February 19, 2026 • min read
Value-based contracting: 8-step healthcare buyer checklist
A practical guide to value-based contracting in healthcare to help you understand contract clauses that define outcomes, payment triggers, risk sharing, reporting, and audit rights.
Written by

Evidence-based healthcare insights
Value-based contracting in healthcare is the work of translating “value-based care contracts” into enforceable terms: outcome measures, risk sharing, reporting, and audit rights that protect plan sponsors and payers.¹ Most benefits leaders and plan executives already believe in the idea of value-based care.
The harder work is turning that belief into contract language that holds up if claims lag, when engagement drops, and when renewal becomes a high-stakes internal debate. If you are negotiating a new healthcare contract agreement, you can use this 8-step buyer checklist to understand how value-based care mechanics work in practice to separate them from any marketing claims from vendors.
Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Value-based payment aligns reimbursement with outcomes, quality, or efficiency rather than service volume.³
- Shared savings, bundled payments, capitation, and outcome-based pricing shift financial risk, cash flow timing, and accountability in different ways.³
- MSK is a strong proving ground because procedure rates vary widely, low-value utilization can still occur, and outcomes can be tracked at scale using validated measures.⁴ ⁵ ⁶ ⁷ ⁸
A value-based care contract should not require faith, it should create accountability you can verify, defend, and forecast.¹ ³
Use this guide to ensure you get that level of accountability for any prospective healthcare provider. It is a practical blueprint you can use in RFPs, renewals, and vendor negotiations, especially in MSK, where the difference between “value-based” in name and value-based in reality shows up fast.
What value-based contracting means
Value-based contracting is an agreement structure where payment is meaningfully linked to performance, such as outcomes, quality, or total cost impact, rather than only the volume of services delivered.¹²
In practice, this is less about buzzwords like “shared risk” and more about whether the contract answers a few simple questions in plain language:
- What counts as success, and how is it measured?
- What triggers payment, and what does not?
- What can the buyer verify independently?
- How is risk bounded so finance can forecast and governance can function?
If a contract cannot answer those questions clearly, it might still be called a value-based contract. Unfortunately, the service will likely not reflect this promise.
When “value-based” contracts still fail buyers in the real world
Most “value-based” failures are not philosophical, the problems are structural and they begin to manifest over time as results and return on investment doesn’t match up to the premise you were sold.
A pitch deck can promise outcomes and accountability. Then the contract quietly reverts to the same old pattern: vague measures, billing tied to activity, and reporting that cannot be audited. That is how buyers lose twice.
- They absorb cost for performance they cannot verify
- They lose internal confidence in value-based care as a strategy.³
Often, the result is a reversion back to a fee-for-service healthcare model without the same incentive to deliver quality over quantity.
Value-based contracts are also vulnerable to breakdown when they become overly complex or when measurement requirements create burden without clarity.³ If the contract creates confusion about what is being measured and what is being paid for, you risk losing some of the efficiencies and savings of value-based care, with excess paperwork and broken forecasting in return.
Common value-based care contract red flags to avoid
Some contract risks are easy to miss because they look like “standard operations” until the invoice arrives. Watch for the following common issues both before and after selecting a healthcare vendor and signing a contract:
- Hidden fees framed as enablement, implementation, platform, or reporting add-ons
- Outcomes defined after launch, or outcomes that shift based on vendor preference
- Payment tied to activity proxies like clinic visits or utilization rather than healthcare improvement
- Exclusions that remove high-need members and inflate apparent performance
- Reporting that cannot be audited, or reporting that arrives too late to support governance
If any of these are true, the buyer is left doing what fee-for-service has trained the system to do: pay first, ask questions later. For many teams, this is where healthcare price transparency becomes relevant. It can reveal what you pay, but the contract still has to make clear what you are paying for.
Value-based contract checklist: what to verify before you sign
This checklist is designed as a buying framework for the moment that matters most, when value-based intent meets legal language.
The goal is to make accountability easy to understand and hard to evade. If a vendor cannot meet these requirements, you are not being “too strict.” You are protecting your members, your budget, and your ability to lead the system toward contracts that reward recovery instead of volume.
1. Clarify scope, population, and eligibility
Before you negotiate outcomes, lock in who counts. In value-based contracting, the population definition becomes the foundation of every performance claim. Your contract should specify:
- The eligible population and any exclusions, with rationale
- Attribution rules, including when responsibility starts and ends
- How mid-year eligibility changes are handled
- How multiple MSK pathways are handled, including acute, chronic, pre-surgical, and post-surgical
If eligibility is vague, everything downstream becomes negotiable. That is how contracts drift from accountability into debate.
2. Understand how outcomes are measured
Outcomes are where a value-based contract becomes real. This is not the place to compromise on clarity because outcomes shape payment, governance, and vendor comparisons.
Your contract should include:
- The specific outcome instrument(s) used, named explicitly
- The improvement threshold that defines “success”
- The timing window for baseline and follow-up measurement
- Clear handling of missing data, including nonresponse, drop-off, and incomplete assessments
A simple test: if your team cannot explain the measure, threshold, and timing to a skeptical stakeholder in under a minute, you will struggle to defend results at renewal.
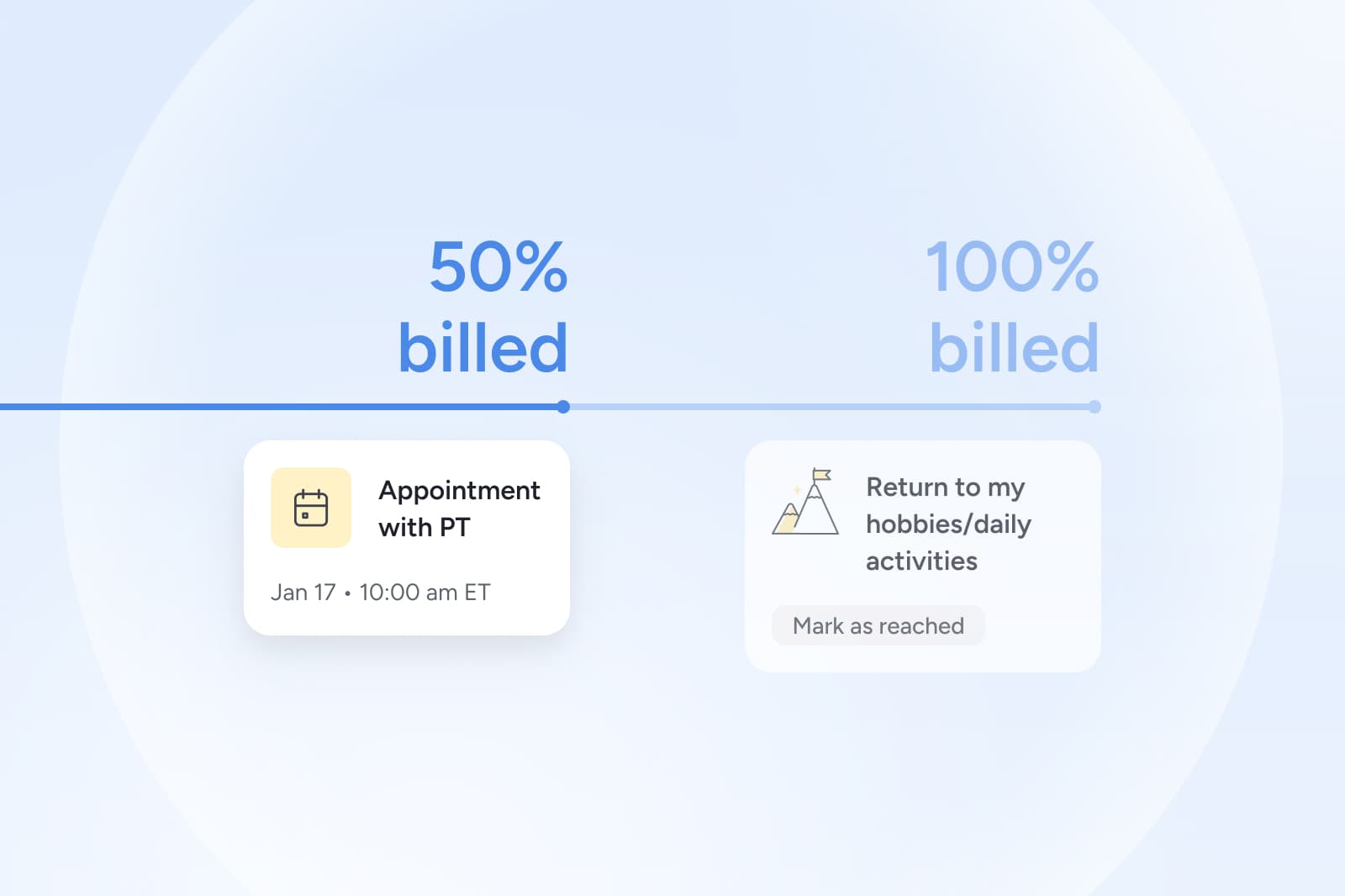
3. Payment mechanics and billing triggers
Payment triggers are where value-based contracting either protects the buyer or quietly recreates fee-for-service. An effective value-based care agreement should define:
- What triggers payment, including outcomes-based triggers where applicable
- What does not trigger payment, stated explicitly
- Invoice timing and required documentation for billing
- Rules for disputes and reconciliation
Finance teams need billing logic that produces predictable signals. This means stronger accountability, more accurate forecasting, cleaner reporting, and fewer surprises.
Validated savings and an auditable measurement system will make return on investment clear for both parties.
4. Risk sharing and bounded exposure
Risk sharing should feel balanced. It should motivate quality healthcare performance without turning your contract into an uncontrolled exposure event. Your agreement should spell out:
- The portion of fees at risk and how it is calculated
- Caps per member or per contract year
- Risk corridors or other guardrails that bound downside
- Change control clauses for benefit design shifts, eligibility shifts, and methodology changes
A contract can be tough and fair at the same time. Bounded downside and clear change control are what make risk-sharing sustainable.
5. Total cost of care, savings, and a shared source of truth
Cost conversations fall apart when both sides are “right” because they are using different definitions. Your contract should make that impossible by defining:
- What is included in total cost of care, by service category
- The baseline and comparison method, including runout assumptions
- Reconciliation timing and how lag is handled
- Whether savings are used for reporting only or tied to payment
When the source of truth is defined upfront, your ABRs and QBRs become decision meetings, not spreadsheet debates.
6. How data sharing, reporting, and audit rights work
If you cannot verify performance, you cannot govern it. Audit rights are not meant to be aggressive or time-consuming, but they are a prerequisite for buyer confidence. You should expect robust tracking and analysis. Hold your vendors to set expectations on:
- Reporting cadence, with monthly operational updates and quarterly governance views
- Minimum report contents, including enrollment, outcome completion, outcomes, and utilization signals
- Audit rights with process, timelines, and permitted reviewers
- Documentation standards and data retention expectations
- A clear dispute process tied to billing triggers and performance reporting
This is the clause that protects you when the conversation shifts from what we believe to what we can prove.
7. Implementation and operational lift
Implementation is where well-intended value-based deals can stall. The contract should protect you from accidental operational overload by specifying:
- Implementation timeline and dependencies
- Required data feeds and responsible parties
- Service-level expectations for issues and escalations
- Governance structure and QBR expectations
A buyer-friendly value-based care contract makes rollout predictable. That predictability is what enables adoption, measurement, and long-term value.
8. Renewal protections and change control
Value-based contracts can erode over time if terms drift at renewal or if definitions change midstream. Protect against this drift with:
- Mutual agreement requirements for measure changes and methodology changes
- Clear rules for pricing changes and what triggers renegotiation
- Performance remediation steps and termination for cause if accountability cannot be verified
Renewal should be a maturation of what the contract already proved. You want to avoid a situation where you are walking into a renewal to overhaul your agreement. If you have concerns or problems during a contract cycle, you should address them immediately.
How value-based contracting becomes operational
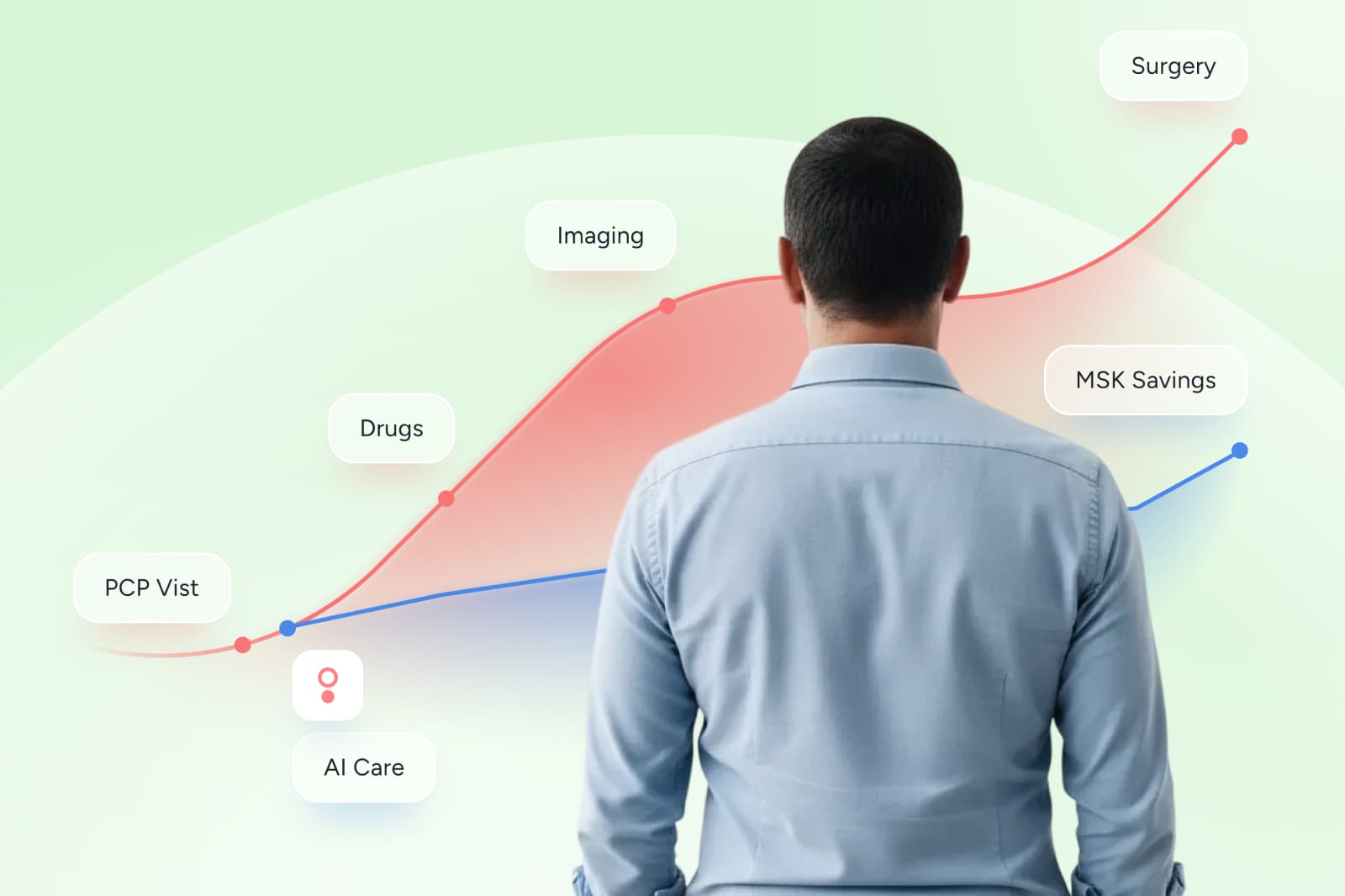
Musculoskeletal care is where value-based contracting stops being theory and becomes a system-level decision.
MSK spend is large, emotionally visible to members, and operationally visible to payers. It is also a category where low-value patterns persist across settings, which makes incentives and contract terms so much more than administrative details.⁴ That is why MSK is a proving ground for better contracting. When outcomes are measurable and pathways are variable, buyers have a real opportunity to reshape how care is purchased.
Outcome-based pricing can be one of the clearest structures in MSK contracting because it makes the unit of purchase the outcome, not the visit. Sword Health’s Outcome Pricing is designed around transparent triggers and measurable improvement so buyers can see what payment is tied to and what can be verified in reporting.⁵ ⁶
If you are evaluating an MSK partner, the most useful question is not whether they claim outcomes, but whether they can show, in the contract, how improved outcomes changes what gets billed.
GUARANTEED SAVINGS
Get the industry's highest ROI and slash MSK spend with Sword
3.2x
Average ROI (the industry's highest independently-validated rate)
70%
reduction in surgery intent
41%
fewer ancillary services
10%
drop in MSK-related MRIs
35%
reduction in spine surgeries
Build a contract your finance team can trust
Value-based contracting works when the agreement is specific enough that two people, on different teams, can read it and reach the same conclusion about what gets paid and why.
That is also how system change happens. Every contract term is a choice about what healthcare rewards: volume or recovery, ambiguity or verification, noise or clarity. Buyers who insist on measurable outcomes, clear triggers, and audit-ready reporting are not just protecting budgets. They are helping pull the market toward care models that expand access and reward what matters.
If you are negotiating MSK contracts this year, request a demo that focuses on contract mechanics and reporting verification, not a feature tour. Ask to walk through outcome definitions, billing triggers, risk limits, and the reporting your team can audit for forecasting and governance.⁵ ⁶
Start saving $3,177 per member per year
Slash MSK costs and get the industry’s top validated ROI of 3.2x
Footnotes
Centers for Medicare & Medicaid Services (CMS). Health Care Payment Learning & Action Network (HCPLAN). https://www.cms.gov/priorities/innovation/health-care-payment-learning-and-action-network
Health Care Payment Learning & Action Network (HCP-LAN). Alternative Payment Model (APM) Framework. https://hcp-lan.org/apm-framework/
Boone C, Zink A, Wright BJ, Robicsek A. Value-Based Contracting in Clinical Care. JAMA Health Forum. 2024. https://jamanetwork.com/journals/jama-health-forum/fullarticle/2822685
Harris K, Lopera-Escobar A, Luscombe G, Ferreira P, Mesa-Castrillon C. Is low-value care for persistent musculoskeletal pain more common in rural than urban areas? A scoping review. BMC Health Services Research. 2025. https://link.springer.com/article/10.1186/s12913-024-12132-3
Sword Health. How outcome pricing aligns costs with measurable results. https://swordhealth.com/newsroom/outcome-pricing
Sword Health. Transparent, Outcome-Based Pricing for MSK Care (Fair Pricing). https://swordhealth.com/value/fair-pricing