February 18, 2026 • min read
The cost of menopause that health plans cannot ignore
The cost of menopause shows up in claims, productivity, and retention. Learn where the spend concentrates, why pelvic symptoms matter, and what benefits leaders can do now.
Written by

Evidence-based healthcare insights
The Sword summary warm-up
Menopause costs do not show up as one neat line item, so they are easy to underestimate until they start hitting retention, productivity, and claims at the same time.
- Menopause affects nearly 20% of the U.S. workforce, and the estimated annual productivity loss tied to menopause-related symptoms is $150B.¹
- A large share of menopause’s workplace impact is driven by pelvic symptoms, including bladder and bowel issues that employees often do not disclose.¹ ²
- When you address pelvic symptoms with accessible, high-engagement pelvic care, you can reduce downstream utilization and create measurable ROI, including Bloom’s validated 2.9:1 gross ROI.³
 A benefits leader rarely hears the real reason someone leaves early for the day. Mangers might see a calendar block, a sudden shift in availability, a high performer who starts declining travel. The story shows up later in claims and turnover dashboards, but the lived experience stays invisible.
A benefits leader rarely hears the real reason someone leaves early for the day. Mangers might see a calendar block, a sudden shift in availability, a high performer who starts declining travel. The story shows up later in claims and turnover dashboards, but the lived experience stays invisible.
Menopause is one of the clearest examples of this gap. The costs are real, but they rarely arrive labeled. When symptoms stay private, care gets delayed and the plan absorbs avoidable downstream utilization.
Menopause is often discussed as a People & Culture consideration or a niche health support topic. The smartest health plan administrators consider menopause and postmenopause as a cost-and-risk topic.
Menopause-related costs are fragmented across medical and pharmacy claims, disability, absenteeism, presenteeism, and turnover. That fragmentation creates plausible deniability in budget conversations. It also creates a gap in care for a significant chunk of members of almost all US health plans and employer benefits programs.
If you are building an effective women’s health strategy, menopause is not a side quest. It is a predictable, sizable exposure. And it is one you can manage with effective, targeted care that prevents more costly downstream interventions.
The business case: working women suffer through menopause in silence
Nearly 20% of the U.S. workforce experiences menopause.¹ That is millions of people navigating a multi-year transition while they are still working, still leading, and still accountable for results. The impact is not neatly documented in claims reports as women with menopause-related pelvic symptoms often suffer through their discomfort without seeking care. Work and family commitments often get in the way. That is, unless more serious issues develop to the point where more expensive and invasive healthcare intervention is needed.
The macro cost for employers is not subtle:
- Global estimates place productivity loss due to menopause-related symptoms at $150B annually.¹
- One in five women will quit or consider leaving their job due to severe menopause-related symptoms.¹
Those numbers describe a risk profile you can actually plan for. If you are responsible for total rewards or health benefits planning, or making decisions about coverage for a health plan, you can have a direct impact on reversing this trend. More accessible and specific women's health coverage can allow your members to stay healthier throughout menopause and postmenopause.
The cost of menopause is hidden in pelvic symptoms
Menopause is associated with many symptoms, but for employers and health plans, pelvic symptoms are a major driver of both quality-of-life impact and downstream cost.
Sword’s Menopause at Work whitepaper uncovers the hidden pelvic health problems that so many women are suffering through without dedicated support.
Impact of menopause
The numbers that change the menopause cost conversation
49%
of menopausal working women report urinary symptoms including involuntary leakage.²
38%
of postmenopausal women experience bowel dysfunction.²
74%
of women ages 40 to 59 report some form of pelvic organ prolapse²
These are not edge cases. They are high-prevalence symptoms that quietly reshape the workday and care-seeking behavior. When employees manage them alone, they often wait longer to seek help, and the plan pays later through escalation and repeat utilization.
This is exactly why women’s health benefits need to be broader than just fertility or family formation coverage. The best plans don’t settle for solving for one moment in life. To reduce utilization and the expense or acute and invasive downstream procedures, you can invest in more proactive care that allows women to reverse their symptoms earlier.
These symptoms also tend to stay quiet at work. Many women do not discuss pelvic concerns in the workplace due to stigma and embarrassment, and some take time off without disclosing the reason.² When people feel they cannot name what is happening, they also do not access care early. That is how manageable issues become expensive ones.
The silent costs of menopause at work
- The absence code never says “menopause.”
- The member doesn’t raise a hand until symptoms start changing the workday.
- By the time a claim appears, the opportunity for earlier, lower-cost support has already passed.
Why traditional care models fail with accessibility and scale
ROI on healthcare investment comes from a care pathway that people will actually use.
Traditional in-clinic women's health care pathways usually require members to trade time, privacy, and predictability for care. For many women in midlife, that trade-off does not fit reality. They are balancing work, caregiving, and symptoms they may not feel comfortable addressing with a stranger in an unfamiliar clinic environment.

When the first step feels hard, women often suffer in silence before:
- symptoms escalate
- care starts later
- adherence drops
- more acute care is needed
- costs rise
From a plan management standpoint, ROI is not something you model once and then hope for. It depends on whether members can start quickly, stay engaged, and build enough consistency to change symptoms and care-seeking patterns.
When support is hard to access, hard to fit into a workweek, or uncomfortable to talk about, people tend to delay care, drop off early, and rely on short-term workarounds that often lead to more expensive escalation later. The best women's health strategies fit with the member's needs. A personalized AI Care program like Bloom allows your members to access care from the comfort of home at any time that suits their schedule.
What a measurable menopause benefit should do in contract terms
Before we talk about solutions, it helps to name the buying decision you are actually making. An effective menopause benefit should be able to answer, in enforceable terms:
- What is the defined population and symptom scope?
- What is the engagement model, and what does “active participation” mean?
- What outcomes will be measured, and on what timeline?
- What is the methodology for savings, and how do you avoid double counting?
- What are the exclusions, escalation pathways, and member safety guardrails?
This is where many “women’s health benefits” options fall apart. They offer broad promises, but the mechanics are not specific enough to survive procurement scrutiny.
If you want to be part of shifting healthcare toward outcomes, you cannot accept ambiguity. “Value-based” language only matters when it is measurable, attributable, and operationally realistic. Menopause is broad. Costs are real. That combination often pushes benefits teams toward programs that sound comprehensive but are hard to validate in claims, outcomes reporting, and governance.
Pelvic symptoms are where the story becomes clearer and more measurable. They are common in menopause and postmenopause, they disrupt daily life and work, and they often drive delayed care and avoidable downstream utilization.² When you give women a private, practical way to address these change the care pathway in a way that plans and employers can actually measure.³
Bloom supports women in menopause with 24/7 at-home access

Bloom provides the ideal solution to shift expensive downstream care costs and replace this with a personalized AI Care women’s health program. Members can access from the comfort and privacy of their own home to address and rehabilitate their symptoms before they escalate.
Each session lasts 10 to 15 minutes and can be completed from home. Members have access to the optional Bloom Pod, an FDA-listed biofeedback device that provides real-time feedback during sessions. The Sword app tracks progress and enables messaging with their Women’s Health Specialist for continued support.
This digital-first model eliminates barriers like scheduling, travel, and privacy concerns that often prevent women from accessing in-person care. Continuous guidance and progress tracking keep members engaged and deliver higher adherence, which directly translates to better outcomes⁷.
The 4-step Bloom member experience
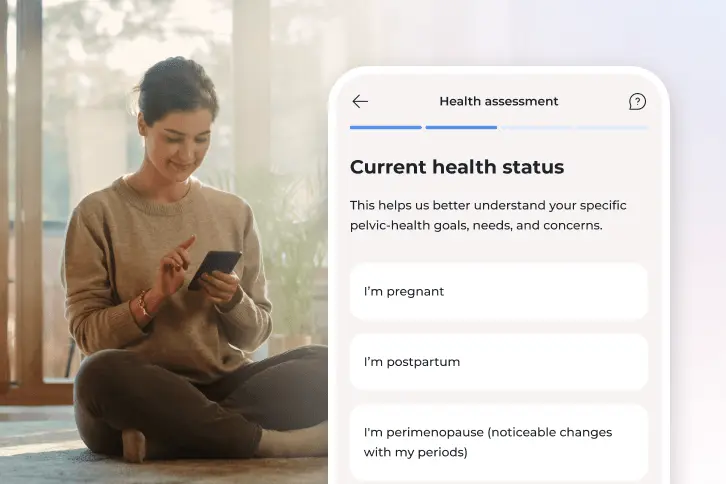
1. Member history check
The member shares symptom and their health history to inform a personalized care plan.
2. Matched care specialist
The member is matched with a Pelvic Health Specialist who guides each member's recovery.
3. Members get their Bloom kit
We ship everything the member needs, including the Bloom Pod, directly to their door.
4. Members recover from home
Recovery begins with real-time biofeedback helping to adjust the plan with progress.
Bloom’s ROI is validated based on pelvic care results, including lower downstream healthcare use.³ This makes it easier for benefits and plan teams to evaluate, track, and stand behind, while giving women a benefit they can actually use.¹ ² ³
In Sword Health’s Bloom pelvic health ROI analysis, validated by Risk Strategies Consulting, Bloom delivered impressive financial impact:
- $2,276 total healthcare savings per member per year with Bloom
- 2.9x gross ROI, validated by Risk Strategies Consulting
- $2.2K yearly direct cost savings per Bloom member³ ⁴
- Member-reported improvements including a 50% increase in productivity ⁴
For benefits leaders, this is the conversion from idea to decision: pelvic care can be measured, attributed, and contracted in a way that stands up to governance.
Support women in menopause with effective and specific care
Women’s health outcomes are not evenly distributed. Access barriers and stigma amplify disparities, especially for conditions that are hard to discuss.
In Bloom’s equity impact summary, women wait an average of 6.5 years to seek help for pelvic discomfort.⁴ That delay is a cost story as much as it is a care story.
If your strategy is to reduce preventable spend while improving member experience, you do not need a separate “equity program.” You need benefits that are accessible by design, and that can perform across diverse member populations.
If you are thinking, “We can do this, but it has to be simple to implement,” you are right to insist on that. A clean path usually looks like this:
- Define the scope clearly: Position pelvic symptoms as a core women’s health need that is relevant in menopause and beyond, not as an add-on.
- Align on measurement upfront: Agree on engagement definitions, outcomes cadence, and savings methodology before contract signature.
- Make eligibility and access frictionless: Members should be able to start without unnecessary administrative steps, and without requiring disclosure at work.
- Communicate with dignity: Benefits messaging should reduce stigma, emphasize privacy, and make the “what do I do next” step obvious.
This is how you build an effective menopause-adjacent women’s health benefit without adding governance burden. When you address menopause pelvic symptoms with measurable, accessible care, you can expect measurable health improvements and sustained cost savings across your population. ³ ⁴
If you want to evaluate whether Bloom fits your population and cost-containment goals, set up a chat with a Bloom expert to walk through the ROI methodology and the contract mechanics. You will leave that conversation with a clear view of what is being measured, how savings are attributed, and what an effective rollout looks like for your organization.
Offer Bloom and give women expert care from the comfort of home
Offer women life-changing support and slash claim costs driven by pelvic health conditions with Bloom's digital pelvic care plans.
Footnotes
Sword Health. A workplace playbook for menopause support. Reports & Guides. March 13, 2024. https://swordhealth.com/reports-and-guides/menopause-at-work.
Sword Health. Claims-based pelvic health savings with a 2.9x ROI. Reports & Guides. April 2, 2025. https://swordhealth.com/reports-and-guides/bloom-pelvic-health-roi.
Pereira AP, Janela D, Areias AC, Molinos M, Tong X, Bento V, Yanamadala V, Atherton J, Dias Correia F, Costa F. Innovating Care for Postmenopausal Women Using a Digital Approach for Pelvic Floor Dysfunctions: Prospective Longitudinal Cohort Study. JMIR mHealth and uHealth. 2025;13:e68242. doi:10.2196/68242. https://mhealth.jmir.org/2025/1/e68242/.
Sword Health. Bloom program overview. https://meet.swordhealth.com/bloom.
Sword Health. What is the Sword Bloom Pod and how does it work? https://swordhealth.com/articles/sword-bloom-pod.