December 5, 2025 • min read
Ovary pain after menopause: causes, guidance, and support
Learn why ovary pain after menopause happens, what causes ovary-like pain, and how to understand and manage pelvic discomfort.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- True ovary pain after menopause can occur but is less common, because the ovaries become smaller and less active after the menstrual cycle ends².
- Many sensations that feel like ovary pain often come from nearby areas, such as the pelvic floor muscles, bladder, or bowel²,³.
- Once a clinician rules out ovarian or medical causes, pelvic care can help women understand and manage ongoing discomfort safely and confidently.
Why pelvic aches after menopause feel like ovary pain
Many women expect pelvic discomfort to ease once periods stop, so when an ache or pressure appears deep in the pelvis, it can feel confusing or alarming. Because the sensation is internal, many women assume it is coming from the ovary.
It helps to know that after menopause, the ovaries become smaller, less hormonally active, and less likely to generate pain². At the same time, other pelvic structures remain active, and they can all create sensations that mimic ovary pain. The bladder, bowel, pelvic floor muscles, and ligaments sit very close together.
When any of these become irritated, the discomfort can radiate or feel like it comes from the ovary region. Understanding how this small space works can help you feel more confident as you navigate these new sensations.
5 common causes of ovary-like pain after menopause

Below are the most frequent explanations clinicians see in postmenopausal women.
1. Postmenopausal ovarian cysts
Although cysts are more common before menopause, they can still form later in life¹. A cyst is a small fluid-filled sac that may cause pressure or a dull ache, usually on one side. Because cysts after menopause require monitoring, a clinician may recommend an ultrasound.
2. Pelvic floor muscle tension
Pelvic floor tension is a frequent cause of deep pelvic discomfort. These muscles support the bladder, bowel, and pelvic organs. After menopause, hormonal changes and daily habits can lead to tightness or reduced coordination²,³. When these muscles tense, the sensation can feel like ovary pain because the muscles sit so close to the reproductive organs.
3. Bladder irritation
Menopause often affects bladder function and sensation². Even mild bladder irritation or urgency can cause cramping or pressure that women perceive as ovary pain simply because of how close the bladder sits to the ovaries.
4. Bowel changes
Constipation, gas, and bloating are common during and after menopause². Because the bowel sits next to the ovary, digestive discomfort often feels like it originates from the reproductive system.
5. Pelvic organ prolapse
As tissues lose elasticity with age and hormonal changes, pelvic organs may shift downward. Research shows that pelvic organ prolapse affects up to 50 percent of women to some degree, with higher prevalence during and after menopause². This can create heaviness, pressure, or aching in the lower abdomen.
Other causes of ovary pain
Less common reasons include hernias, nerve irritation, or inflammation in the bowel. A clinician can help determine whether imaging or additional testing is needed.
Is the pain really coming from your ovary, or somewhere else?
True ovary pain is possible after menopause, but it is less common because the ovaries are no longer active in the way they were earlier in life². When ovarian pain does occur, it usually relates to something a clinician should check, such as a cyst or a benign growth¹.
More often, the discomfort is linked to other pelvic structures. Research shows that pelvic floor dysfunction affects 1 in 3 women, causing tension, weakness, and pressure³. These symptoms can feel almost identical to ovarian discomfort. Bladder and bowel changes, which are also common in menopausal women², can create similar sensations.
A clinician can help determine the source, but noticing patterns can give you helpful clues. Here are a few signs the sensation may not be coming from the ovary:
- The discomfort improves or worsens with movement, sitting, or stress
- The pain eases after a bowel movement
- You feel pressure or urgency linked to your bladder
- The ache spreads across the pelvis instead of staying on one side
- The feeling comes and goes instead of staying steady
These patterns often point to pelvic floor tension, digestive changes, or bladder irritation. A clinician can help confirm the cause, but these clues give you a helpful starting point.
How Bloom helps women manage pelvic pain after menopause
If your clinician has ruled out medical causes for your ovary-like pain, the next step is often understanding what your pelvic muscles and tissues need to feel supported again. Many women discover that the discomfort they feel is linked to pelvic floor tension, weakness, or changes in support structures, not the ovaries themselves. This is where Bloom, a digital pelvic care program by Sword Health, can help.
Bloom gives women a simple way to understand their pelvic symptoms, build confidence in their bodies, and gently support the muscles that help them feel more comfortable day to day. Everything happens privately at home, on your schedule.
What is Bloom and who does it help?
Bloom is a digital pelvic care program available through the Sword Health app. It is designed for women in every life stage, including menopause, who want clear, supportive guidance for symptoms such as bladder leakage, pelvic pressure, pelvic floor dysfunction, or ongoing pelvic discomfort.
Every member is paired with a dedicated Women’s Health Specialist holding a Doctor of Physical Therapy degree. This clinician becomes your guide, helping you understand your symptoms and adjusting your plan as your comfort improves.
Based on your needs, your Specialist builds a plan designed to calm tight muscles, support weak areas, and improve how your pelvic floor responds throughout the day. Your personalized plan may include:
- gentle strengthening for stability
- relaxation and breathing techniques to calm tension
- posture and pressure-management strategies
- education about what triggers your symptoms
Bloom begins with a conversation. Your Women’s Health Specialist learns about your symptoms, your daily routines, and how menopause has affected your comfort. Many women find this step reassuring because someone finally listens to their pelvic concerns with warmth and expertise.
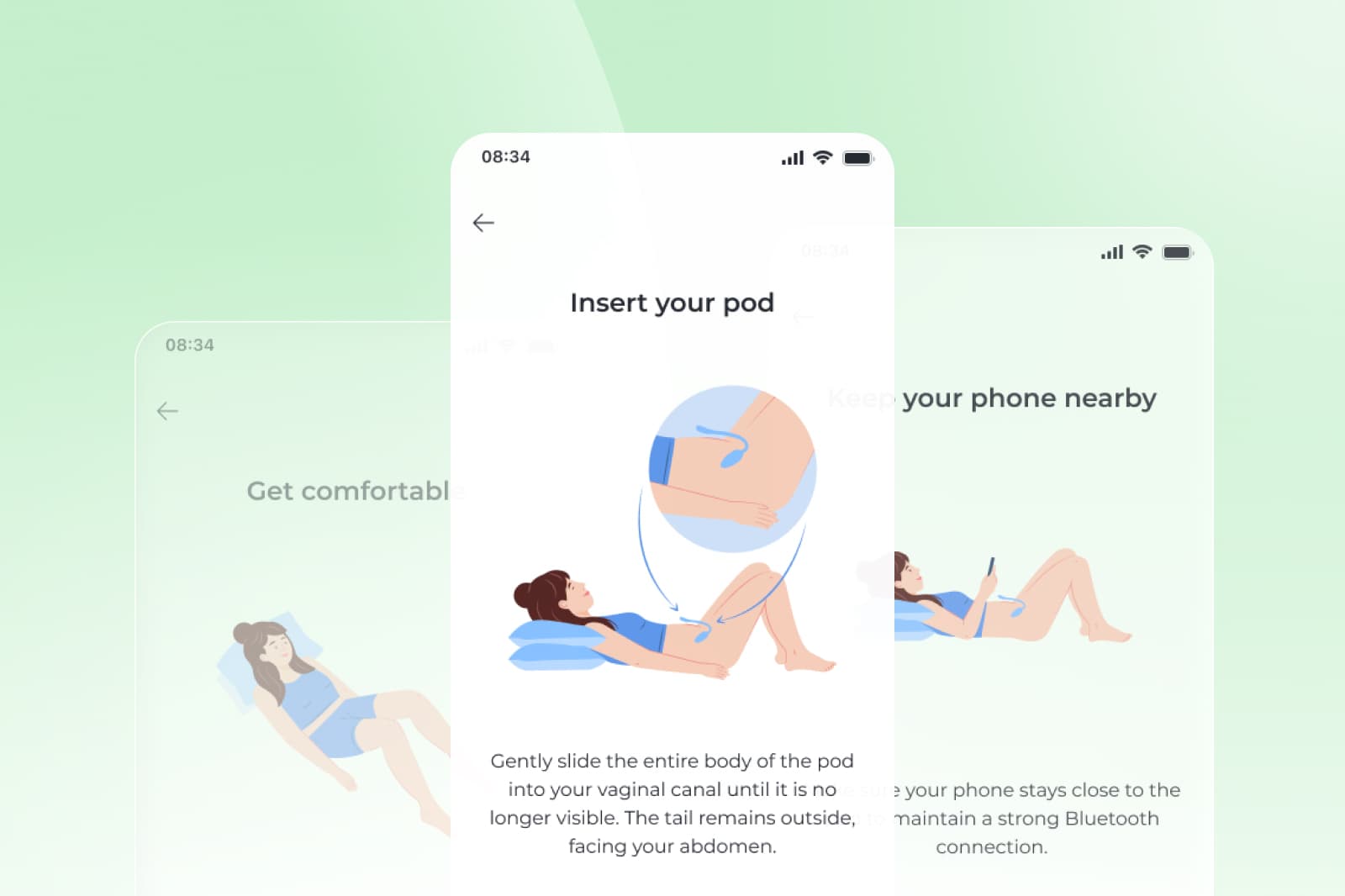
Most sessions take 10–15 minutes and can be done at your convenience. If recommended, you may also use the Bloom Pod, a small FDA-listed device that helps you see how your pelvic muscles engage. Many women say the real-time feedback makes the process feel easier and more intuitive.
Get started with Sword Bloom in 4 easy steps
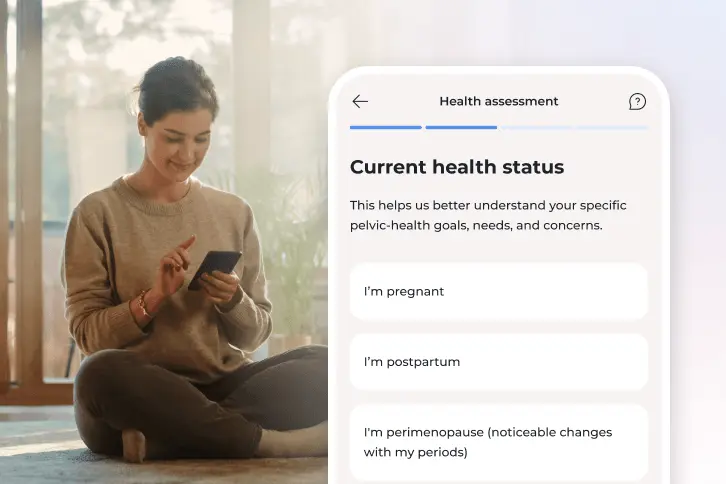
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Bloom is designed for women experiencing pelvic pain and discomfort, including symptoms like:
- pelvic floor dysfunction³
- bladder or bowel changes²
- pelvic pressure or tension
- lingering discomfort not tied to a medical condition
Women with ovary-like pain often learn that their discomfort is linked to pelvic floor tension, weakness, or support changes and issues that affect a significant portion of menopausal women²,³. For women in this situation, Bloom is proven to be effective in managing and reducing symptoms within weeks.
A note for women with ovary-like pain
Bloom is not designed to diagnose or treat ovary pain or medical conditions. New or persistent ovary-like pain should always be evaluated by a clinician first. Once serious causes are ruled out, Bloom can be a helpful next step for managing ongoing pelvic tension or discomfort.
How to tell what’s causing your pelvic discomfort
The pelvis can be tricky because many types of discomfort feel nearly identical. These simple observations may help point you toward the likely cause:
Look at what affects the discomfort
- Worse with sitting, lifting, or stress: Often linked to pelvic floor tension²,³
- Worse with a full bladder: May relate to bladder irritation²
- Better after a bowel movement: Often digestive or muscular
- Steady, one-sided pressure: Needs medical evaluation¹
Notice the type of sensation
- Sharp or pinpointed: Often muscle or nerve-related
- Dull or heavy: May relate to pelvic floor tension or prolapse²
- Sudden or severe: Requires prompt medical assessment
Track patterns and keep a brief symptom log can help you and your clinician see connections between activities, stress, digestion, and discomfort. These are not diagnostic tools, but they help you better understand your body and provide valuable information to your clinician.
When to get medical guidance for postmenopausal pelvic pain
It is always appropriate to check in with a clinician if you notice:
- New or persistent pain
- One-sided discomfort
- Bloating, nausea, or appetite changes
- Unexpected spotting or bleeding
- New bladder or bowel symptoms
- Fever or sudden worsening
Why pelvic discomfort can linger after menopause
Even after medical causes are ruled out, discomfort can continue. This is often due to changes that occur naturally during menopause. Declining estrogen affects the pelvic floor muscles, tissues, and nerves². These shifts can lead to increased tension, reduced coordination, or changes in the way the bladder and bowel interact with surrounding muscles.
Some everyday habits can also contribute to and agitate your pain, so try to avoid prolonged sitting, straining during bowel movements, or tightening the abdomen during stress. These types of discomfort are real but often respond well to pelvic care and education.
Remember, you don't have to accept pelvic pain or discomfort and suffer in silence. You have multiple options to help you overcome these symptoms and get back to living your day-to-day without having to deal with that nagging frustration. Options like Bloom can help, and you can always consult a medical professional for help with more severe symptoms.

Clear next steps to manage your ovary pain
If you are experiencing ovary-like pain after menopause, here is a simple approach that can help:
Step 1: Get clarity on the cause of your pain
A clinician can help identify whether your discomfort is coming from your ovary or another nearby area. This step often brings peace of mind.
Step 2: Notice the patterns of your symptoms
Pay attention to what makes the sensation better or worse. These clues can help guide your care and support.
Step 3: Work on your pelvic floor strength
If your pain is confirmed to be related to issues with your ovaries, your doctor will advise you on how best to treat and manage your symptoms. If your pain subsides, and once medical concerns are ruled out, gentle pelvic care can help reduce tension, improve muscle coordination, and support your comfort during menopause and beyond.
If Bloom is available through your employer or health plan, it can help you understand your symptoms, feel more in control of your pelvic health, and build more comfort in your daily life.
Many leading US health plans and employers provide access to Bloom programs at $0 cost to you. Check to see if your insurer already offers Bloom and you could get started right away.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Royal College of Obstetricians and Gynaecologists. Ovarian Cysts in Postmenopausal Women. Green-top Guideline No. 34. 2016. https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/ovarian-cysts-in-postmenopausal-women-green-top-guideline-no-34/
Chelsea and Westminster Hospital NHS Foundation Trust. Post-menopausal ovarian cysts: Information for patients. https://www.chelwest.nhs.uk/your-visit/patient-leaflets/womens-services/post-menopausal-ovarian-cysts-information-for-patients
Faubion SS, et al. Menopause: unexpected symptoms catch women by surprise. Mayo Clinic, 2023. https://mcpress.mayoclinic.org/menopause/menopause-unexpected-symptoms-catch-women-by-surprise/
Science Reports. Pelvic floor dysfunction prevalence and characteristics. 2022;12:9878.https://doi.org/10.1038/s41598-022-13501-w
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi