October 24, 2025 • min read
Endometriosis care: how to reduce pain and recover after surgery
A comprehensive guide to endometriosis covering symptoms, prevalence, and effective therapy solutions. Learn how pelvic care can help you recover.
Written by

Head of Clinical Affairs, Sword Bloom
Endometriosis care: how to reduce pain and ease the burden
Endometriosis care is one of the most urgent but often overlooked needs in women’s health. Millions live with symptoms for years before they receive a diagnosis, let alone effective care. The condition is common and complex, yet stigma, gender bias, and delays in diagnosis leave many people coping silently.
The stakes are high. Chronic pelvic pain, infertility, missed work, mental health challenges, and mounting medical costs all converge to make endometriosis a significant health and economic issue. On top of this, treatment pathways are fragmented, requiring people to navigate multiple specialists and therapies.
This is why comprehensive endometriosis care matters. It is not only about easing physical pain, but also restoring quality of life, preserving productivity, and reducing the long-term burden on individuals and families.
What is endometriosis?
Endometriosis is a chronic condition in which tissue similar to the uterine lining grows outside of the uterus, often on the ovaries, fallopian tubes, bladder, and bowel. These growths can cause inflammation, scarring, and adhesions that lead to pain and dysfunction.
One particularly severe form, known as deep infiltrating endometriosis, occurs when lesions penetrate deep into pelvic tissues and may affect the bladder, rectum, or other organs. This subtype often causes more debilitating symptoms and may require specialist treatment.
While the exact cause remains uncertain, researchers believe genetic factors, immune dysfunction, and hormonal imbalance all play a role.
One plausible theory is that endometriosis is caused by retrograde menstruation, a common phenomenon in which some of the tissue shed during menstruation flows backwards through the fallopian tubes into the abdominal space where the stomach, intestines, and liver are contained.
Common symptoms of endometriosis that go beyond painful periods
Endometriosis can result in a variety of symptoms. These symptoms can vary between onsets and also from person to person. The most common symptoms include:
- Chronic pelvic pain
- Painful or heavy periods
- Pain during or after sex, known as dyspareunia
- Painful bowel movements or urination, especially during menstruation
- Digestive issues such as bloating, nausea, or diarrhea
- Spotting or bleeding between periods
- Infertility or reduced fertility
- Heavy menstrual bleeding
- Digestive problems
Pelvic pain associated with endometriosis is commonly characterized as chronic, cyclic, and progressive, with periods of exacerbation.
The severity of these symptoms can also vary from person to person. It is also important to note that some people with endometriosis may not experience any symptoms at all, which obviously prevents significant challenges. The condition can be very difficult to detect in asymptomatic cases without coincidental surgical examination.
Prevalence of endometriosis and why diagnosis can take so long
Endometriosis affects up to 10 percent of women of reproductive age worldwide¹. It is most often diagnosed in people in their 30s and 40s, but it can occur at any age among those who menstruate.
Definitive diagnosis requires laparoscopic surgery, which makes it difficult to confirm. For this reason, diagnosis is often delayed for years, with an average wait of four to eleven years from the onset of symptoms. The delay is worsened by overlapping conditions like irritable bowel syndrome and the common dismissal of menstrual pain as “normal.”
On average, women wait 6.5 years to seek care for pelvic health conditions². Stigma, lack of awareness, and limited access to specialized care contribute to this delay, leaving people in pain without answers for far too long.
Why comprehensive endometriosis care can be life-changing
Endometriosis affects more than the body. It touches mental health, work life, relationships, and economic stability.
People living with chronic pelvic pain often experience high stress and fatigue, and women with pelvic health disorders are 3.6 times more likely to experience depression³. Productivity is also heavily impacted: more than 62 percent of people with chronic pelvic pain report reduced work productivity⁴. The financial burden is steep, with the average cost of care for patients with chronic pelvic pain estimated at nearly $30,000 per year⁵.
Without comprehensive endometriosis care, the cycle of pain, stigma, and delayed treatment can continue. Often, pelvic care programs can help women with symptom relief, preventative care, and a reduction in chronic pain.
Treatment paths in endometriosis care
There is no single cure for endometriosis. But a range of medical and supportive care options can help reduce pain and improve quality of life.
Endometriosis pain management
Pain management is often the first step. This can include prescription or over-the-counter medications, lifestyle adjustments, stress reduction, and pelvic floor therapy. Targeting pelvic muscle tension is especially important, as tightness in the pelvic floor and surrounding muscles often worsens pain.
Hormonal therapy for endometriosis
Hormonal therapies, including birth control pills, progestin treatments, and GnRH agonists, aim to regulate or suppress menstruation. This reduces the growth of endometrial tissue and can ease symptoms, though side effects and fertility considerations must be factored in.
Surgical treatment for endometriosis
Surgery is usually reserved for more severe cases or when conservative treatments do not work. Laparoscopic excision is the most common approach, allowing removal of lesions and adhesions. In advanced cases, more extensive surgeries may be necessary.
Non-surgical endometriosis treatment
Not everyone is ready or able to pursue surgery. Non-surgical endometriosis treatment includes pelvic floor therapy, behavioral health support, dietary strategies, and increasingly, digital pelvic health solutions that can be delivered at home.
Endometriosis and pelvic care care options
While there is unfortunately no cure, the symptoms associated with endometriosis are addressable. Women shouldn't have to suffer and pelvic healthcare options are available to minimize pain, discomfort, and that impact on quality of life.
Care options include pain management, hormonal therapies, and surgery to remove the adhesions, lesions, and cysts formed by the tissue growth. Often a combination of these options are required to treat the wide range of symptoms associated with this condition.
Sword Bloom's AI pelvic care helps women reduce pain from home
Bloom offers revolutionary virtual pelvic health care that allows women to access treatment from the comfort of their own home.
Pelvic pain management is effective for individuals suffering from endometriosis. Typically, people who present with any type of chronic pelvic pain tend to hold a lot of tension in their pelvic floor, abdominal, low back, and hip muscles. Over time, these muscles become tight and stiff, further contributing to the pain cycle, particularly during activities like using the bathroom and sexual intercourse. Chronic pelvic pain may also benefit from pain science and behavioral therapies as an essential component in holistic care.
Bloom helps individuals with endometriosis manage their pain and associated symptoms by teaching them how to relax and lengthen their pelvic floor muscles.
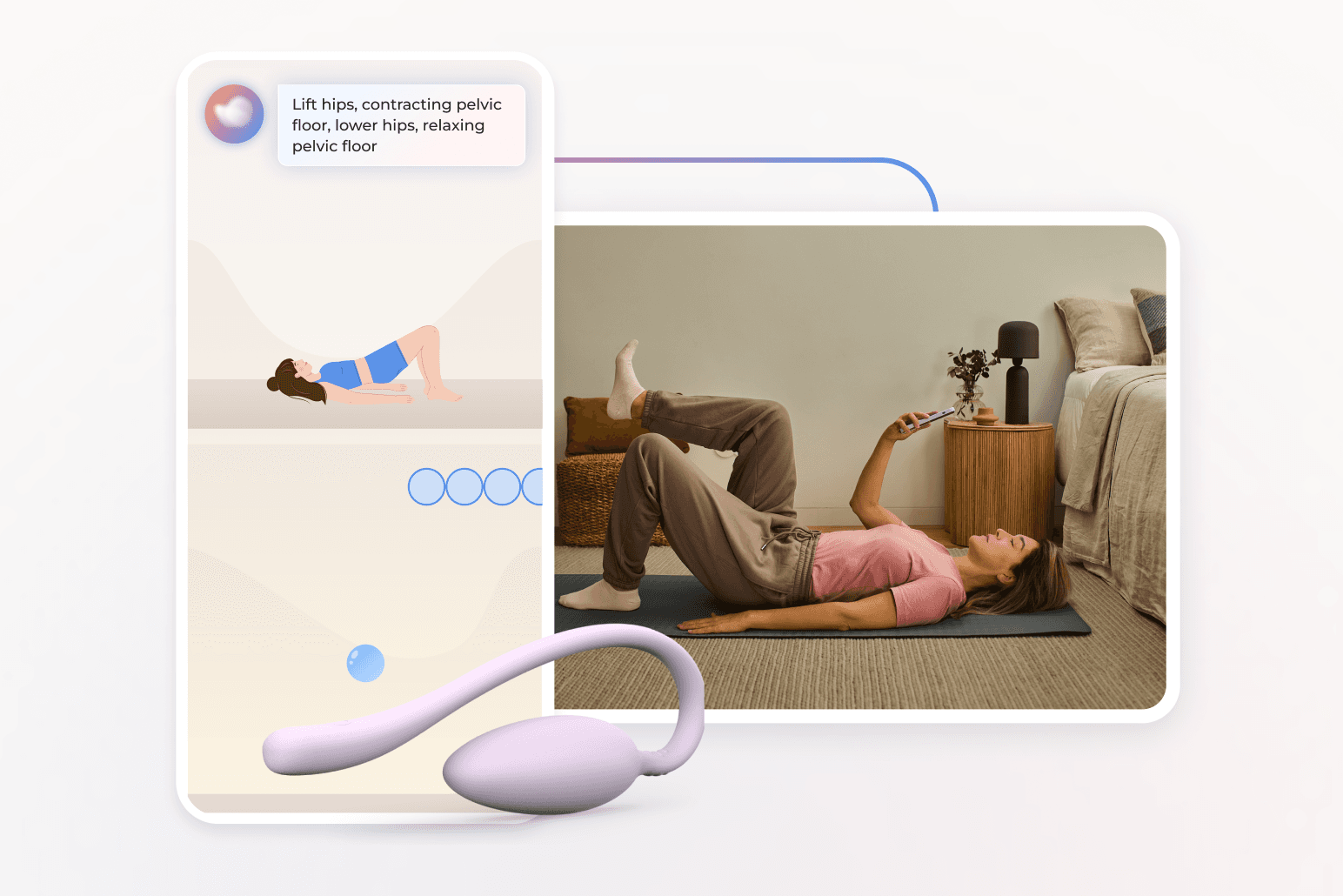
How does Bloom work?
Bloom guides patients through a customized exercise program, designed by a Pelvic Health Specialist, each carrying a Doctor of Physical Therapy degree. Each care plan is personalized to match the specific symptoms and recovery goals of each Bloom member.
You’ll complete sessions on your schedule, guided by real-time feedback from Sword's FDA-listed Bloom Pod medical device. The Bloom Pod is an easy-to-use intravaginal device with a in-built sensor that uses smart technology to help you track your progress. The Sword Health app gives you real-time feedback from the Bloom Pod, which measures pelvic floor muscle movement and force. This tracking works both in isolation and with your abdominal, low back, and hip muscles, depending on the exercise. in your plan.
Get started with Bloom in 4 easy steps
1. Tell us about you
Share your symptoms (like endometriosis for example), your health history, and goals so we can personalize your care.
2. Meet your Women's Health Specialist
You’ll be matched with a care specialists with a Doctor of Physical Therapy who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
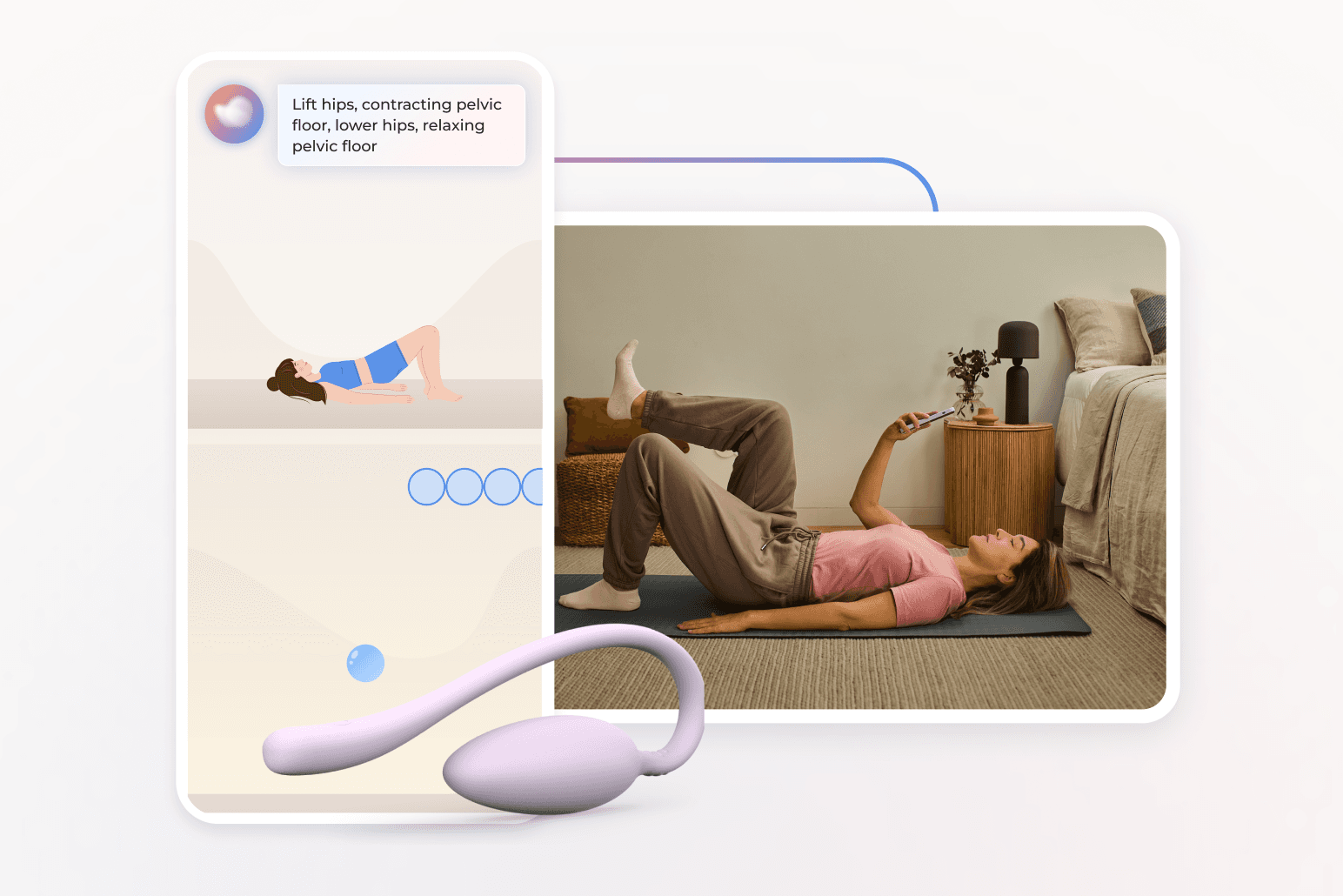
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Bloom is an ideal addition to supplement surgical care
Surgical treatment can be life-changing for some, but it is rarely the end of the story. Recovery requires rehabilitation, education, and ongoing care. Bloom supports members before and after surgery, helping them with scar management, core strengthening, and flexibility exercises. This continuity reduces post-surgical pain and helps restore confidence.
Bloom also plays a vital role for people choosing non-surgical endometriosis treatment. By guiding pelvic floor relaxation and teaching pain management strategies, Bloom empowers individuals to take control of their health at home.
Bringing endometriosis care to the comfort of home
Far too many people live with untreated or undertreated endometriosis because of stigma, limited access to specialists, or uncertainty about their options. Digital care solutions are changing that. Bloom enables people to manage endometriosis at home, with professional oversight and evidence-based programs designed by licensed clinicians.
Living with endometriosis is not something anyone should face alone. Modern care is about more than coping, it is about improving quality of life. With Bloom, people have access to personalized, clinically guided pelvic care that fits into their lives.
Bloom’s expert pelvic care plans may already be covered in your health plan at zero cost to you. You can check your eligibility in moments and enroll right away.
While we use the word "women" in some of our communications, Bloom is designed for all individuals with vaginal anatomy regardless of gender identity. This article is intended for educational purposes only, using publicly available information. It is not medical advice nor should it be used for the diagnosis, treatment, or prevention of disease. Please seek the advice of your physician or another licensed medical provider for any health questions or concerns. In case of emergency, call 911 or contact your relevant local emergency provider immediately.
End pelvic pain with Bloom’s discrete at-home care plans
Offer women life-changing support and slash claim costs driven by pelvic health conditions