August 27, 2025 • min read
Pelvic floor therapy: what every HR leader should know
Written by

Head of Clinical Affairs, Sword Bloom
Most benefit leaders never see pelvic floor therapy on a renewal worksheet. Yet bladder leaks, pelvic pain, and organ prolapse affect one in three women and up to half of all post-menopausal employees.¹ ²
Women wait an average of 6.5 years before asking for help.³ During that gap they often lose sleep, skip key meetings, and, in severe cases, are even forced to walk away from promising careers.
Ignoring the problem costs money. Claims for specialist visits and surgery can top $30,000 per case.⁴ Presenteeism drives hidden loss that finance teams rarely capture. Employers that hope to retain female talent need a plan, not a pad stipend. Pelvic floor therapy is the ideal addition to any benefits plan to better support women in the workplace to be able to bring their best self to their job.
What is pelvic floor therapy?
Pelvic floor therapy uses targeted muscle training plus education and behavior change. Traditional pelvic floor therapy cna involve a pelvic health specialist teaching a patient to contract and relax deep core muscles, then guides progression of these pelvic florr exercises to help the patient recover. Typical goals achievable with pelvic health care include:
- Reduce urinary or bowel leakage
- Ease prolapse pressure
- Lessen chronic pelvic pain
- Improve core stability and sexual comfort
Exercises are brief. Many take ten minutes, three or four times each week. Consistency outweighs intensity, which makes the delivery channel critically important.
Understanding the mechanics is the first step, but access and program adherence determine whether pelvic floor care makes a lasting impact.
In-clinic pelvic therapy works but many women don’t access this care
Traditional pelvic floor physical therapy happens in a treatment room. The therapist performs an internal exam, sets up a biofeedback device, and coaches technique. Outcomes are solid, with response rates near sixty percent in the literature.⁵ Access, however, is limited. Only about one pelvic therapist exists for every ten-thousand U.S. women.⁶
Clinics cluster in major metro areas. Visits cost USD 150 to 300 out of pocket. Busy professionals struggle to carve two hours for commute, waiting room, and session. These barriers are why many women never start or finish treatment, and why new, more flexible care models are gaining traction.
Digital pelvic care uses the same scientific approach at a larger scale
Digital programs keep the evidence-based core and shift delivery to the member’s phone. Each kit includes a medical-grade intravaginal sensor that streams real-time contraction data. A doctoral-level pelvic health specialist reviews progress, adjusts the plan, and messages the member inside a secure app.
Meet Bloom, Sword Health’s digital pelvic therapy program
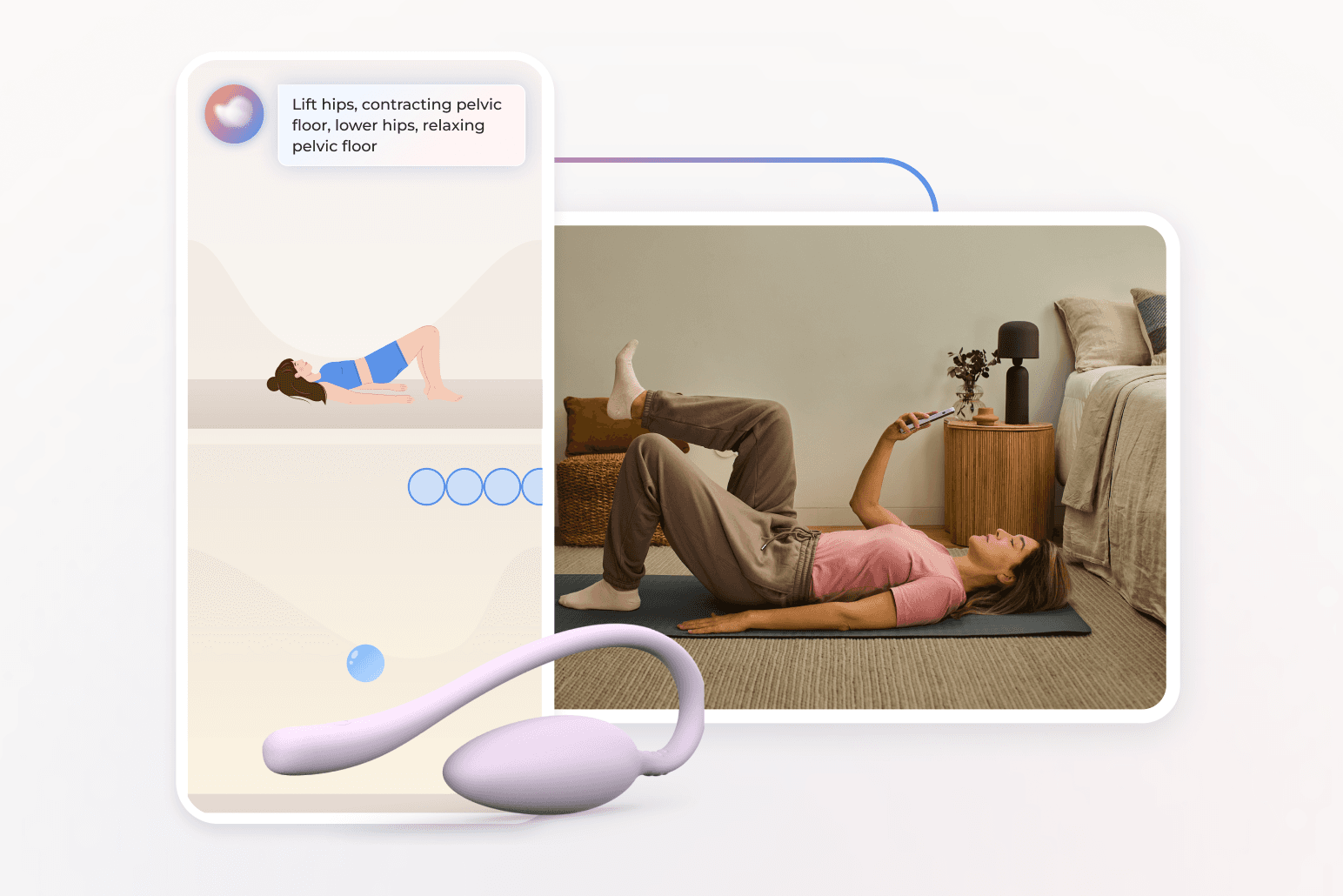
Bloom pairs its FDA-listed Bloom Pod with a smartphone app that guides ten-minute exercise sessions and records muscle activity. Each member is matched with a Pelvic Health Specialist who holds a Doctor of Physical Therapy degree. The clinician reviews data inside a secure portal, sends coaching feedback, and adjusts difficulty as the member progresses. Artificial intelligence flags adherence gaps and suggests content so therapists can focus on higher-value guidance.
For benefit plans this model delivers national reach, minimal hardware burden, and claims-validated savings of $2,276 per member per year with a 2.9:1 gross ROI.¹⁰ Members gain privacy and scheduling freedom, employers gain measurable cost control and stronger retention among female talent.
Bloom delivers a 2.9x ROI with expert pelvic floor care
These advantages are not just theoretical. Bloom’s sustained success has been validated in large-scale member populations and independent claims analyses.
When you look at the real-world data, the impact on both clinical outcomes and employer ROI becomes even clearer.
- 77.6 percent completion in a cohort of 3 051 post-menopausal members.⁹
- 59.5 percent hit a clinically meaningful drop in symptom burden.⁹
- Work-productivity impairment fell 48 percent.⁹
- Annual health-care savings averaged USD 2 276 per member.¹⁰
- Gross ROI 2.9:1 validated by Risk Strategies Consulting.¹⁰
- Sessions take ten to fifteen minutes. Half occur after standard work hours and one in five on weekends, proving flexibility.¹¹
Sessions take ten to fifteen minutes. Half occur after standard work hours and one in five on weekends, proving flexibility.¹²
These results are compelling, but many benefits teams still ask how the digital experience compares to traditional in-clinic pelvic floor therapy.
If you’re weighing pelvic floor therapy options,the digital-first model like Bloom delivers a level of accessibility, engagement, and cost control that is difficult for traditional care to match. When rehabilitation exercises are easier to start, more private, and available outside the 9–5 workday, more women stick with it. And that leads to stronger health outcomes and cost savings.
How pelvic floor therapy delivers strong ROI
The impact of pelvic floor therapy extends beyond symptom relief. The financial gains are significant and measurable fro employers and health plans, in the form of:
- Avoided surgery: digital therapy users recorded 148 fewer pelvic surgeries versus a matched control.¹⁰
- Lower emergency visits: symptom control reduces urgent-care trips.
- Fewer imaging claims: strength gains lower demand for follow-up scans.
- Productivity lift: after Bloom users reach nine sessions, productivity rises by fifty percent.¹¹
Add softer gains such as morale and leadership retention, and the value case grows stronger. When benefits leaders see the full picture, the business case is clear. Pelvic floor therapy is not just a women’s health benefit; it is a strategic investment in workforce stability, productivity, and cost control. Digital delivery removes barriers, ensures higher engagement, and extends care access to employees who would otherwise go untreated.
The message is simple: when you remove the friction from getting help, women recover faster, stay at work longer, and contribute at their highest level. Bloom gives your plan the scale, privacy, and proven results to make it happen.
Takeaway for HR leaders
Pelvic floor therapy addresses an overlooked driver of cost and turnover. Traditional PT helps but reaches few employees. Digital pelvic therapy keeps the science, removes friction, and scales nationwide. Bloom supplies clinician oversight, strong engagement, and clear ROI. Adding this benefit shows that your company supports women at any stage of their career and life. Now is the time to offer Bloom to help the women in your workforce overcome the pain and discomfort of pelvic floor dysfunction.
End pelvic pain with Bloom’s discrete at-home care
Offer women life-changing support and slash claim costs driven by pelvic health conditions
Footnotes
Janela D. et al. (2025). JMIR mHealth & uHealth.
Scientific Reports 12, 9878 (2022).
Waetjen L. et al. (2018). Menopause, 25(1), 29-37.
Fraticelli T. (2019). PT Progress blog.
Hagen S. et al. (2020). BMJ, 371, m3719.
American Physical Therapy Association. Workforce data, 2023.
Molina R. et al. (2024). Int J Gynecol Obstet.
Kołodyńska G. et al. (2019). Menopause Review.
Sword Health (2024). Bloom Impact on Health Equity Whitepaper.
Sword Health (2025). Bloom Pelvic Health ROI Whitepaper.
Sword Health (2024). Bloom Impact on Health Equity Whitepaper.