October 27, 2025 • min read
How to access pelvic floor dysfunction treatment at home
Stop accepting your symptoms and use this guide to learn how you can recover from leaking, discomfort, and pain from the comfort of home with expert support.
Written by

Head of Clinical Affairs, Sword Bloom
You don't have to suffer in silence with pelvic floor issues
Pelvic floor dysfunction affects millions of women, yet most go untreated or wait years to find care.¹ ² Symptoms such as pelvic pain, leakage, or pressure can be distressing, but they are not inevitable.
With new digital tools, women can now access pelvic floor dysfunction treatment at home, guided by licensed experts and supported by clinical data. From-home women's health care programs like Bloom by Sword Health offer private, effective therapy designed to help women heal comfortably, confidently, and on their own schedule.

What is pelvic floor dysfunction and why does it happen?
The pelvic floor is a network of muscles that supports the bladder, bowel, and reproductive organs. These muscles are essential for stability, posture, and everyday functions such as urination, bowel movements, and sexual activity. When the pelvic muscles become weak, tight, or uncoordinated, it leads to pelvic floor dysfunction, a condition that can cause discomfort, pain, and loss of control.³
Pelvic floor dysfunction can develop for many reasons. Pregnancy and childbirth place significant strain on the pelvic muscles. Hormonal changes during menopause reduce muscle tone and elasticity. Chronic constipation, pelvic surgery, and long hours of sitting can also weaken or tighten the pelvic muscles.⁴ ⁵
Research shows that one in three women in the United States will experience pelvic floor dysfunction in her lifetime.⁶ Despite this, many women delay seeking treatment because they assume symptoms are an unavoidable part of aging or postpartum recovery. They are not. Pelvic floor dysfunction is treatable, and recovery is often easier and faster than most women expect.
What are the common symptoms of pelvic floor dysfunction?
Pelvic floor dysfunction can appear differently for each woman, but the most common symptoms include:
- Leaking urine when sneezing, laughing, or exercising
- Difficulty controlling or holding urine
- Constipation or pain during bowel movements
- A feeling of pelvic heaviness or pressure
- Pain during intercourse
- Ongoing pelvic, hip, or lower back pain
These symptoms are disruptive but also highly treatable.⁷ They are signals that the pelvic floor muscles are out of sync and need gentle retraining to function properly again.
What causes pelvic floor dysfunction?
The pelvic floor can be affected by physical, hormonal, and lifestyle factors.
Common causes of pelvic floor dysfunction include:
- Pregnancy and childbirth: Stretching and delivery place pressure on the pelvic muscles and nerves.⁵
- Menopause: Lower estrogen levels can lead to muscle weakness and tissue thinning.⁸
- Chronic straining: Repeated heavy lifting or constipation can overwork muscles.⁴
- Pelvic surgery or trauma: Procedures such as hysterectomy or C-section may disrupt pelvic coordination.⁴
- Posture and stress: Constant tension in the body often translates into pelvic muscle tightness.⁹
Pelvic floor dysfunction is rarely caused by one issue alone. The condition is multifactorial, which is why effective treatment combines physical therapy, education, and behavioral support.¹⁰
How is pelvic floor dysfunction treated?
The standard of care is pelvic floor physical therapy, a specialized form of therapy that retrains the muscles responsible for support and control.¹¹
Treatment typically includes:
- Targeted exercises to strengthen or relax specific pelvic muscles
- Biofeedback to monitor muscle contractions and improve coordination
- Breathing and posture techniques to improve alignment and reduce strain
- Manual therapy to release tightness or pain
- Lifestyle and habit coaching to support bladder and bowel health
These methods help restore control, relieve pain, and rebuild confidence. Many women report feeling stronger and more in tune with their bodies after completing therapy.¹¹
Why pelvic floor dysfunction treatment at home is so much easier
Despite its proven benefits, pelvic floor therapy can be difficult to access. In the U.S., there is only one pelvic health therapist for every 10,000 women,¹² leaving long wait times and significant travel burdens. Privacy concerns and busy schedules add further barriers, especially for mothers and caregivers.
At-home treatment provides a solution. Digital pelvic health programs make therapy accessible, flexible, and discreet. Women can complete guided sessions at home, supported remotely by licensed pelvic health specialists.
The benefits of at-home care:
- Privacy: Therapy happens in the comfort of home.
- Flexibility: Sessions can be completed before or after work, or on weekends.
- Access: Women in rural or underserved areas can reach experts without travel.
- Consistency: Flexible scheduling encourages regular participation, which improves results.¹³
At-home pelvic therapy empowers women to take control of their recovery, combining comfort with clinical precision.
How does at-home pelvic floor therapy actually work?
Modern digital therapy programs bring the structure of in-person care into the home through connected technology and professional support. The leading example is Bloom by Sword Health, a digital pelvic health program designed to help women recover safely, privately, and effectively.
How the Bloom program works
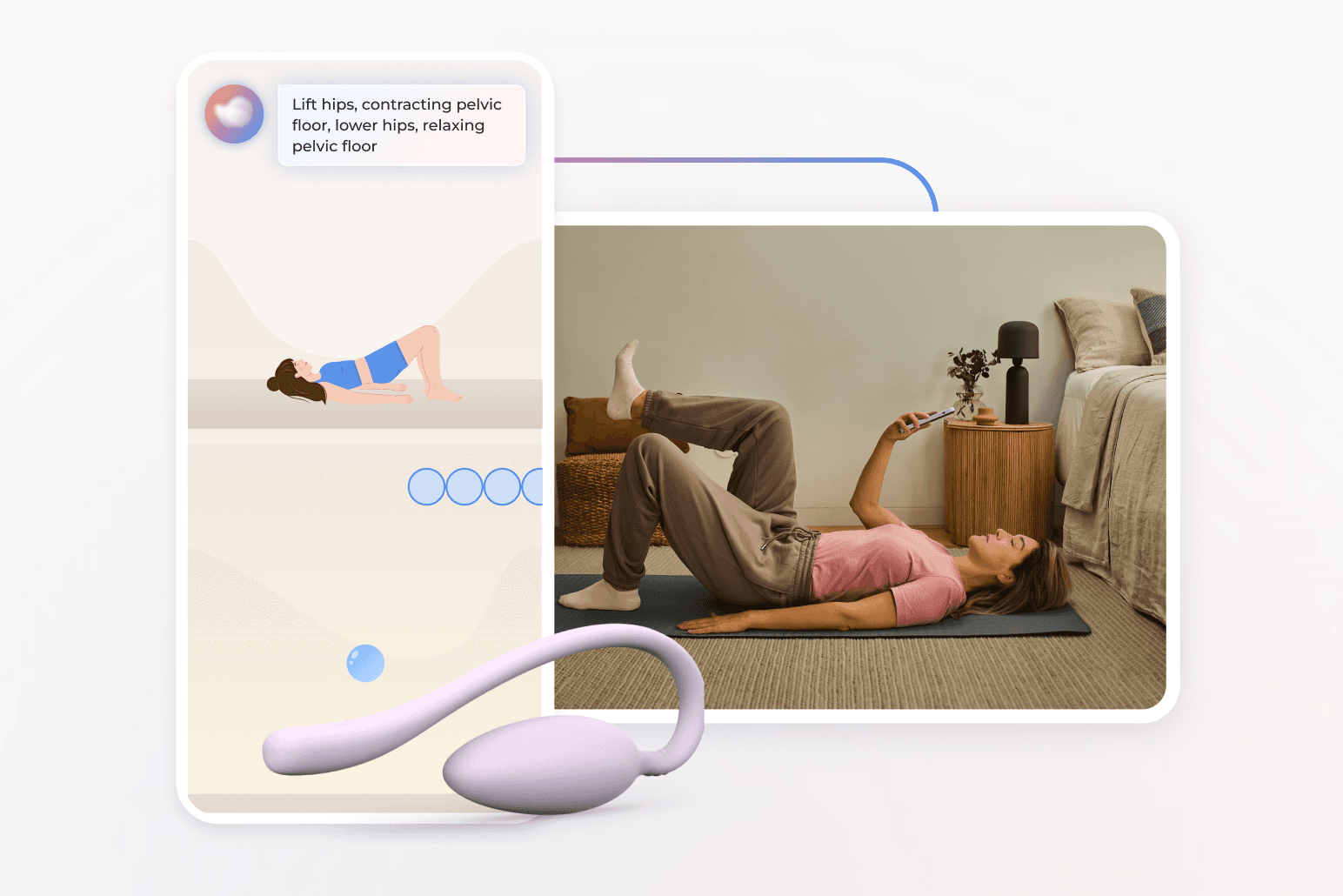
Bloom starts with a detailed clinical intake that identifies each member’s symptoms, health history, and personal goals. Every woman is then paired with a Woman's Health Specialist (who also carries a Doctor of Physical Therapy) who designs an individualized care plan. Members receive the Bloom Pod, an FDA-listed device that measures pelvic floor muscle activity. Using the Sword app, women complete short, guided sessions at home. The Pod provides real-time biofeedback, allowing users to see and understand how their muscles are working.
Throughout treatment, the specialist monitors progress, adjusts exercises, and provides education and encouragement through secure messaging or video calls. The experience mirrors in-person therapy but is more accessible and private.
Get started with Sword Bloom in 4 easy steps
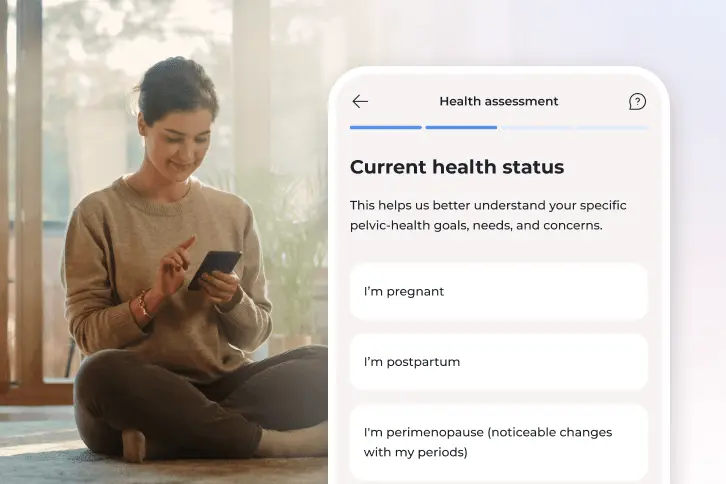
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Why Bloom is so effective compared to alternatives
Bloom combines clinical rigor with real-world flexibility. Traditional therapy often requires weeks of travel, time off work, and out-of-pocket costs. Bloom removes those barriers while maintaining medical-grade supervision.
Clinical outcomes show Bloom's strong results:
- 61 percent of women with moderate-to-severe pelvic floor dysfunction experienced meaningful improvement.¹⁴
- 76 percent reported reduced anxiety, and 54 percent saw improvement in depression symptoms.¹⁴
- Productivity impairment decreased by nearly 50 percent.¹⁴
- Half of all sessions take place outside normal working hours, and 20 percent occur on weekends.¹⁵
Bloom’s combination of privacy, flexibility, and professional oversight makes it one of the most accessible and effective pelvic care options available.
Reclaim comfort and confidence with Bloom
If you are dealing with pelvic discomfort, pain, or leakage, you do not have to manage it alone. Pelvic therapy can help you rebuild strength, control, and comfort, and with Bloom, you can do it discreetly and effectively from home. Recovery is guided by licensed specialists, supported by real data, and designed for your life and schedule. It is care that meets you where you are, helping you move forward with confidence.
Are you already be covered for Bloom's personalized care programs by your employer or health insurer? Check your coverage today (you may be able to get started today at $0 cost to you).
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Nygaard IE, et al. Prevalence of symptomatic pelvic floor disorders in U.S. women. JAMA. 2008;300(11):1311–1316. https://doi.org/10.1001/jama.300.11.1311
Margolis JS, et al. Care-seeking delay and symptom burden in women with pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2021;27(7):e482–e488. https://doi.org/10.1097/SPV.0000000000001135
Bø K, et al. Evidence-based physical therapy for the pelvic floor. J Physiother. 2019;65(2):67–75.
Low LK, et al. Pelvic floor disorders after childbirth: a systematic review. Obstet Gynecol. 2014;123(2 Pt 1):276–287.
Chen J, et al. Hormonal and neuromuscular changes associated with menopausal pelvic floor dysfunction. Front Public Health. 2025;12:1495679.
Kenne K, et al. Sci Rep. 2022;12:9878. https://doi.org/10.1038/s41598-022-13501-w
Stenzl A, et al. EAU Guidelines on Urinary Incontinence in Adults. Eur Urol. 2024;85(3):387–403.
Kavvadias T, et al. The link between posture, stress, and pelvic floor dysfunction. Phys Ther Rev. 2022;27(5):307–314.
Cochrane Incontinence Group. Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654.
Dumoulin C, et al. Pelvic floor muscle training vs no treatment: updated systematic review. Cochrane Database Syst Rev. 2023;12:CD005654.
Sword Health. Bloom Health Equity Whitepaper. 2024. https://swordhealth.com/insights/reports-and-guides/bloom-health-equity
Janela D, et al. Healthcare. 2024;12(2):141. https://www.mdpi.com/2227-9032/12/2/141
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Sword Health. Bloom Book of Business. 2023.