September 19, 2025 • min read
Building a smarter women’s health strategy with digital pelvic care
Learn how to future-proof your women’s health strategy by adding more dedicated benefits including digital pelvic care.
Written by

Evidence-based healthcare insights
The healthcare benefits gap hiding in plain sight
Employers and health plans often describe their benefits strategy as “comprehensive,” yet one critical dimension is consistently underdeveloped: women’s health. Maternity care and parental leave policies may exist, but beyond those, most benefits portfolios leave gaps where extremely common women’s health issues are left without dedicated support. Pelvic health, menopause, and other women’s health conditions are too often overlooked.
This gap is costly. One in three women in the United States will experience a pelvic health disorder in her lifetime.¹ The ripple effects extend beyond personal discomfort: absenteeism, presenteeism, increased medical claims, and talent loss from a workforce already under pressure.² For employers competing in tight labor markets, failing to meet women’s health needs is no longer an option.
The opportunity is equally clear. By anchoring a women’s health strategy in digital pelvic care, organizations can create benefits that are equitable, cost-effective, and aligned with the real needs of half their workforce.
Why women’s health must be central to your benefits strategy
Women represent more than half of today’s workforce and make the majority of healthcare decisions in households. Yet their unique health needs remain underserved. Pelvic floor disorders such as urinary incontinence, prolapse, and chronic pelvic pain are relatively common and often underrepresented in workplace benefits offerings.¹
When left untreated, these conditions create significant costs.
- Chronic pelvic pain reduces job performance by more than 60%.³
- Surgeries for pelvic conditions average nearly $29,951.²
- Women with pelvic health disorders are also 3.6 times more likely to experience depression.⁴
These burdens add up across claims, absenteeism, and retention. Without proactive investment, women’s healthcare gaps undermine both workforce equity and financial performance.
The cost of fragmented women’s health programs
Many employers approach women’s health through a patchwork of point solutions: maternity leave support, wellness stipends, and generic healthcare benefits that lack targeted focus.
This fragmentation fails to deliver real outcomes. Given that pelvic floor dysfunction affects up to half of postmenopausal women and nearly three-quarters of women aged 40 to 59,⁸ it is clear these issues are too widespread to be overlooked. For employers, that prevalence translates directly into hidden costs in claims, absenteeism, and lost productivity across their workforce.
- Women delay seeking pelvic health care for an average of 6.5 years, during which symptoms worsen and treatment costs escalate.⁵
- One in five women experiences painful intercourse⁶
- 32% report urinary incontinence⁷
- Over 40% of postmenopausal women experience some form of pelvic floor dysfunction⁸
- Nearly three-quarters of women aged 40 to 59 experience pelvic organ prolapse⁸
Without integrated support, many women's pelvic health issues remain untreated, leading to unnecessary procedures and lost productivity.
The financial burden is steep: surgeries for pelvic floor conditions average nearly $30,000 and chronic pelvic pain alone can reduce workplace performance by more than 60%.² ³ Women also delay seeking pelvic health care for an average of 6.5 years,⁵ which means conditions often worsen and become even more costly before treatment begins.
A smarter strategy requires replacing fragmented benefits with an anchor program that addresses a critical, high-prevalence need and connects to broader women’s health goals.
Anchor your women’s health strategy in digital pelvic care
Pelvic health is one of the most pressing and overlooked issues affecting women at work. Nearly three-quarters of women aged 40 to 59 experience pelvic organ prolapse.⁸ Half of pregnant and postpartum women live with pelvic floor disorders.⁹ These conditions impact confidence, daily performance, and career progression.
Digital pelvic care removes barriers that keep women from treatment. These models work because they are private, discreet, and accessible, giving women the chance to engage in care without stigma or disruption. They are less intimidating than in-clinic options and allow sessions to be completed anytime, making it far easier for employees to stay consistent with treatment.
Evidence from peer-reviewed studies confirms that digital pelvic health programs achieve strong engagement and safety outcomes, with completion rates above 75% and minimal adverse events.¹¹
Satisfaction is also high, with members rating their experience an average of 8.6 out of 10, reinforcing the effectiveness of digital-first pelvic care.¹¹
By contrast, traditional in-clinic physical therapy programs often see adherence rates drop below 50% after just a few sessions, highlighting the relative strength of digital engagement models.¹¹
Anchoring benefits strategy in pelvic health builds measurable impact into the foundation of women’s health programming.
Bloom offers women clinically validated pelvic care from the comfort of home
By combining privacy, discretion, and accessibility, Bloom’s digital-first approach shows why virtual models work so well to close gaps in women’s health benefits.
Bloom is Sword Health’s revolutionary digital pelvic health solution, designed to give women access to expert care from the comfort of home.
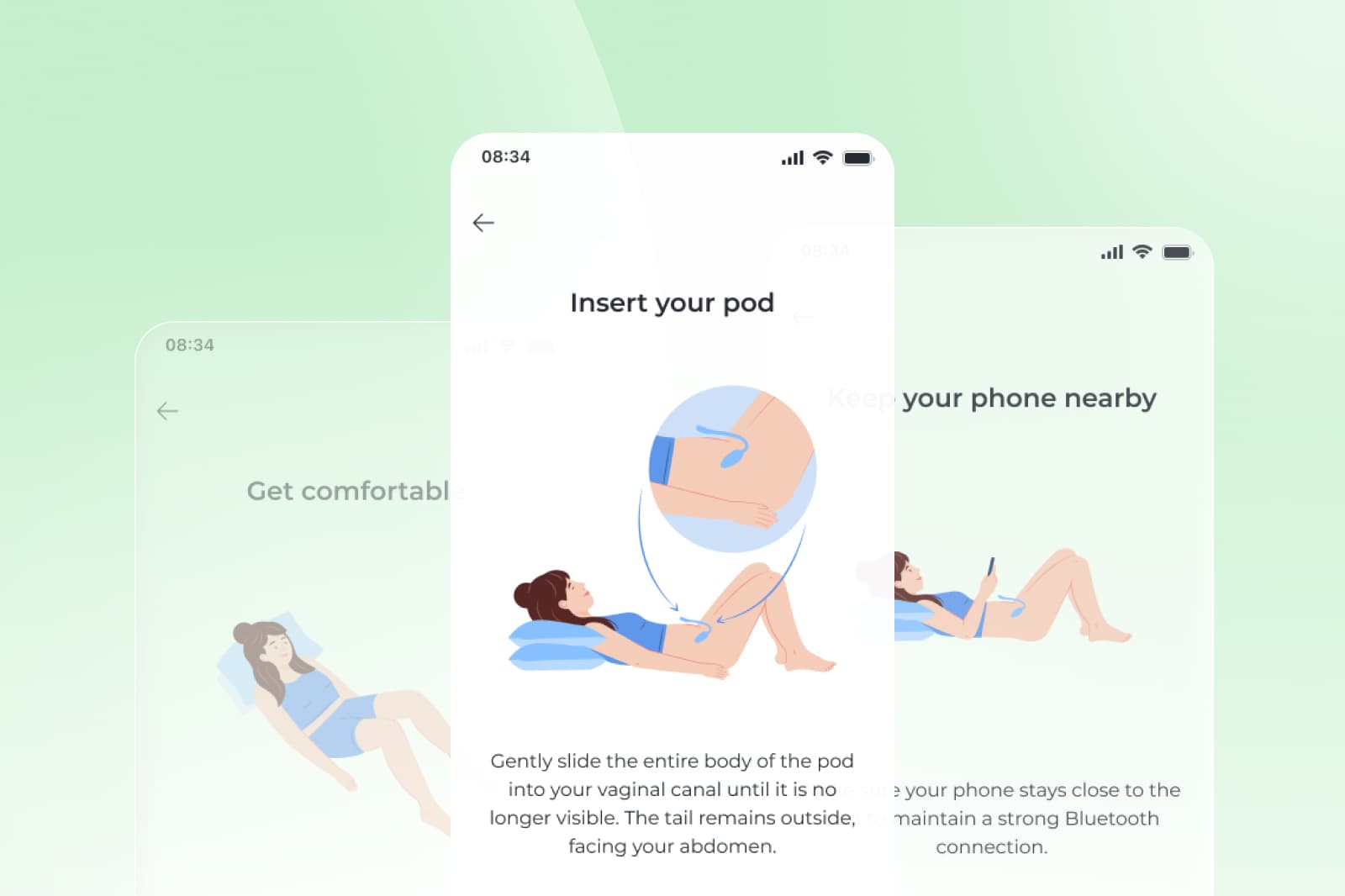
Bloom combines the power of pelvic care experts with the Bloom Pod, and FDA-listed medical device that is shipped to each member's home. The Bloom Pod is an intravaginal device that tracks pelvic floor muscle contraction and relaxation, offering real-time feedback and results to members through the app.
The combination of individualized care from a Pelvic Health Specialist (holding a Doctor of Physical Therapy degree), the Bloom Pod, and the Sword Health app provides real-time progress and results.

Bloom's a virtual-first programs give women access to expert care in the privacy and comfort of their own home. Sessions are short and can be completed at any time, with 50% completed after hours and 20% on weekends.¹¹
Bloom's clinically-proven results are powerful for members and health plans alike:
- 61% of members with moderate-to-severe conditions report significant improvement.¹²
- 56% improvement in anxiety and 50% improvement in depression among members screening positive at baseline.¹³
- $2,327 in yearly direct savings per member, delivering a 2.9:1 ROI.²
For employers, the higher engagement and satisfaction rates of Bloom directly translate into stronger ROI, since consistent participation drives better clinical outcomes and reduces costly downstream interventions.² In fact, analyses of Bloom cohorts have shown a reduction in avoidable pelvic surgeries, which often cost nearly $30,000 per case, adding another layer of savings for employers.²
Design a future-ready women’s health strategy
Employers often recognize the need to modernize women's health benefits but lack a guide or roadmap to get started. A future-ready women’s health strategy is structured, integrated, and data-driven.
Effective women's health benefits strategies share the following four foundations:
- Address gaps and uncover costs: Audit claims and employee surveys to identify hidden burdens like pelvic floor disorders, menopause, and maternal health needs.
- Provide a digital pelvic care option: Start with Bloom to address one of the most prevalent and costly gaps.
- Add other women's health benefits with specific focus: Layer in menopause, fertility, and maternal health solutions that align with pelvic health but provide support for those specific scenarios.
- Measure and communicate outcomes: Track health ouctomes and key metrics closely and seek providers who offer value-based care out outcome-based pricing models. Use ROI, productivity, and equity data to demonstrate value to leadership and employees alike.
By anchoring first in pelvic health, organizations create a base that ensures other women’s health investments connect and deliver stronger collective results.
Innovative employers are leading the way with stronger women's health benefits
Organizations that adopt integrated women’s health benefits are already realizing competitive advantages.
Large employers introducing Bloom have documented reduced surgical claims by avoiding unnecessary procedures.² Mid-size companies report retention of senior female leaders by addressing pelvic symptoms that previously drove turnover. Members themselves describe improved focus and confidence, reinforcing both productivity and engagement.
These stories demonstrate that women’s health strategy is not just an equity initiative, it is a lever for financial performance and talent resilience.
The massive ROI of offering stronger women's health support
Employers and health plans are accountable for proving ROI on every benefits investment. Women’s health delivers measurable returns.
Bloom’s program has shown:
- $2,327 average annual cost savings per member.²
- 50% improvement in productivity.¹²
- 49% lower likelihood of seeking other interventions.¹⁴
- 47% of members from high Social Deprivation Index areas achieving equivalent results to peers.¹⁴
When health equity improves alongside cost control and productivity, women’s health strategy proves itself as a business strategy.
Offer Bloom and stop women suffering in silence
Fragmented benefits approaches are no longer sustainable. They drain budgets, confuse employees, and miss the opportunity to address one of the largest hidden cost drivers in healthcare.
By anchoring a women’s health strategy in digital pelvic care, employers and health plans create a resilient framework that delivers value across claims, productivity, retention, and equity. Bloom is proven to deliver this impact at scale, and it integrates seamlessly into broader benefits design.
The organizations that act now will set themselves apart, not only as healthcare innovators but also as employers of choice.
Stop women suffering in silence with pelvic pain
Offer women life-changing support and slash claim costs driven by pelvic health conditions with Bloom's digital pelvic care plans.
Footnotes
Kenne K, et al. Sci Rep. 2022;12:9878. doi:10.1038/s41598-022-13501-w.
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi
Hutton D, et al. PLoS One. 2023;18(2):e0269828. doi:10.1371/journal.pone.0269828.
Koller D, et al. JAMA Netw Open. 2023;6(1):e2251214. doi:10.1001/jamanetworkopen.2022.51214.
Urol Nurs. 2005;25(2):109-115. PMID:15900979.
Tayyeb M, Gupta V. Dyspareunia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. PMID:32965830.
Kołodyńska G, et al. Prz Menopauzalny. 2019;18(1):56-61. doi:10.5114/pm.2019.87605.
Menopause. 2012;19(11):1235-1241. doi:10.1097/gme.0b013e31826d2d93.
Palmieri S, et al. Int J Gynaecol Obstet. 2022;158(2):346-351. doi:10.1002/ijgo.14019.
Sword Health, Bloom Book of Business, 2023.
Sword Health, Bloom Book of Business, 2023.
Sword Health, Bloom Book of Business, 2023.
Sword Health, Bloom Book of Business, 2023.
Sword Health, Bloom Impact on Health Equity Whitepaper, 2024. https://swordhealth.com/insights/gated-reports/bloom-health-equity