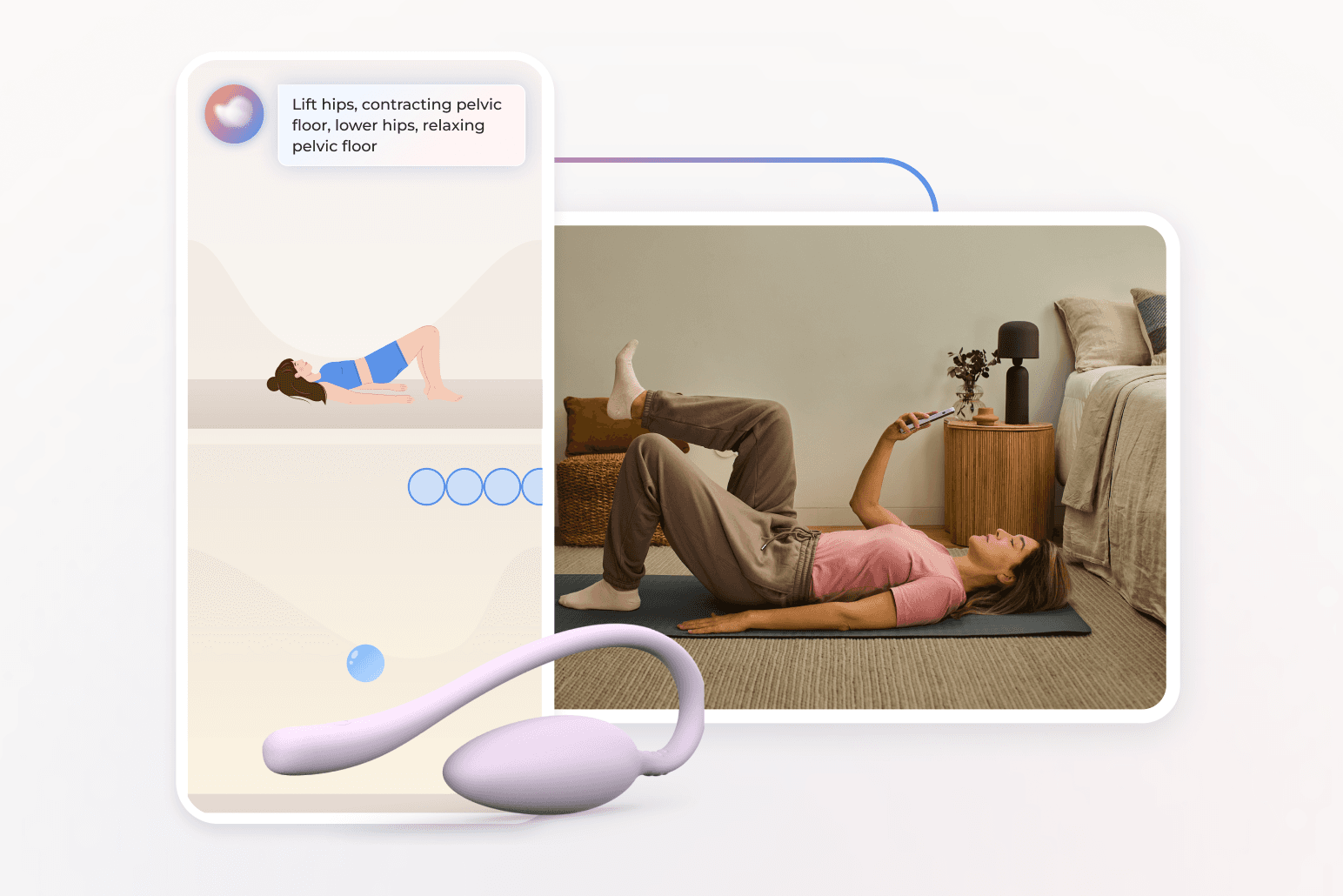
Digital pelvic care programs remove these hurdles, allowing women to access expert care at any time they like from a location of their choice. Sword Bloom offers digital pelvic care developed to solve these exact problems. Bloom makes it easy to get relief with expert-led care accessible from the comfort and privacy of home. With personalized exercises, real-time feedback, and a dedicated Pelvic Health Specialist, Bloom helps women at every life stage from adulthood, pregnancy, postpartum and menopause
How does Bloom work?
- Enrolled members are matched with a dedicated women's health specialist that holds a Doctor of Physical Therapy (DPT)
- Members meet virtually with their matched pelvic health specialist and get insights into their tailored program.
- The Bloom kit is shipped, including the Bloom Pod, which is then paired with the Sword Health app. Members use the app to access the personalized program prepared by their matched women's health specialist.
- Each workout is supported by the Sword app and the Biofeedback sensor inside the Bloom pod guides exercise form in real time.
- The PHS continuously monitors the program and adjusts the exercises planned as the member progresses.
- Members find relief from pelvic symptoms with a program tailored just for them, all from the comfort of home.
The Bloom pelvic health care model is flexible, private, and scalable across the United States, and various international markets. This accessibility and discretion of the from-home pelvic care model makes Bloom an ideal benefits plan addition for employer with dispersed or hybrid workforces.
Digital pelvic care isn’t just a solution to overcome the barriers to accessing treatment. The approach is effective, clinically credible, easy-to-use, and fiscally smart. An independent study of Sword Bloom members found an average of $5,203 in total healthcare savings per patient per year and a 2.9:1 gross ROI.¹⁰ Real-world data paints a compelling picture and the results speak for themselves.
Clinically-proven results
Bloom delivers life-changing pelvic care
69% feel better with Bloom
Nearly 7 in 10 Bloom members report feeling better or much better after care
67% find relief in just 9 sessions
Two-thirds of women with menstrual pain improved in under 10 Bloom sessions
9/10 member satisfaction score
Bloom members consistently rate their care experience among the highest in digital health
56% report improved workplace productivity
Bloom helps members feel better at work, boosting focus and reducing lost days
Pelvic healthcare benefits belong in a broader women’s health strategy
A single-point point solution rarely delivers lasting impact. Employers achieve the greatest value when pelvic health integrates with:
- Musculoskeletal (MSK) programs: Pelvic floor muscles are part of the core kinetic chain; coordinated MSK and pelvic benefits improve overall movement, pain, and function.
- Mental-health services: Depression and anxiety correlate strongly with bladder and bowel disorders.¹
- Pregnancy and postpartum care: Leakage and pelvic pain often begin or worsen after childbirth. Early digital intervention reduces surgical risk later.
- Menopause support: Addressing pelvic symptoms alongside vasomotor and cognitive changes keeps senior talent productive.
When these elements live in one platform, HR teams gain cleaner reporting, members get seamless navigation, and finance teams see additive cost control. Bloom's exceptional results show that digital pelvic care can deliver incredible health improvements for your members, while saving your downstream MSK costs:
- High engagement, low risk: a 3,051-member post-menopausal cohort completed digital pelvic therapy at a 77.6% rate with only 0.69% minor adverse events and average satisfaction of 8.6/10.²
- Meaningful symptom relief: 59.5% of participants hit the minimal clinically important change on the Pelvic Floor Impact Questionnaire.²
- Productivity rebound. work-productivity impairment fell 48%, and non-work activity impairment fell 55%.²
- Mental-health lift: among those starting with moderate to severe anxiety or depression, 76% and 54%, respectively, improved to a clinically meaningful degree.²
- Return on investment: Third-party claims analysis confirmed $5,203 annual savings and 2.9:1 ROI.¹⁰
Hidden productivity costs you can’t see in pelvic floor claims data
Claims related to pelvic floor conditions only uncover part of the total healthcare expenditure, and the related organizational costs. Consider:
- Micro-break loss: employees with urgency leave their desks up to 10 times more per day, reducing focused work blocks.
- Presenteeism drag: 62% of women with chronic pelvic pain report reduced on-the-job performance.³
- Leadership impact: symptom embarrassment prevents many high-potential women from pursuing promotions when their ability to work to their full potential is compromised
Digital pelvic care reduces the incidence of each factor, often within the first month, by giving women discreet recovery plans they can use at home, after hours, or on weekends. 50% of Bloom sessions occur outside 9–5, and 22% on weekends.¹¹
Mapping the ROI of pelvic health benefits
| Cost lever | Pre-intervention trend | Digital pelvic program impact |
|---|---|---|
Specialist visits, imaging, surgery | Rising year-over-year | ↓ $2,276 per patient in pelvic-related spend¹⁰ |
Absenteeism & presenteeism | Hidden but significant | 50% productivity gain after nine sessions¹⁰ |
For every $1 invested, employers can recoup nearly $3 in direct and indirect savings while elevating employee experience.¹⁰
6-step playbook for reducing pelvic healthcare costs
- Start with data: quantify female headcount by life stage to size the opportunity.
- Choose evidence-based vendors: look for FDA-listed sensors, peer-reviewed results, and doctoral-level clinicians.
- Bundle enrollment triggers: integrate pelvic onboarding into new-hire, maternity, menopause, and MSK pathways.
- Normalize the conversation: launch with manager toolkits and private Slack/Teams channels so employees can engage without shame.
- Measure what matters: track symptom scores, productivity surveys, and claims deltas quarter-over-quarter.
- Scale with incentives: tie completion rewards to broader wellness points to sustain engagement.
Stop pelvic pain with benefits women actively seek
The math is clear: pelvic health benefits slash spend, lift productivity, and support DEI goals by keeping women in the talent pipeline.
Reducing the incidence of pelvic care issues results in significant reductions in healthcare spend and the indirect costs associated with the impact of these conditions on women in the workplace. Download the Bloom ROI Whitepaper to see how top employers and health plans are slashing pelvic floor-related spend while improving access for your people:
End pelvic pain with Bloom’s discrete at-home care
Offer women life-changing support and slash claim costs driven by pelvic health conditions
Footnotes
Kołodyńska G et al. Menopause Rev. 2019.
Janela D et al. JMIR mHealth UHealth. 2025; e68242.
Scientific Reports. 2022;12:9878.
Yanamadala V et al. JAMA Netw Open. 2023;6(1):e2251214.
Lamin E et al. Int Urogynecol J. 2016;27(1):65–72.
Biote. Women in the Workplace Survey. 2022.
Faubion SS et al. Mayo Clin Proc. 2023;98(6):833–845.
Waetjen LE et al. Menopause. 2018;25(1):29–37.
Fraticelli T. PT Progress. 2019.
Sword Health. Bloom Pelvic Health ROI Whitepaper. 2025.
Sword Health. Bloom Impact on Health Equity Whitepaper. 2024.