February 20, 2026 • min read
Healthcare price transparency for payers: how to buy smarter
Learn how to use price transparency rules to compare healthcare vendors, avoid hidden fees, and pair transparency with outcome-based contracts, using MSK as the clearest example.
Written by

Evidence-based healthcare insights
Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Price transparency rules make negotiated rates and hospital charges more visible, but the data is only useful when it changes purchasing decisions.¹ ²
- For payers, the real unlock is pairing transparency with contracts that define what “success” means and what triggers payment.⁷
- MSK is one of the best categories to start with because variation is persistent, avoidable utilization is common, and outcomes can be measured at scale.³ ¹⁰
Why healthcare price transparency still feels frustrating for payers
Most health plan leaders agree with the intent behind healthcare price transparency: make prices visible so buyers can compare, negotiate, and stop overpaying.¹ ²
In practice, it often does not feel that clean. You get enormous machine-readable files, inconsistent formats, and prices that are hard to interpret without context.² ³ Providers define services differently and plans and vendors often define “episodes” differently. Even when you can see the rate, it is not always clear what it buys you. That is the core problem when transparency reveals prices, as it does not automatically reveal value.⁷ ⁸ ⁹
What “healthcare price transparency” includes
Healthcare price transparency in the US generally refers to two major rule sets.
- Hospital price transparency (CMS): Hospitals must publish standard charge information, including machine-readable files and shoppable services.¹
- Health plan price transparency (Transparency in Coverage): Plans and issuers publish machine-readable files with in-network rates and out-of-network allowed amounts and billed charges.²
These rules were designed to help the market work better. CMS explicitly anticipates that purchasers and third parties will process the data into tools and insights that make buying decisions easier.²
Why transparency alone does not fix costs
Research on transparency shows a consistent theme: visibility is necessary, but not sufficient.
A growing body of work shows wide price variation and useful market insights coming out of transparency data.⁷ At the same time, reviews of transparency interventions show mixed effects on overall spending because many transparency tools do not change incentives, clinical pathways, or contracting terms.⁸ ⁹
For payers, the implication is practical: if the contract still pays for volume, you can see the price, but you are still buying utilization. The missing link is a pricing model that makes “what we pay for” as clear as “what it costs.”
MSK is the clearest place to connect transparency to smarter purchasing
MSK is where price transparency becomes immediately relevant to payer economics.
MSK spend is large, it escalates fast, and it varies widely across markets and providers.³¹⁰ This is not just price variation. It is pathway variation: two members with similar symptoms can end up in completely different sequences of imaging, specialist visits, injections, or surgery. And once a member enters a higher-cost pathway, the costs are harder to unwind.
This is why MSK is a strong proving ground for transparent outcomes-based care: you can define outcomes, track improvement, and contract around what matters.
What “better buying” looks like: from transparent prices to transparent payment terms
Price transparency helps you ask sharper questions. Outcomes-based contracting helps you act on the answers. When you combine them, you move from “What is the negotiated rate?” to questions that help with accurate forecasting and added accountability:
- What is included versus billed separately?
- Are there activation fees, PMPM charges, or add-on costs?
- What triggers payment?
- What happens if members do not improve or do not engage?
- Can we audit outcomes and performance consistently?
This is where outcome-based pricing becomes useful. It turns transparency into a purchasing lever,.
How outcome-based pricing makes price transparency actionable
Outcome-based pricing ties a meaningful portion of payment to verified improvement measured using validated outcomes tools.⁷ ¹² For health plan and finance teams, this changes the financial signal:
- More predictable payment structure: Instead of claims volatility tied to service volume, payment is linked to defined milestones or outcomes triggers.
- Clearer accountability: If the member does not meet the outcome threshold, payment changes accordingly, based on the contract terms.
- Cleaner vendor comparison: When two MSK vendors both say “we improve outcomes,” outcome-based pricing forces comparable definitions: the measure, the threshold, and how success is counted.⁷
This is also where transparency helps with both procurement and governance. A transparent contract with auditable triggers is easier to defend internally than a model that relies on broad promises and opaque fee structures.
Sword leads the industry in outcome-based MSK pricing
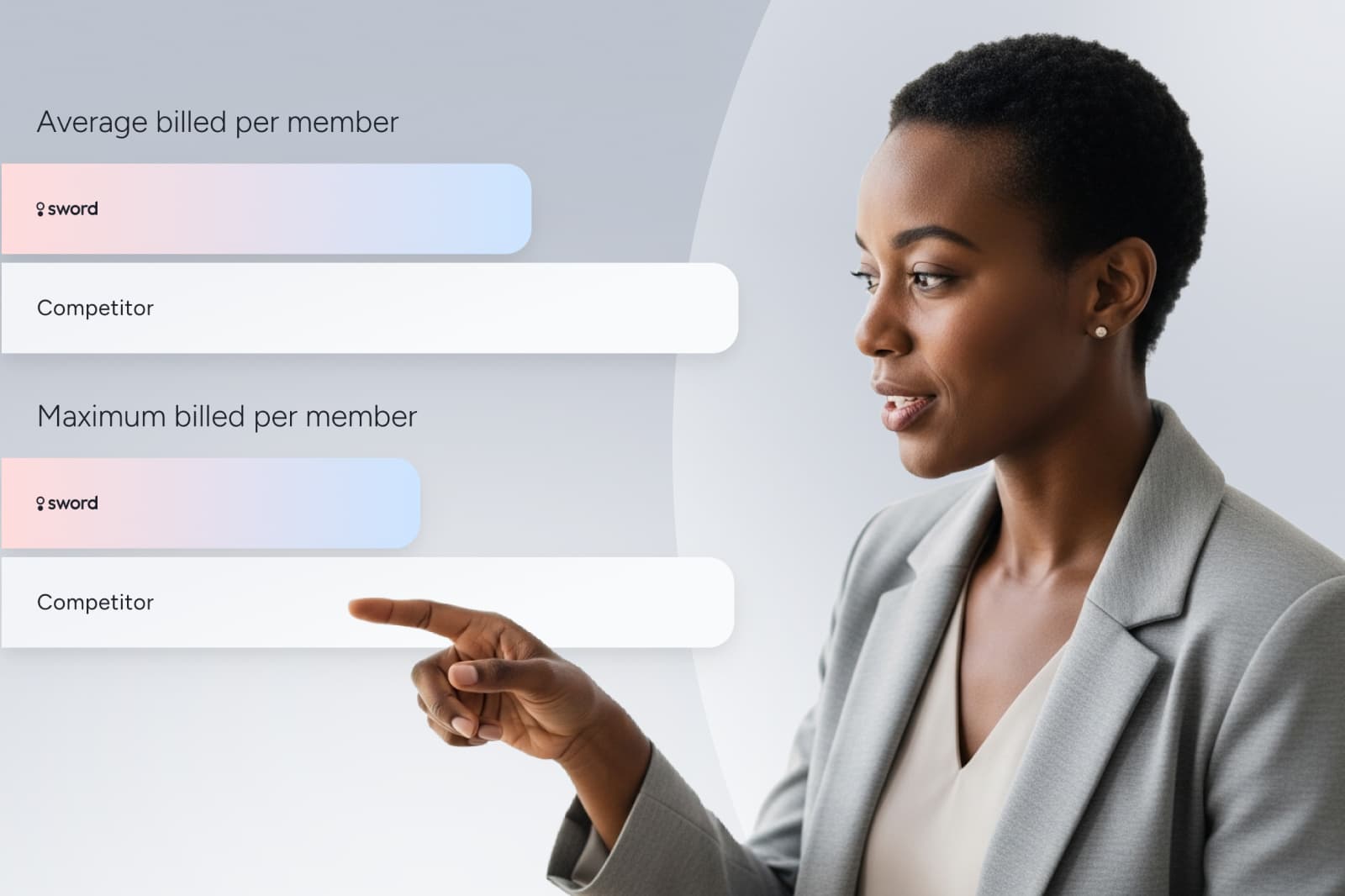
Outcome-based pricing is still rare in healthcare and was virtually absent in digital healthcare until 2024. Sword introduced outcome-based pricing to the industry, pioneering this contract structure where clients pay in full only when members achieve meaningful improvements. Simply, Sword's outcome-based pricing means we only get paid in full when the members hit measurable healthcare goals.
This approach realigns incentives to focus the vendor on providing quality care that drives measurable health improvements. Buyers know exactly what they are paying for and why.
How Sword’s outcome pricing works
- Payment is tied directly to clinical outcomes captured through validated measures.
- Outcome triggers are transparent and auditable.
- The model reflects Sword’s belief that payment should reward recovery, not utilization.
- Members can enroll in multiple programs with unlimited sessions.
- Payments are capped at $1,000 per member.
GUARANTEED SAVINGS
Get the industry's highest ROI and slash MSK spend with Sword
3.2x
Average ROI (the industry's highest independently-validated rate)
70%
reduction in surgery intent
41%
fewer ancillary services
10%
drop in MSK-related MRIs
35%
reduction in spine surgeries
A payer checklist for transparent MSK contracts
Before you commit to an MSK partner, the contract should make these items easy to answer.
Pricing clarity
- All fees and caps are clearly defined.
- Any add-on services and charges are explicitly listed.
Outcome clarity
- The outcome measure is validated and appropriate for MSK.
- The improvement threshold is defined in plain language.
- The handling of missing outcomes data is documented.
Audit and reporting
- Reporting cadence supports QBRs and forecasting.
- Outcomes and billing triggers are independently auditable.
Equity and access
- Eligibility and engagement strategies support broad populations.
- Terms discourage selection bias.
This checklist helps payer teams use transparency the way it was intended: to buy care with fewer surprises and more accountability.
Clearer purchasing needs transparency plus accountability
Healthcare price transparency is a step toward a more functional market. But it only changes outcomes when it changes what you buy and how you pay. In MSK, the combination is especially powerful:
- Transparency helps you see variation and pressure-test vendor claims.¹ ² ⁷
- Outcome-based pricing helps you connect payment to measurable improvement, so forecasting improves and “value” is not just a slogan.⁷ ¹²
If you are reviewing MSK contracts this year, a helpful next step is a short evaluation walkthrough focused on the mechanics:
- How outcomes are defined and measured
- What triggers payment and what does not
- What reporting looks like for finance, clinical, and consultant stakeholders
If you are considering a new MSK care provider to help you lower costs while still delivering better results, Sword has the industry's highest independently-validated ROI of 3.2x. ¹³
Sword pioneered Outcome Pricing in digital MSK, and we built it for the exact moment you’re in now: when “value-based” claims have to survive procurement, finance review, and renewal scrutiny. With independently validated ROI methodology and clear, auditable payment triggers, Sword gives you a straightforward way to pressure-test outcomes, compare models, and move forward with confidence instead of assumptions.⁶ ⁷
Set up a call with a Sword expert to see how Sword’s outcome-based pricing is structured and how it supports transparent, auditable MSK purchasing.¹ ² If you want to explore the model first, you can also review Sword’s transparent, outcome-based pricing before you jump on the call.
Start saving $3,177 per member per year
Slash MSK costs and get the industry’s top validated ROI of 3.2:1.
Footnotes
Centers for Medicare & Medicaid Services (CMS). Hospital Price Transparency Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/hospital-price-transparency-fact-sheet
Centers for Medicare & Medicaid Services (CMS). Use of Pricing Information Published under the Transparency in Coverage Final Rule. https://www.cms.gov/priorities/healthplan-price-transparency/overview/use-pricing-information-published-under-transparency-coverage-final-rule
Clark S, Horton R. Fee-for-service is not fit for purpose. Lancet. 2019;393(10188):2070-2071. https://doi.org/10.1016/S0140-6736(19)31252-1
Joynt Maddox KE, Orav EJ, Jha AK. Association Between Hospital Spending and 30-Day Mortality for Patients With Sepsis. JAMA Intern Med. 2017;177(1):62-68. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2589379
Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. Commonwealth Fund. 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits
Tseng P, Kaplan RS. Administrative Costs in the US Health Care System: The Forgotten but Significant Contributor to Total Spending. Health Affairs Forefront. 2020. https://www.healthaffairs.org/content/forefront/administrative-costs-us-health-care-system-forgotten-billions
Wang Y, Whaley CM, Bai G. Healthcare Price Transparency: Research Findings and Implications for Policy and Practice. Journal of General Internal Medicine. 2025;40:1175-1177. https://doi.org/10.1007/s11606-024-09295-4
Chen J, Miraldo M. The impact of hospital price and quality transparency tools on healthcare spending: a systematic review. Health Economics Review. 2022;12:62. https://doi.org/10.1186/s13561-022-00409-4
Hwang A, Anderson AC, et al. Outcomes of price transparency policies for healthcare services in the United States: a systematic review. The Lancet Regional Health - Americas. 2025. https://www.sciencedirect.com/science/article/abs/pii/S2211883725000012
Dartmouth Atlas Project. Trends and Regional Variation in Hip, Knee, and Shoulder Replacement. 2010. https://data.dartmouthatlas.org/downloads/reports/Joint_Replacement_0410.pdf
Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. https://www.bmj.com/content/bmj/357/bmj.j1982.full.pdf
Sword Health. How outcome pricing aligns costs with measurable results. Sep 10, 2024. https://swordhealth.com/newsroom/outcome-pricing
Sword Health. Cut MSK costs with predictive care: Risk report (Risk Strategies Consulting analysis). https://swordhealth.com/reports-and-guides/risk-strategies-consulting-analysis