October 20, 2025 • min read
Postmenopause cramps: What they mean and when to get help
Learn why cramps can occur after menopause, when to seek medical advice, and how Bloom helps women improve comfort and prevent pelvic floor problems.
Written by

Evidence-based healthcare insights
The Sword summary warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Many women are surprised to experience cramps after menopause, long after their menstrual cycles have ended.
- These sensations are common and often linked to changes in muscle tone, hormones, or pelvic floor health, not something more serious.
- Understanding what causes postmenopausal cramps helps women take confident steps toward comfort and prevention.
- Bloom offers expert pelvic care designed to improve strength, flexibility, and comfort through personalized programs available anywhere, anytime, often at no cost through your health plan.
Why do cramps happen postmenopause?
Cramping after menopause can be confusing. Many women associate cramps with menstrual cycles, so feeling them years later can lead to concern. The reality is that postmenopausal cramps are common and usually caused by changes in muscle activity, hormone balance, or pelvic support structures rather than a serious medical condition¹.
You might notice sensations such as tightening in the lower abdomen, a dull ache across the pelvis, or occasional spasms. These can appear sporadically or during certain activities, like after sitting for long periods, exercising, or during digestion. While mild cramps are often benign, it helps to understand what’s happening in your body and when to escalate your care and talk to a doctor.
This guide will help you understand why cramps can still appear after menopause, what your body is signaling when they do, and how to ease them safely.
You will learn how hormonal and muscular changes affect comfort, what lifestyle habits make a difference, and when to seek medical guidance. Most importantly, we will explore how pelvic care programs like Bloom can help restore strength and confidence, and prevent future pelvic floor issues before they start.
Hormonal and muscular changes can cause cramps during or after menopause
Feeling cramps after menopause can be unsettling, especially when you expected those sensations to end with your last period. It’s natural to wonder what they mean or whether they signal something serious. The truth is that your body continues to change long after menopause, and those changes can affect how your muscles and nerves behave. Most of these adjustments are normal and manageable with the right care.
This section breaks down what’s happening inside your body in simple terms, helping you understand how hormones, muscles, and everyday habits work together to influence pelvic comfort and what you can do to stay comfortable and confident.
1. Hormonal shifts affect muscle tone and circulation
Estrogen supports muscle elasticity, nerve sensitivity, and circulation in the pelvis. As estrogen levels decline after menopause, the tissues and muscles in the lower abdomen and pelvis may lose some flexibility and hydration². This can make muscles tighten or spasm more easily, creating cramp-like sensations.
Even years after the final menstrual period, small hormonal fluctuations can continue to influence muscle behavior and the nervous system that controls pelvic activity³.
2. Pelvic floor tension or weakness
The pelvic floor acts as a network of muscles supporting the bladder, uterus, and bowel. If these muscles become weak or overactive, they can cause tension and cramping in the pelvic region⁴. Some women describe this as a feeling of heaviness or tightness that comes and goes throughout the day.
These sensations are very common. According to Sword Health’s Menopause at Work whitepaper, nearly three in four women between ages 40 and 59 experience some form of pelvic muscle dysfunction, often presenting as cramping, urinary frequency, or pelvic pressure. Over time, unmanaged tension can contribute to pelvic floor disorders (PFDs) such as prolapse or leakage, which are easier to prevent than to reverse⁵.
3. Digestive and urinary changes
Menopause affects more than reproductive organs. Lower estrogen can slow digestion and alter bladder sensitivity. Constipation, bloating, or urinary urgency can all create sensations that feel like menstrual cramps⁶. Maintaining hydration and movement helps regulate these systems and reduce referred pain in the lower abdomen.
4. When cramps may signal something else
Most postmenopausal cramps are related to muscular or hormonal factors, but there are times when they require medical evaluation. Cramps accompanied by vaginal bleeding, bloating that does not resolve, or sharp, localized pain should always be checked by a clinician⁷. In rare cases, these symptoms can indicate fibroids, endometrial changes, or gastrointestinal conditions that need medical attention.
You do not have to accept discomfort or live with these cramps as a normal part of life after menopause. While they can feel discouraging, your body is capable of change and recovery. With the right information and small, consistent habits, you can reduce these sensations, protect your pelvic health, and regain confidence in how your body feels.
In the next section, we will walk through simple, evidence-based ways to ease cramping and support your long-term comfort, steps that anyone can start from home.
How to manage and prevent postmenopausal cramps
Mild cramps can often be reduced through consistent movement, hydration, and pelvic strengthening. These steps help regulate circulation and muscle coordination across the abdomen and pelvis.
1. Move regularly to reduce muscle tension
Movement is one of the best ways to prevent cramps. Walking, stretching, and low-impact exercises increase blood flow and release muscular tension. Yoga or gentle core work can be especially beneficial.
Simple routines such as light stretching before bed or short walks during the day improve flexibility and prevent muscles from tightening. Even a few minutes of movement can ease discomfort⁸.
2. Support your digestion and hydration
A balanced diet and hydration routine help reduce pressure in the pelvic and abdominal area. Constipation or bloating can make cramping worse, so maintaining regular bowel habits is key.
Tips for digestive comfort:
- Eat fiber-rich foods like fruits, vegetables, and whole grains.
- Drink water throughout the day instead of large amounts all at once.
- Limit caffeine and alcohol, which can irritate the bladder and dehydrate tissues⁹.
Hydration also helps the pelvic floor work efficiently and keeps tissues supple, improving comfort during movement and rest.
3. Relax and strengthen your pelvic floor
Many women are unaware that their pelvic floor muscles can be both weak and tense at the same time. Over time, this imbalance can cause cramps, bladder changes, or a feeling of heaviness in the pelvis¹⁰.
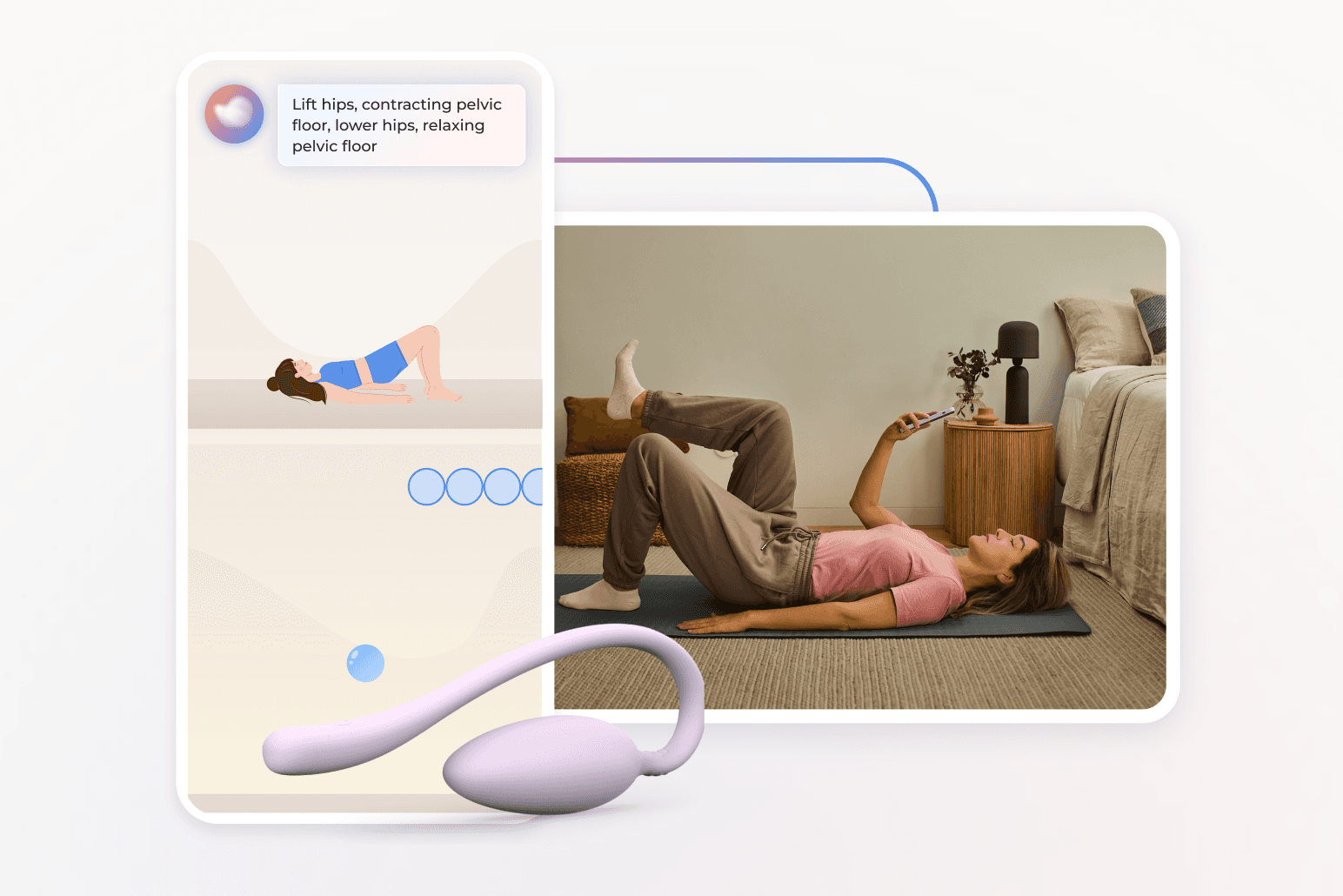
Gentle pelvic floor exercises help retrain muscle coordination. The goal is not just to strengthen but to restore normal tone and relaxation. Guided programs that teach correct activation and release can significantly reduce tension-related cramps¹¹.
Bloom makes this process simple. Each member is paired with a Women’s Health Specialist who creates a personalized care plan based on her symptoms, mobility, and goals. The optional Bloom Pod uses biofeedback to guide each movement, ensuring exercises are performed safely and effectively.
Sword’s 2025 Digital Pelvic Health for Postmenopausal Women study found that 65% of women reported improved comfort and mobility after using Bloom’s pelvic care program, with more than 77% completing their programs successfully, far exceeding typical adherence rates in traditional in-person care¹².
Beyond symptom relief, consistent pelvic health care helps prevent progression to pelvic floor disorders. Early strengthening improves circulation, supports the bladder and bowel, and reduces long-term risks of prolapse or urinary leakage¹³.
4. Manage stress and get quality rest
Stress can increase muscle tension, especially in the pelvis. When the body is under constant strain, muscles stay partially contracted, which can trigger cramps or tightness. Mindfulness, deep breathing, and adequate sleep support muscle relaxation and hormonal balance¹⁴.
Try a nightly routine that includes stretching or quiet breathing before bed. Avoid screens in the hour before sleep and keep your room cool and dark. Consistent rest helps your body recover and reduces the frequency of tension-related cramps.
How Bloom helps women stay comfortable and prevent pelvic floor issues
Bloom is a digital women’s health solution that supports women through every stage of life, but it's particularly helpful for women experiencing cramps during menopause and beyond.
Members work one-on-one with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. Together, they create a personalized care plan to strengthen and relax the pelvic floor, improve posture, and reduce tension that causes cramps or discomfort.
Each member receives a personalized pelvic care plan through the Sword Health app. The optional Bloom Pod, an FDA-listed medical device, measures muscle movement and provides real-time feedback to help women perform their exercises.
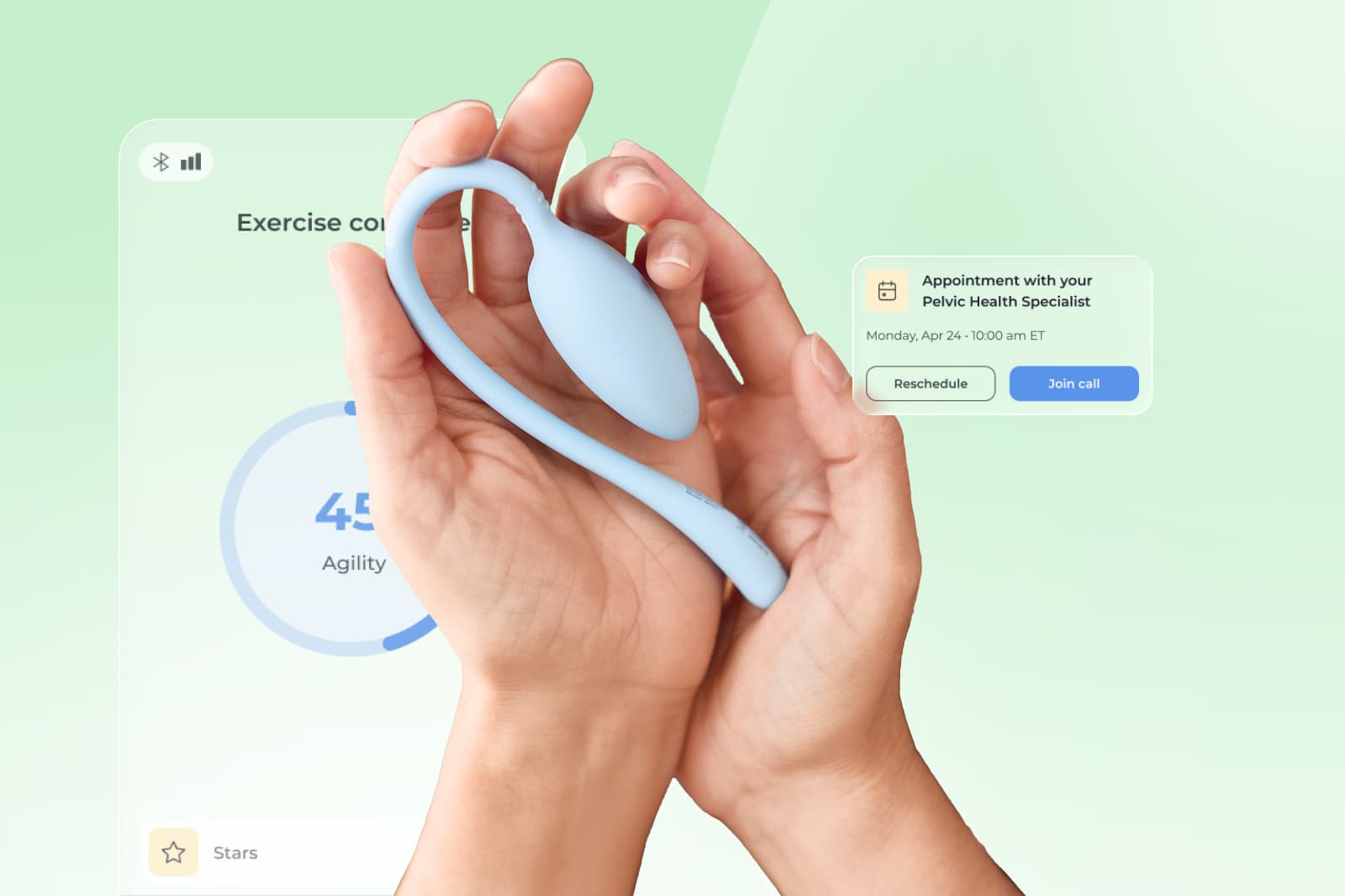
Sessions take just 10 to 15 minutes, and all you need to work on your personalized care plan is the Sword mobile app and the insertable Bloom Pod is fitted with biofeedback technology that provides guidance vis the Sword app during your exercises.
This makes it so easy for you to access expert care at any time and place to suit your schedule. And just by working on improving your pelvic control a couple of times a week, you can reduce the symptoms of cramps and help to prevent pelvic floor dysfunction in the future.
Get started with Sword Bloom in 4 easy steps
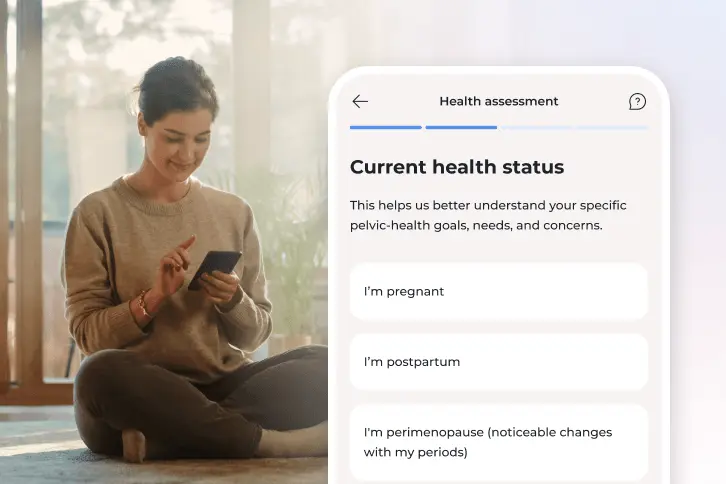
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Clinical outcomes from Sword’s Digital Pelvic Health for Postmenopausal Women study show that Bloom:
- Improves pelvic muscle coordination and overall comfort in 65% of women¹².
- Reduces the daily impact of pelvic symptoms by nearly 60%¹².
- Helps prevent the development of PFD symptoms, including urinary frequency and pelvic heaviness¹³.
- Achieves a 77% program completion rate, significantly higher than traditional in-clinic care¹².
Sword’s Menopause at Work study also found that women who participated in pelvic care reported improved quality of life, better energy, and fewer work interruptions, underscoring the broader benefits of proactive pelvic health programs¹⁵.
With Bloom, women can access professional, personalized pelvic care discreetly and conveniently, empowering them to take control of their comfort and health long-term.
How do you know when to seek medical help for pelvic cramps?
It is completely understandable to feel uneasy when something in your body changes, especially if cramps return years after menopause. Many women worry that these sensations might mean something serious, but most causes are not harmful. Still, your body deserves attention and understanding. Seeking evaluation is not about alarm, it’s about care and peace of mind.
You should reach out to a clinician if you notice:
- Persistent or sharp pain that does not go away
- Cramps accompanied by vaginal bleeding or spotting
- Bloating that worsens or does not improve
- A feeling of pelvic heaviness or pressure that increases over time
- Pain or discomfort that interrupts daily activities or rest
These symptoms do not always signal something serious, but they do mean your body is asking for attention. A clinician can help rule out causes such as fibroids, infections, or endometrial changes and guide you toward the right support. Early evaluation helps prevent small issues from becoming larger ones and gives you clarity about what your body needs.
If your cramps are mild but ongoing, you do not have to wait until they worsen. Gentle, guided pelvic care through Bloom can help you understand your body, reduce tension, and prevent further discomfort. Consistent attention, even to mild symptoms, is a powerful act of self-care that helps you stay strong and confident through every stage of life.
Stop accepting cramps and regain control with expert pelvic care
Cramps after menopause are common, and they are your body’s way of asking for care, not a sign that something is wrong. Understanding what causes them and knowing when to seek help is key to feeling in control again.
Pelvic care with Bloom helps women build strength, balance, and comfort through simple, guided programs designed to fit real life. Many employers and health plans include Bloom as a covered benefit¹⁵. Checking eligibility takes less than two minutes:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Li X, et al. Frontiers in Endocrinology. 2022;13:823454. https://doi.org/10.3389/fendo.2022.823454
Angelou K, et al. Cureus. 2020;12(4):e7586. https://doi.org/10.7759/cureus.7586
Kim S, et al. International Urogynecology Journal. 2022;33(12):3205–3215. https://doi.org/10.1007/s00192-022-05221-9
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Sword Health. Menopause at Work Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/menopause-at-work
Triadafilopoulos G, et al. Women & Health. 1998;27(4):55–66. https://doi.org/10.1300/J013v27n04_05
Walker MJ, et al. Menopause. 2023;30(4):451–459. https://doi.org/10.1097/GME.0000000000002178
Warburton DE, et al. CMAJ. 2006;174(6):801–809. https://doi.org/10.1503/cmaj.051351
Cumberbatch MG, et al. European Urology Focus. 2022;8(5):1264–1273. https://doi.org/10.1016/j.euf.2022.02.013
Bø K. Current Opinion in Obstetrics and Gynecology. 2020;32(5):395–400. https://doi.org/10.1097/GCO.0000000000000668
Janela D, et al. JMIR mHealth & uHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Sword Health. Bloom Health Equity Whitepaper. 2025. https://swordhealth.com/insights/reports-and-guides/bloom-health-equity
Irwin MR. Physiological Reviews. 2015;95(2):553–605. https://doi.org/10.1152/physrev.00032.2014
Sword Health. Menopause at Work Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/menopause-at-work