August 27, 2025 • min read
Reduce urinary incontinence leaks and avoid surgery
Treat urinary incontinence without surgery. Learn causes, proven therapies, and how digital pelvic care supports private, effective recovery.
Written by

Head of Clinical Affairs, Sword Bloom
Urinary incontinence (UI) is one of the most common yet underreported health challenges facing women today¹. The condition is too often cloaked in stigma and silence. Women should feel confident and empowered to seek health without any judgement, especially as the condition is so common. The harrowing impact of UI quietly disrupts lives, undermines workplace performance, and inflates healthcare costs². Resolving this issue can deliver genuinely life-changing improvements for women suffering with UI, and the financial imperative for employers and health insurance providers is significant³.
Thankfully, urinary incontinence treatment and recovery is possible without surgery. This guide will uncover what urinary incontinence is, the underlying causes, and the wide-ranging impacts on women, businesses, and healthcare plans. You’ll learn about proven, non-surgical treatment methods and how digital solutions are reshaping access to effective pelvic health management.
What is urinary incontinence?
Urinary incontinence is defined as the involuntary leakage of urine. It ranges from occasional small leaks triggered by coughing or sneezing, known as stress incontinence, to more frequent and unpredictable urgency incontinence⁵.
Who can suffer from urinary incontinence?
Contrary to common belief, urinary incontinence is not just an issue for elderly individuals. Approximately one in three adult women experience urinary incontinence at some point in their lives⁴. Prevalence notably increases with life events like pregnancy, childbirth, menopause, and hormonal changes⁵.
Common types of urinary incontinence
Urinary incontinence refers to a loss of bladder control, leading to unintentional urine leakage, but there are several types:
- Stress Incontinence: Leakage occurs during activities that increase pressure on the bladder, such as coughing, sneezing, laughing, or lifting heavy objects.
- Urge Incontinence: Sudden and intense urges to urinate that lead to involuntary leakage.
- Mixed Incontinence: Combines symptoms of both stress and urge incontinence.
How does urinary incontinence develop?
For many women, UI develops gradually due to a combination of anatomical, hormonal, and lifestyle factors. Major life stages such as pregnancy, childbirth, and menopause alter the strength and coordination of pelvic floor muscles⁷.
- Pregnancy and childbirth: The physical strain of pregnancy and delivery can weaken pelvic floor muscles, significantly increasing the risk of stress incontinence⁶.
- Menopause: Hormonal changes affect the strength and elasticity of pelvic tissues, leading to increased episodes of urinary leakage⁷.
- Surgical interventions: Procedures like hysterectomies can disrupt pelvic structures, increasing vulnerability to incontinence⁸.
- Chronic conditions: Obesity, diabetes, or neurological disorders can elevate risk by weakening pelvic muscles or altering bladder function⁹.
Understanding these triggers underscores the importance of early intervention and effective pelvic health management.
The hidden impact of UI on women and workplaces
The personal toll of UI extends beyond physical discomfort, deeply impacting emotional well-being and workplace productivity. Women suffering from UI are 3.6 times more likely to experience depression¹⁰.
Impact of UI on individuals
UI can affect women’s confidence, sense of control, and mental health¹³. Many women avoid physical activity or social outings, wear protective pads daily, and plan their days around restroom access¹³.
These changes often go unspoken but have a cumulative effect on wellbeing.
- Mental health: Women with UI are significantly more likely to experience anxiety and depression. Research shows a 3.6x higher incidence of depression compared to unaffected women⁵.
- Daily disruption: Fear of embarrassing episodes can limit participation in work meetings, travel, and social interactions, leading to isolation and reduced professional confidence.
Impact UI on work and productivity
These individual impacts cascade into significant organizational and economic consequences for employers.
UI leads to missed workdays, reduced focus, and absenteeism⁵. In a workforce of 10,000, more than 1,600 employees are likely struggling with UI-related symptoms that interfere with their roles⁴. These disruptions are rarely linked directly to incontinence on claims reports, but the hidden impact shows up in performance reviews, healthcare spend, and attrition.
- $2,916/year in lost productivity per MSK patient¹⁴
- More frequent and longer breaks during workdays¹³
- Opting out of advancement due to stigma or unaddressed symptoms¹³
Costs of UI to employers and insurers
- Direct medical costs: Imaging, consults, medications, and surgeries can average $30,000 per case in severe scenarios¹².
- Indirect costs: Absenteeism, presenteeism, turnover, and short-term disability claims silently inflate budgets³.
Addressing the stigma of UI: why women suffer in silence
Despite being common and treatable, UI is one of the most under-discussed health issues for women.
- Fewer than 30% of women with UI seek care⁴
- Even among those who see a provider, UI is often minimized or misdiagnosed¹³
- Many face 12+ week wait times for pelvic health specialists⁴
Urinary incontinence is heavily stigmatized, preventing many women from seeking help promptly. Cultural taboos, lack of awareness, and inadequate workplace support compound the problem, prolonging suffering and escalating costs. Only about half of women with UI ever discuss it with a healthcare provider, perpetuating a cycle of unmanaged health deterioration⁷.
Systemic UI care access barriers
- Long wait times for pelvic health specialists (up to 12+ weeks in many markets)⁷
- Limited provider availability in rural or underserved regions²
- Insurance hurdles and lack of awareness about coverage for pelvic floor therapy²
Employer blindspots
Many benefits leaders underestimate the scale or business impact of UI. It’s rarely listed in top claims, but it hides in:
- Gynecology and urology consults
- Mental health visits linked to chronic discomfort
- Surgical interventions for bladder repair or prolapse
Non-surgical treatment for urinary incontinence
Thankfully, many UI cases can be improved or resolved without surgery. Evidence shows urinary incontinence is highly treatable through non-surgical interventions, particularly pelvic floor muscle training (PFMT), behavioral strategies, and lifestyle modifications⁵.
Pelvic floor exercises: Proven to reduce or eliminate symptoms in 70% of stress incontinence cases¹⁴ when performed consistently by improving muscle coordination and reducing or eliminating leakage episodes⁵
Biofeedback training: Helps women accurately perform pelvic floor exercises, improving efficacy and adherence¹⁵.
Lifestyle adjustments: Managing fluid intake, bladder irritants, and weight¹⁵
These changes, combined with PFMT, can eliminate the need for surgical intervention. Despite proven effectiveness, these conservative treatments remain underutilized due to limited provider availability, discomfort with in-person sessions, and time-consuming clinic visits.
Pelvic floor muscle training (PFMT)
Often referred to as Kegels, PFMT is an effective option for UI treatment.
What is pelvic floor muscle training (PFMT)?
Pelvic floor muscle training (PFMT), commonly known as Kegels, involves repeated contraction and relaxation of the muscles that support the bladder, uterus, and bowel.
How PFMT works
These exercises help strengthen the pelvic floor, which can become weakened or imbalanced due to life events like childbirth, menopause, or surgery. A properly functioning pelvic floor plays a critical role in maintaining continence and preventing leakage.
- Muscle engagement: The exercises retrain the brain and muscles to engage properly, improving control over urination.
- Tissue strengthening: Strengthening pelvic muscles can better support pelvic organs and reduce pressure on the bladder.
- Improved coordination: Regular practice enhances the timing and coordination between the muscles and the bladder.
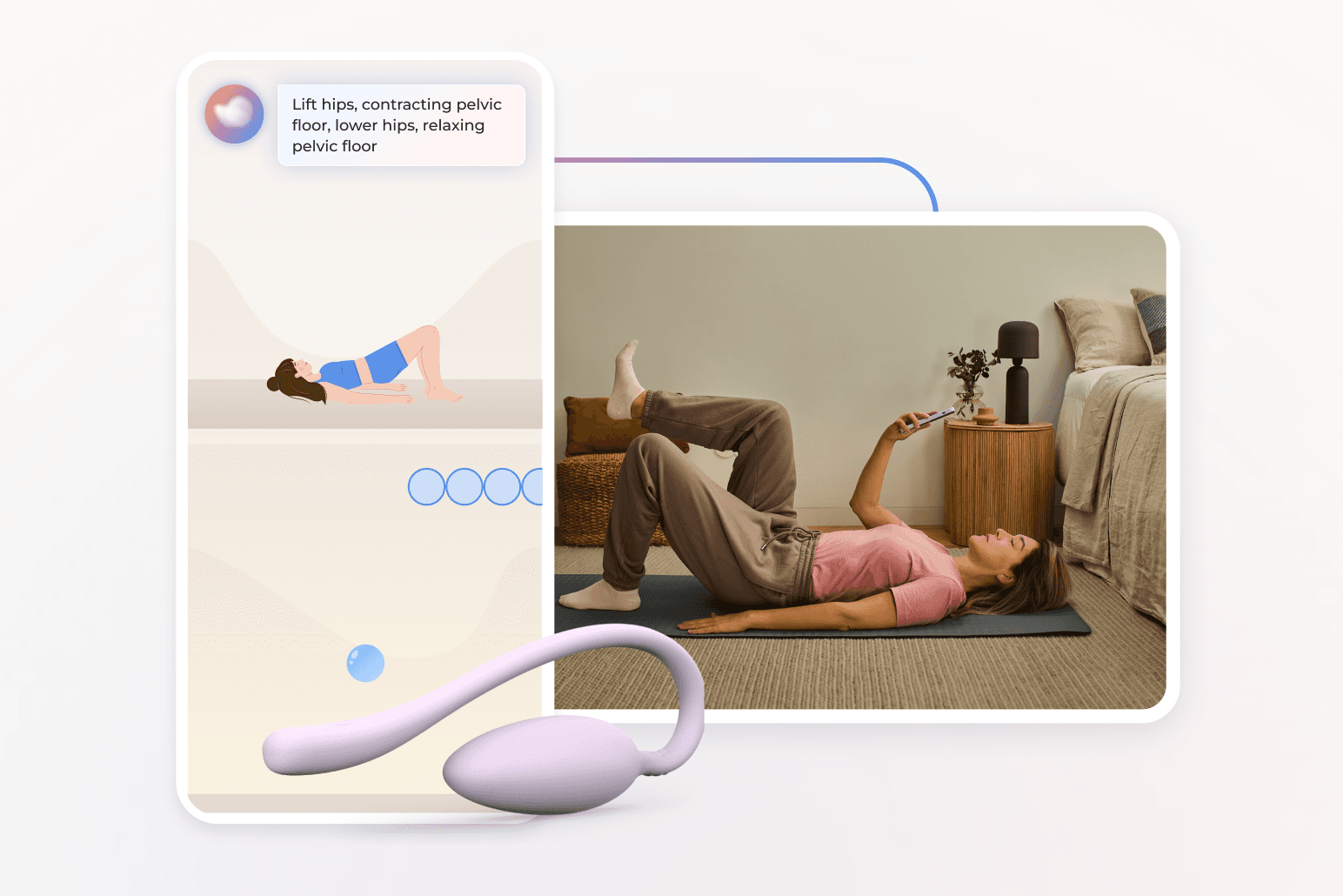
Digital biofeedback tools help guide users through exercises by providing visual or auditory cues to confirm whether the correct muscles are being engaged.
This is especially helpful since many women unknowingly contract the wrong muscle groups, reducing the efficacy of traditional Kegels.
One study found that 59.5% of women experienced a clinically meaningful improvement in symptoms when guided with Bloom’s PFMT program¹⁶.
Bloom is a digital-first solution for pelvic health at scale
Bloom by Sword Health is a clinically validated, virtual pelvic health program designed to deliver non-invasive, scalable, and stigma-free care directly to those who need it.
For employers and health plans, Bloom simplifies access and ensures outcomes, helping large populations manage urinary incontinence and related pelvic conditions with ease. What sets Bloom apart is its from-home digital delivery model, combined with the human touch of personalized support from a women's health care specialist. The program blends expert clinically-guided care with innovative biofeedback tools and real-time guidance, all inside on easy-to-use app. With Bloom, members can:
- Start care quickly without long wait times
- Work with a dedicated Doctor of Physical Therapy (DPT)
- Access discreet, guided PFMT programs anytime, anywhere
- Track their progress, get feedback, and adjust their care plan as needed
Critically, Bloom gives women the tools and expert guidance they need to learn proper muscle engagement and track progress. One study found that 59.5% of women reached a clinically meaningful improvement with PFMT as delivered through Bloom⁸.
Digital pelvic care is transforming urinary incontinence treatment
Digital care offers women a powerful alternative to traditional in-clinic care, which often presents logistical and emotional barriers.
Many women face difficulties traveling to a clinic, experience discomfort discussing deeply personal issues in public settings, or are unable to schedule appointments during working hours while balancing jobs and family responsibilities.
These barriers lead to delays or avoidance in seeking care. The consequences of this are catastrophic for the individual. This means prolonged symptoms, increased mental distress, and escalating pain. As the condition deteriorates, the requirements for eventual treatment are much more significant in terms of intervention and cost.
Traditional UI care challenges
Traditional, in-person pelvic health care has long been the default option, but it often creates substantial barriers to treatment. Many women avoid seeking care altogether, but even when a woman does get to the clinic, teh statistics show high drop-out rates from care plans.
- Low adherence: Up to 70% of women drop out of in-person pelvic PT programs¹⁷.
- Privacy concerns: Discussing and treating UI in clinical settings can feel invasive
- Inflexibility: Scheduling, transportation, and PTO needs limit access
The digital pelvic health care alternative
Digital pelvic health programs Bloom by Sword Health effectively overcome barriers traditionally associated with pelvic care:
- Accessibility: Bloom provides discreet, private access to clinically validated pelvic care from home, removing logistical barriers.
- Engagement and adherence: Guided biofeedback, personalized coaching, and regular virtual check-ins ensure higher completion and success rates than traditional in-person therapy.
- Clinical efficacy: Bloom’s virtual delivery consistently achieves clinical outcomes comparable or superior to in-person treatments.
Offer Bloom to help women reduce UI symptoms
Bloom is a virtual-first pelvic health program, created to remove the obstacles that keep women from getting care.
How Bloom works
- Women are matched with a Pelvic Health Specialist holding a Doctor of Physical Therapy degree
- They receive a personalized plan of guided PFMT, education, and real-time feedback
- Sessions take place at home, at their pace, in complete privacy
Bloom delivers proven results at scale
- 77.6% completion rate across thousands of users¹⁶
- 8.6 out of 10 satisfaction score¹⁶
- 0.69% adverse event rate, demonstrating excellent safety profile¹⁶
- Significant reductions in symptom burden, anxiety (76.1%), and depression (54.1%)¹⁶
Bloom also empowers employees in high–Social Deprivation Index (SDI) areas, lower-income brackets, and rural geographies. In fact, 27% of users come from socially deprived areas, and outcomes remain consistent across income and race⁵.
Implementing Bloom in your benefits strategy
Adding Bloom to your benefits plan is straightforward and high impact. You can get started fast as Sword's team manage a 4-step onboarding process within weeks.
- Plan analysis: Identify target populations most likely to benefit
- Outreach strategy: Educate eligible employees with engaging, stigma-free messaging
- Onboarding: Employees sign up via app and begin with a DPT-led evaluation
- Support: Bloom’s care team monitors progress, safety, and satisfaction
Ignoring urinary incontinence is no longer viable. Forward-thinking employers recognize that proactive pelvic health management is essential for employee wellness and sustainable healthcare costs. Integrating digital pelvic solutions like Bloom demonstrates leadership commitment to comprehensive employee health.
Learn how Bloom by Sword Health’s digital-first approach could help your plan members regain control discreetly, confidently, and cost-effectively. Set up a demo with a Bloom expert today.
Stop MSK care spend leaking away
Invest in the healthcare platform that predicts and prevents pain with guaranteed ROI
Footnotes
National Association for Continence. "Statistics and Facts." 2021.
Journal of Women’s Health. 2021;30(4):473–481.
Sword Health. Proven ROI Report. 2025.
Agency for Healthcare Research and Quality. "Definition & Types of Urinary Incontinence." 2022.
Waetjen LE et al. Menopause. 2018;25(1):29–37.
Handa VL et al. Am J Obstet Gynecol. 2011;205(5):456.e1–456.e6.
Faubion SS et al. Mayo Clin Proc. 2023;98(6):833–845.
Weber AM et al. Obstet Gynecol. 2000;95(7):1045–1052.
Subak LL et al. Obstet Gynecol. 2002;100(5 Pt 1):881–886.
Yanamadala V et al. JAMA Netw Open. 2023;6(1):e2251214.
Sword Health. Internal Population Modeling. 2024.
Lamin E et al. Int Urogynecol J. 2016;27(1):65–72.
Anger JT et al. J Urol. 2012;188(6):2268–2273.
Dumoulin C et al. Cochrane Database Syst Rev. 2018;10:CD005654.
Bø K et al. Br J Sports Med. 2015;49(7):457–463.
Janela D et al. J Med Internet Res. 2024;26:e68242.
Bø K et al. Br J Sports Med. 2017;51(7):493–494.