December 5, 2025 • min read
Can endometriosis still affect you after menopause?
Some women continue to experience endometriosis symptoms after menopause. Learn why it happens, when to seek care, and how Bloom supports pelvic comfort at home.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Some women still experience endometriosis symptoms after menopause, and others may develop pain that feels similar.
- Understanding how endometriosis behaves after menopause helps women make sense of their symptoms and know when to seek medical evaluation.
- With the right support and pelvic care strategies, women can manage symptoms, protect daily comfort, and feel confident knowing Bloom provides accessible, guided support at home.
Why you might be feeling pain after menopause
For many women, menopause marks a transition that brings relief from symptoms that once appeared during the menstrual cycle. Because of this, pelvic or abdominal pain after menopause often feels unexpected. Some women describe the sensation as confusing or even frightening, especially if they had endometriosis earlier in life.
These feelings are understandable. Pelvic pain after menopause can happen for several reasons, and not all of them are related to endometriosis. Hormonal changes influence almost every tissue in the pelvis. Muscles, nerves, digestion, and bladder sensitivity can all shift during this time. Many women notice aches or discomfort that come and go, or sensations that feel familiar but not exactly the same as before.
You are not imagining your symptoms, and you are not alone. This guide explains the reasons pelvic pain can appear after menopause, when it may be linked to endometriosis, and how to find the support you deserve.

Can endometriosis continue after menopause?
Endometriosis usually becomes less active after menopause because estrogen levels fall. Even so, research shows that about 2-5% of women continue to experience endometriosis symptoms after menopause¹. This happens for a few reasons that are important to understand:
1. Some endometriosis tissue remains sensitive even with low estrogen: Endometriosis lesions can respond to small amounts of estrogen produced by the body. Even after menopause, estrogen still comes from areas like body fat and adrenal glands. This means existing tissue may continue to cause discomfort, although usually less intensely than before.
2. Hormone therapy can influence symptoms in some cases: Hormone replacement therapy can be very helpful during menopause. For a small number of women, certain hormone regimens may stimulate endometriosis tissue. A clinician can help determine the safest approach based on your history².
3. Surgical menopause does not always remove every lesion: Some women undergo hysterectomy or oophorectomy expecting their symptoms to stop immediately. While these surgeries can help, endometriosis can remain if tissue outside the reproductive organs was not removed.
4. New or “de novo” endometriosis is rare but possible: There are documented cases of women developing endometriosis-like lesions for the first time after menopause³. This is rare and often linked to inflammation or structural changes in the pelvis rather than typical endometriosis behavior.
Endometriosis after menopause is not common, but it is medically recognized. Understanding the possibilities helps women feel less anxious and more prepared to discuss symptoms with a clinician.
Pelvic pain after menopause isn't always endometriosis
Pelvic pain shares many overlapping causes. This contributes to the uncertainty many women feel when they try to understand what their body is telling them. The good news is that several common explanations are not dangerous and respond well to gentle, supportive care.
Pelvic floor tension and muscle overactivity
The pelvic floor is a group of muscles that support the bladder, uterus, and bowel. During menopause, these muscles can become tight or overactive because of changes in tissue elasticity, posture, stress levels, or earlier patterns of holding tension. Many women describe this as a deep ache, pressure, or sharp pain that feels like endometriosis. A tight or overactive pelvic floor is extremely common and very treatable with guided pelvic care.
Digestive changes can mimic endometriosis discomfort
Digestion often slows during menopause. Constipation, bloating, and gas can create pressure that feels similar to pelvic pain. Women with a history of IBS may notice symptoms becoming more sensitive⁵. Because the intestines and pelvic nerves sit close together, it is easy to mistake digestive discomfort for pelvic pain.
Bladder sensitivity and urinary changes
Bladder urgency and frequency are common during menopause due to hormonal changes that affect the urethra and surrounding tissues⁴. When the bladder becomes irritated, it can create aching or cramping low in the pelvis. This can feel similar to endometriosis flare pain and the impact is significant on overall pelvic health.
Vaginal and vulvar tissue changes
Lower estrogen levels naturally thin the tissues around the vagina and vulva. This change can cause burning, pressure, or discomfort that many women initially interpret as internal pelvic pain.
Scar tissue or adhesions from the past
If you had endometriosis, surgery, or childbirth earlier in life, adhesions may remain in the pelvis. As tissues lose elasticity after menopause, these areas can become more noticeable.
Understanding these layers helps women feel grounded rather than overwhelmed. Pelvic pain is common after menopause, and many causes are manageable with the right information and support.
How to know if your symptoms need evaluation
Postmenopausal pelvic pain should be discussed with a clinician. Many causes are manageable and not serious, but some symptoms need timely attention for clarity and peace of mind.
Consult a clinician if you notice any of these severe symptoms:
- Bleeding after menopause
- Severe or worsening pelvic or abdominal pain
- Fever or nausea
- New or intense pain with bowel movements
- Unexplained weight loss
- Sudden increase in pelvic pressure
These symptoms do not necessarily indicate a serious condition. Even so, evaluation helps identify the cause and reduces uncertainty.
Practical ways to reduce pelvic and abdominal pain after menopause
The goal of pelvic comfort is not to eliminate every sensation. It is to support your body as it adapts to new hormone patterns and help you feel more at ease. These approaches can make a meaningful difference.
1. Support pelvic floor relaxation
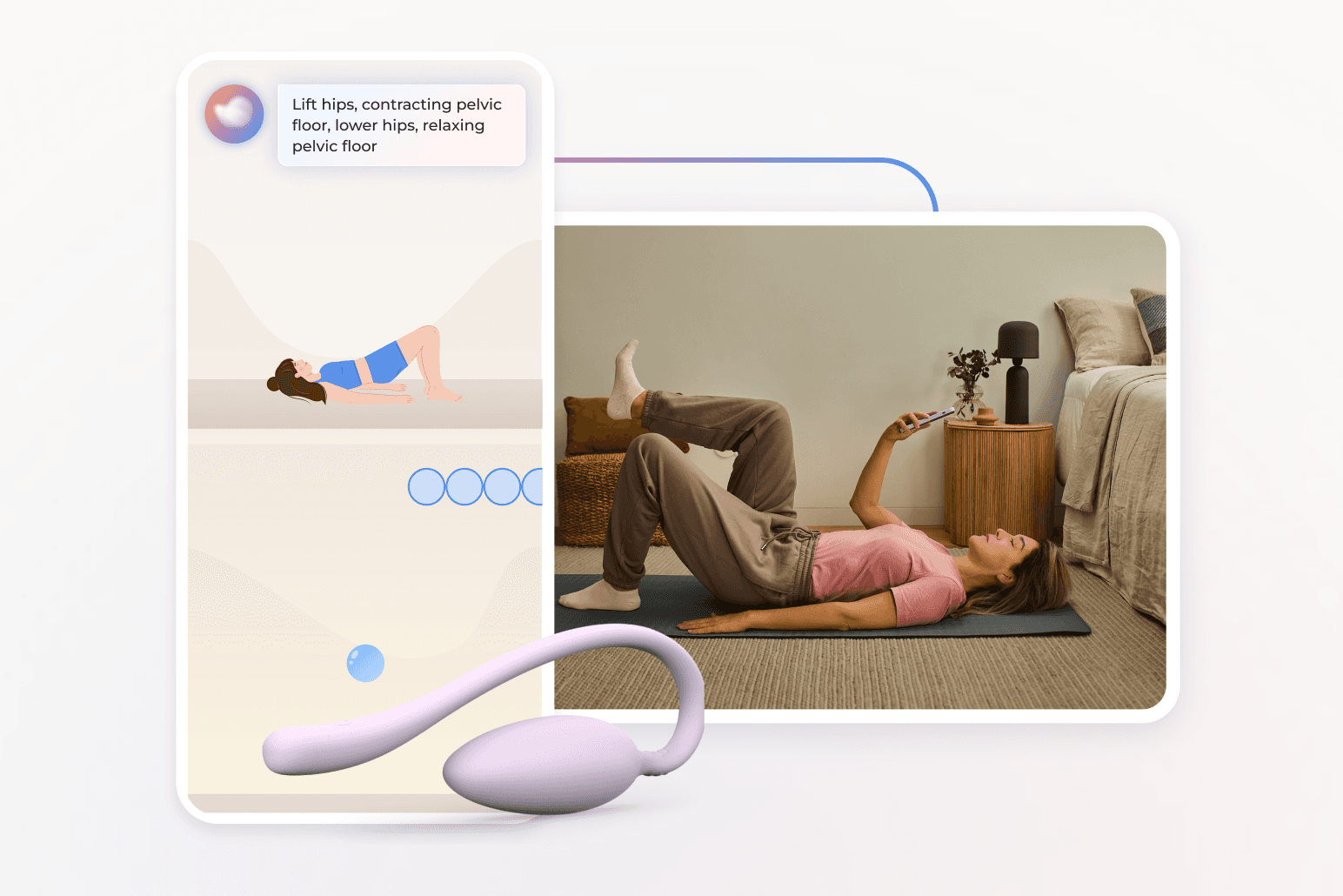
Many women unknowingly hold tension in the pelvic floor. Deep breathing, gentle stretching, and guided relaxation can reduce this tension. Sword Bloom is also an excellent support for women suffering from pelvic discomfort or pain. Each Bloom member is matched with a Women’s Health Specialist who holds a Doctorate in Physical Therapy. This care specialist prepares a personalized care program that you can complete from home. The program can teach techniques that help your pelvic floor release instead of tighten in response to discomfort.
2. Add gentle, steady movement throughout the day
Walking, stretching, and low impact exercises help reduce inflammation, support circulation, and ease muscular tightness. Small amounts of consistent movement are more effective than occasional intense exercise.
3. Use warmth to soothe pelvic muscles
Warm compresses or a heating pad can calm tight or irritated pelvic muscles. Heat increases circulation and helps tissues release tension, which many women find comforting.
4. Support digestion with nutrition and hydration
Digestive changes are a major contributor to pelvic discomfort. Increasing fiber, staying hydrated, and creating regular meal routines can help relieve bloating and constipation⁵. Simple adjustments often reduce symptoms significantly.
5. Prioritize rest that supports healing
Menopause can affect sleep. Establishing a calming routine and consistent sleep times helps your body reduce inflammation and restore muscle comfort.
These strategies are meant to be approachable. When practiced consistently, they help your body feel more supported and reduce the intensity of symptoms.
When endometriosis requires medical or surgical care
Some symptoms indicate that endometriosis or another condition needs medical evaluation. A clinician may suggest:
- Medication to reduce inflammation
- Adjustments to hormone therapy
- Imaging, such as ultrasound or MRI
- Evaluation for bladder or bowel contributors
- Laparoscopy if persistent lesions are suspected
This evaluation may sound intimidating, but each step provides useful information that helps clinicians tailor care to what your body needs. Many women feel comforted once they understand the source of their symptoms.
How Sword Bloom help you manage pelvic pain from home
Bloom offers a practical, gentle way to help your body feel more at ease. Every member begins with a digital assessment and works one-on-one with a dedicated Women’s Health Specialist who holds a Doctor of Physical Therapy degree. The program provides:
- A customized plan designed specifically around your symptoms, goals, and comfort level
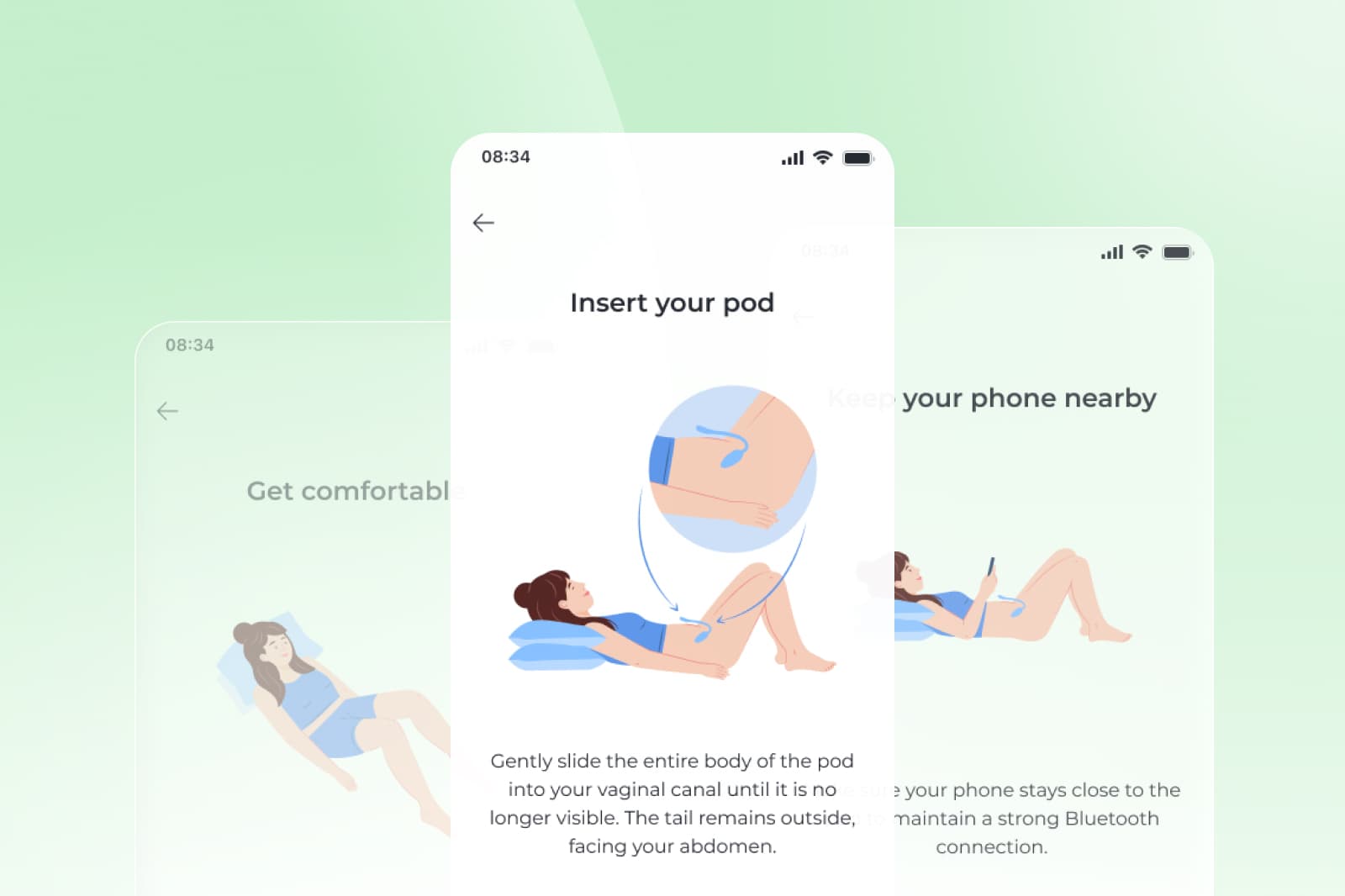
- From home sessions supported by smart technology
- Real time biofeedback from the Sword Bloom Pod to guide each exercise
- Ongoing adjustments based on your progress and needs
Get started with Sword Bloom in 4 easy steps
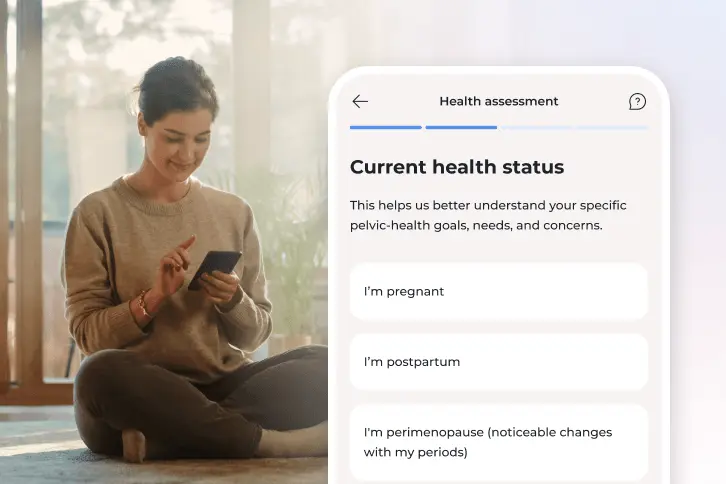
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
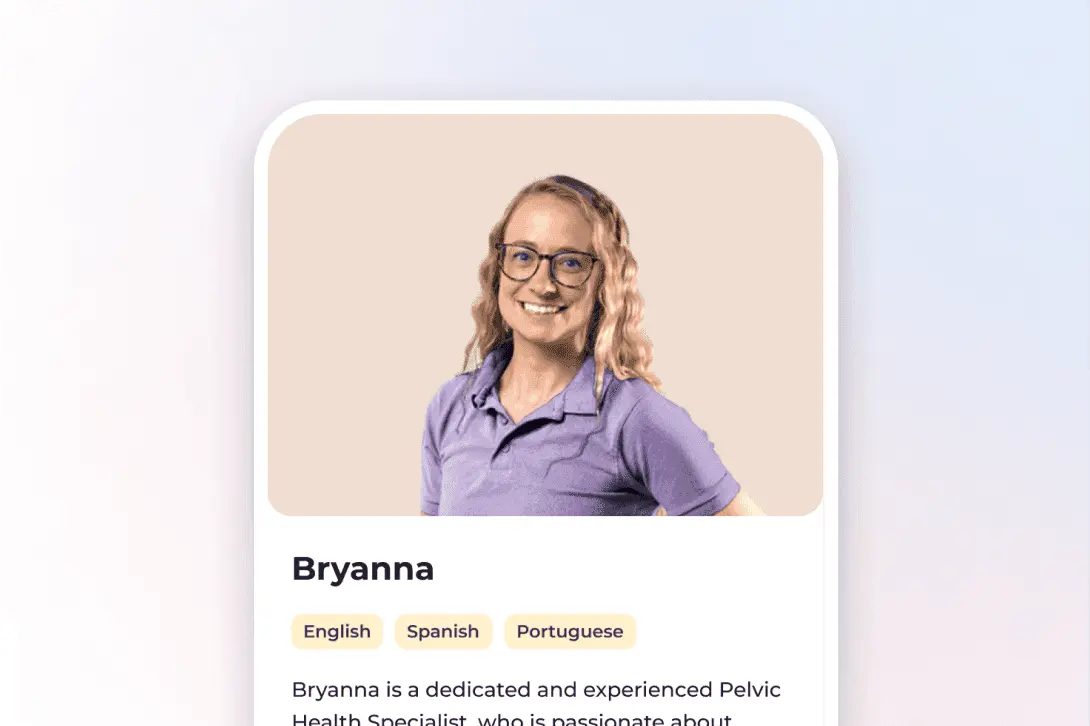
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Bloom does not replace medical evaluation for endometriosis. Instead, it works alongside it. Many women find that understanding how their pelvic muscles work and learning how to calm and coordinate these muscles reduces discomfort and increases confidence in their body’s resilience.
Check to see if your insurer already offers Bloom at no cost to you.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Gemmell LC, et al. The management of menopause in women with a history of endometriosis. Maturitas. 2017;104:7-11. https://doi.org/10.1016/j.maturitas.2017.07.015
Clayton RD, et al. Endometriosis after menopause. Obstetrics and Gynecology. 2003;101(5):953-955. https://doi.org/10.1016/S0029-7844(02)03201-4
Haas D, et al. Endometriosis in menopause. Facts Views Vis Obgyn. 2012;4(1):39-47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3344471/
Robinson D, et al. Lower urinary tract symptoms in menopause. Post Reproductive Health. 2017;23(3):155-162. https://doi.org/10.1177/2053369117713900
Bharucha AE, et al. Constipation and pelvic pain in women. Gastroenterology. 2021;160(5):1444-1455. https://doi.org/10.1053/j.gastro.2020.12.062