February 17, 2026 • min read
How to improve your pelvic health after menopause
Pelvic health after menopause can change over time. Learn what symptoms to watch for, what helps, and how to get support that fits your life.
Written by

Senior Clinical Program Manager, Sword Bloom ·
There is a quiet myth that menopause is the finish line. You made it through hot flashes, mood shifts, and sleep that felt like a revolving door, so now you are supposed to be “done.” But your pelvic health did not get the memo.
For many women or people with vaginal anatomy, postmenopause is when pelvic symptoms finally get loud enough to interrupt the day: the unexpected leak when you laugh, the heaviness that makes you sit down sooner, the dryness that turns intimacy into a negotiation, the constipation that seems to come out of nowhere.
None of this means something is “wrong” with you. It means your body is still adapting, and it still deserves support.
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Pelvic health after menopause is not “past tense.” Symptoms can appear or shift years later, especially genitourinary changes linked to lower estrogen.¹ ²
- Many postmenopausal pelvic symptoms are common and manageable, especially when support matches your body and your needs.¹
- A good plan is not “just Kegels.” It can include strength, relaxation, coordination, and practical habits that reduce day-to-day disruption.³
- Ongoing support can be simple, discreet, and if your health plan has coverage for Bloom's women's health AI Care plans, you can access a personalized program with 24/7 access from the comfort of home starting with a quick eligibility check.
Pelvic health after menopause still matters
Your pelvic health is part of how you move through the world. It shapes how you sleep, how you travel, how you exercise, and how confident you feel when you are far from the nearest bathroom.
After menopause, symptoms can also become more noticeable over time if they are not addressed, especially genitourinary symptoms related to estrogen changes.¹ ² That can feel confusing, because many people expect things to “settle down” after their last period.
A steadier frame is this: postmenopause is a new baseline. If a symptom is changing your routines, it deserves attention, even if it started quietly or developed gradually. You should not settle for discomfort or suffer in silence.
Why the pelvic floor changes postmenopause
The pelvic floor is a network of muscles and connective tissues that supports the bladder, bowel, and reproductive organs. It also plays a role in continence, pressure management, and comfort during intimacy.
After menopause, lower estrogen can affect tissues in and around the vagina, vulva, urethra, and bladder. This cluster is often discussed as genitourinary syndrome of menopause (GSM).¹ ² GSM is common, and it can progress without treatment, which is why symptoms may feel more persistent over time.¹ ²
Just as important, menopause is not the only influence. Your pelvic floor also reflects:
- Your health history (past pregnancy, birth, surgeries, athletics, heavy lifting)
- Any chronic patterns (constipation, straining, breath holding)
- Overall strength, mobility, and coordination changes with aging
So if symptoms show up “late,” it does not mean you missed your chance. You still have more than enough time to reduce and prevent symptoms from impacting your quality of life.
Postmenopause pelvic symptoms worth noticing, not ignoring

Many postmenopausal pelvic symptoms start small. They are easy to minimize until they quietly reshape routines.
Here is a simple rule that helps: if a symptom changes what you do, it deserves attention.
Common postmenopausal pelvic symptoms:
- Bladder changes: leaks with coughing or exercise, urgency, frequent urination, or a feeling you are not fully emptying
- Vaginal and vulvar changes: dryness, burning, irritation, or discomfort with intimacy (often discussed within GSM)¹ ²
- Bowel changes: constipation, straining, or difficulty fully emptying⁵
- Pelvic pressure or a bulge sensation, which can be a sign of prolapse⁴
- Recurrent urinary symptoms, especially alongside dryness or irritation (which can overlap with GSM)¹ ²
If you are reading this and thinking, “I thought this was just normal now,” you are not alone. But “common” and “inevitable” are not the same thing. You should take action and seek support to reduce your symptoms and get back to the best version of you.
Why the “just do Kegels” advice can backfire
A lot of women are offered one line of advice: do Kegel exercises and move on. The reality is more nuanced, especially after menopause. Pelvic floor muscles can be weak, but they can also be overactive, tense, or poorly coordinated. Some people need more strength. Others need better relaxation and timing first. Many need both, in a sequence that changes over time.
That is why pelvic floor muscle training is typically taught as a structured plan, not a vague reminder. In evidence reviews, pelvic floor muscle training is associated with meaningful improvement for urinary incontinence for many women.³
If you have tried Kegels and felt worse, more pressure, more urgency, or more discomfort, that is useful information. It is a sign to shift from guessing to guided, individualized support.
A 4-step postmenopause pelvic health routine to fits real life
“Lifelong pelvic health” does not mean long routines or thinking about your pelvic floor all day. It means a maintenance mindset, like brushing your teeth. Small habits, done consistently, protect comfort and confidence over time. Think of this as a menu, not a mandate.
1. Keep bowel habits gentle
Constipation is common as we age, and it can be influenced by diet, activity level, medical conditions, and medications. Straining can increase pelvic pressure, so bowel support is pelvic support.⁵ Simple supports to discuss with your clinician may include improving your hydration, fiber changes, increasing daily movement, and reviewing constipating medications.⁵
2. Build whole-body strength and pressure control
Your pelvic floor does not work alone. It coordinates with your diaphragm, deep core and trunk muscles, hips, and glutes. A few times a week, focus on strength that supports daily life: sit-to-stand, step-ups, carries, and breath-coordinated core work. Pay attention to your breathing during effort and try not to hold your breath. This can reduce unnecessary strain.

3. Use lubrication and moisturizers when vaginal dryness shows up
Dryness is not only about sex. It can affect sitting, walking, and even wiping after urination. Over-the-counter lubricants and moisturizers can help many people with mild symptoms. For more persistent GSM symptoms, clinicians may discuss prescription options such as low-dose vaginal estrogen or other therapies, depending on your health history and preferences.¹ ²
4. Do pelvic floor work that matches your specific symptoms and needs
If you want one takeaway, make it this: the right pelvic floor plan is specific to your symptoms and your body. For some, that includes strengthening. For others, it includes relaxation, lengthening, and coordination. For many, it is a blend that evolves. Guidance matters, especially after menopause when symptoms can shift rather than fade on their own.¹ ² ³
When to get extra support
Some pelvic symptoms are inconvenient but others are signals that you should escalate and get help from a doctor or expert clinician right away.
If any of the following are true, it is worth getting evaluated:
- A bulge or lump sensation in or around the vagina, or pelvic heaviness that is new or worsening⁴
- Leaking that limits exercise, travel, or sleep, or that is not improving with basic habits³
- Recurrent urinary symptoms, especially alongside vaginal dryness or irritation¹ ²
- Pain with intimacy, burning, or irritation that persists despite over-the-counter measures¹ ²
- Any bleeding after you have been without a period for more than 12 months, even spotting⁶
That last one is especially important. Postmenopausal bleeding is often not serious, but it should always be checked.⁶
Bloom is the ideal program to support your pelvic health after menopause

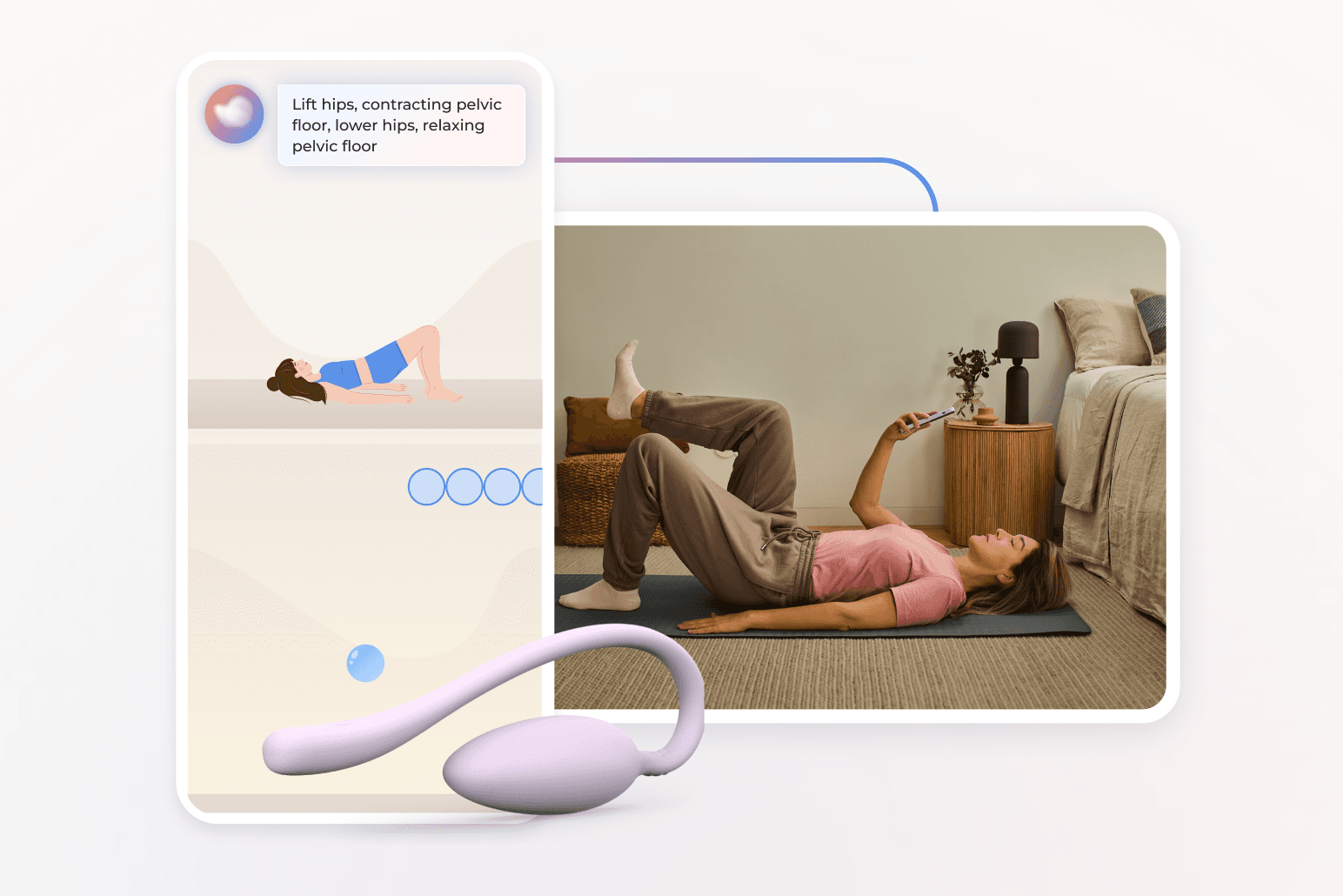
Bloom is a digital women’s health solution designed to support women in every life stage, including during and after menopause. Members are paired with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. Each member receives a personalized pelvic care plan through the Sword Health app. The program also includes an optional insertable Bloom Pod, an FDA-listed biofeedback sensor, which measures your muscle movement during your exercises and provides real-time feedback as you go.
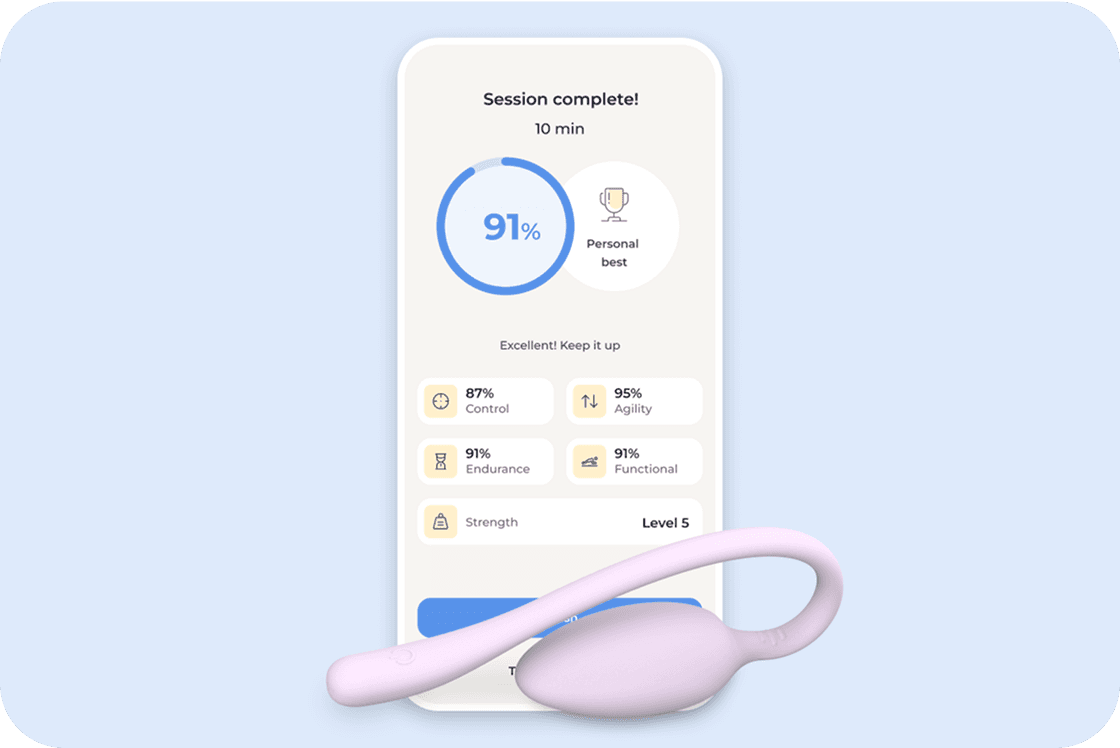
Each session lasts 10 to 15 minutes and fits easily into your day and your personalized program is updated by your care specialist as you progress to keep you adapting and improving. This specialist is also on hand to keep you accountable to your exercise plan, and to escalate your situation to a doctor if your symptoms warrant this action.
Bloom’s results speak for themselves:
- 65% of women report meaningful improvement in daily life¹⁵.
- 56% experience higher productivity and 50% report less anxiety¹⁵.
- 77% complete their program, exceeding typical in-person adherence rates¹⁶.
These outcomes show that consistent, guided pelvic care can reduce your symptoms, prevent discomfort, and rebuild your body confidence from the privacy of home. You get 24/7 access to your personalized care plan and direct support from your matched women's health expert through the Sword app.
Get started with Sword Bloom in 4 easy steps
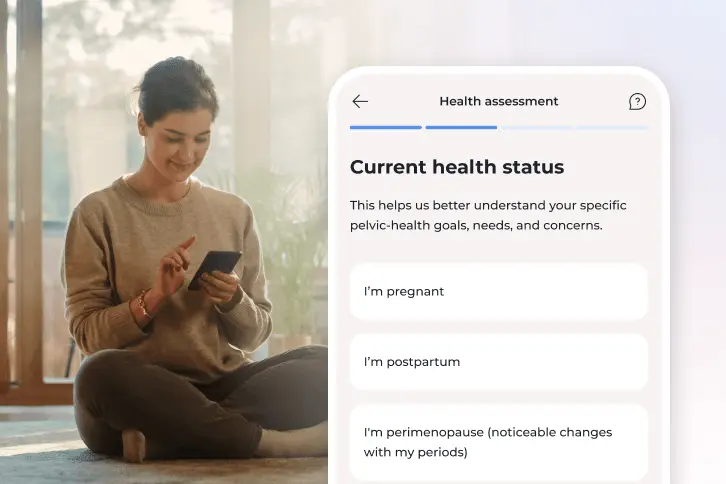
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
How to get started with Bloom
Many employers and health plans now include Bloom as a covered benefit¹¹. You may have already coverage within your health insurance to access personalized pelvic and musculoskeletal care at no cost to you.
Checking your eligibility is simple:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Menopause is a milestone, not the end
Postmenopause can be expansive. For many women, it is the first time in decades that life is not organized around cycles, caretaking intensity, or hormonal unpredictability.
You deserve to move through that freedom without bracing for leaks, discomfort, or pressure that makes you feel older than you are.
Pelvic health after menopause is not about “fixing” yourself. It is about staying connected to your body, so it can keep carrying you well. Don't settle for pain or discomfort. With the right support you can get back to your best and take back control of your body and your quality of life.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
The North American Menopause Society (NAMS). The 2020 genitourinary syndrome of menopause position statement. Menopause. 2020. https://www.isswsh.org/images/content/2020-NAMS-GSM-Paper.pdf
The Menopause Society. Genitourinary Syndrome of Menopause (MenoNote). https://menopause.org/wp-content/uploads/for-women/MenoNote-GSM.pdf
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training for urinary incontinence in women (Cochrane Review summary). https://www.cochrane.org/evidence/CD005654_pelvic-floor-muscle-training-urinary-incontinence-women
NHS. Pelvic organ prolapse. https://www.nhs.uk/conditions/pelvic-organ-prolapse/
National Institute on Aging. Concerned About Constipation? https://www.nia.nih.gov/health/constipation/concerned-about-constipation
NHS. Postmenopausal bleeding. https://www.nhs.uk/symptoms/post-menopausal-bleeding/