October 10, 2025 • min read
Expanding pelvic health therapy access with digital care plans
Learn how digital women’s health programs make expert care so much more accessible for members, while also delivering strong ROI for health insurers.
Written by

Evidence-based healthcare insights
Pelvic health access is the overlooked gap in too many health plans
When employers and health plans talk about equity, the focus often falls on mental health, primary care, or chronic disease. Yet one of the most common and costly health challenges for women remains overlooked: pelvic floor dysfunction.
Pelvic health conditions affect 1/3 of women in the United States.¹ The prevalence increases with age, reaching nearly half of postmenopausal women.² Symptoms can include urinary incontinence, pelvic pain, prolapse, and bowel dysfunction, issues that disrupt daily life, diminish confidence, and impact workplace productivity.
Despite the scale of the problem, access to pelvic health care is strikingly limited. On average, women delay seeking help for 6.5 years.³ During that time, symptoms worsen, costs rise, and quality of life declines. In the workplace, this hidden epidemic shows up in absenteeism, presenteeism, rising claims, and turnover of experienced female leaders.
For employers and health plans, ignoring pelvic health access is not a missed opportunity to deliver better health outcomes and a costly blind spot resulting in more expensive downstream care interventions.
Why pelvic health access is a business-critical issue
The case for improving pelvic health access is not simply about compassion, though compassion is essential. It is about addressing a systemic health equity issue with direct consequences for organizational performance.
Research links pelvic health issues to:
- Productivity loss: Chronic pelvic pain alone reduces job performance by more than 60 percent.⁴
- High costs: Pelvic surgeries average nearly $30,000 per case.⁵
- Mental health impact: Women with pelvic floor dysfunction are 3.6 times more likely to experience anxiety or depression.⁶
- Retention risk: One in five women has considered leaving work due to unmanaged menopause-related symptoms.⁷
These numbers translate into real-world business outcomes. Higher medical claims erode benefits budgets. Absenteeism and presenteeism disrupt teams and projects. Losing senior women leaders undermines diversity, equity, and inclusion goals.
For organizations that want to control MSK costs related to women's health issues, or to maximize productivity and retain elite female talent for longer, offering dedicated pelvic health care is an easy and cost-effective decision.
The barriers keeping women from accessing pelvic health therapy
If pelvic health conditions are this prevalent and costly, why do so few women receive effective care? The answer lies in persistent barriers across geography, time, stigma, and socioeconomic status.
- Geographic access: In the United States, there is only one pelvic health specialist for every 10,000 women.⁸ Services are concentrated in urban centers, leaving many women in rural areas with little or no access. Even in cities, wait times for appointments can stretch months.
- Time and scheduling: In-person sessions require time away from work, travel, and often childcare arrangements. For mid-career women juggling professional and personal responsibilities, these logistics are enough to prevent them from ever starting care.
- Stigma and awareness: Pelvic health is still considered taboo in many workplaces and communities. Women are reluctant to discuss symptoms like leakage or pelvic pain with providers or managers. As a result, they wait years before seeking help, during which conditions worsen.³
- Socioeconomic disparities: Women in areas with higher Social Deprivation Index (SDI) scores face longer waitlists, higher out-of-pocket costs, and greater logistical challenges. These inequities compound existing health disparities, making care least accessible to the women who need it most.⁹
- Drop-off in traditional care: Even when women overcome these barriers and begin in-person care, many do not complete their full program. Two-thirds of patients stop after only six sessions, well before the recommended duration.⁹ Without consistent engagement, outcomes are limited and women are left discouraged.
These barriers create a cycle of delayed care, worsening health, and rising costs. To break that cycle, employers and health plans must adopt models that remove friction and stigma from care delivery.
Digital programs overcome the barriers of traditional pelvic health care
Digital women’s health programs have transformed access to care, much like virtual mental health and musculoskeletal programs. By bringing pelvic care into women’s homes, these solutions eliminate barriers of geography, stigma, and scheduling. Sword Health member data shows how digital care expands access equitably:
- Convenience: 50 percent of sessions are completed after hours and 22 percent on weekends.⁹
- Equity: 47 percent of members live in moderate-to-high SDI areas yet achieve outcomes equal to peers.⁹
- Engagement: Completion rates exceed 75 percent, compared to less than 50 percent for in-clinic programs.⁹
Care delivered virtually is private, flexible, and inclusive. Women no longer have to rearrange their lives to access support. Because digital programs track engagement and outcomes, employers and health plans can measure impact across entire populations.
Bloom delivers digital pelvic care at scale with a 2.9x ROI
Bloom by Sword Health was built to address the very challenges that have kept women from receiving pelvic health support. By combining doctoral-level specialists, advanced technology, and a digital-first model, Bloom makes pelvic care accessible, private, and scalable.
- Clinical expertise from care specialists: Each member is guided by a Women's Health Specialist who holds a Doctor of Physical Therapy degree.
- Industry-leading AI technology: The FDA-listed Bloom Pod measures pelvic floor muscle coordination and gives members real-time guidance on their exercises through the Sword app.
- 24/7 access from the privacy of home: Short, guided sessions take place at home with full privacy and flexibility.
- Support for women at all life stages: Bloom helps women across all life stages, from adulthood to postpartum and menopause.⁹
This approach overcomes the access barriers of traditional care and increases engagement and satisfaction rates. This is what enables Bloom to deliver better health outcomes and drive such significant return on investment as women find recovery faster and avoid more costly MSK care interventions.
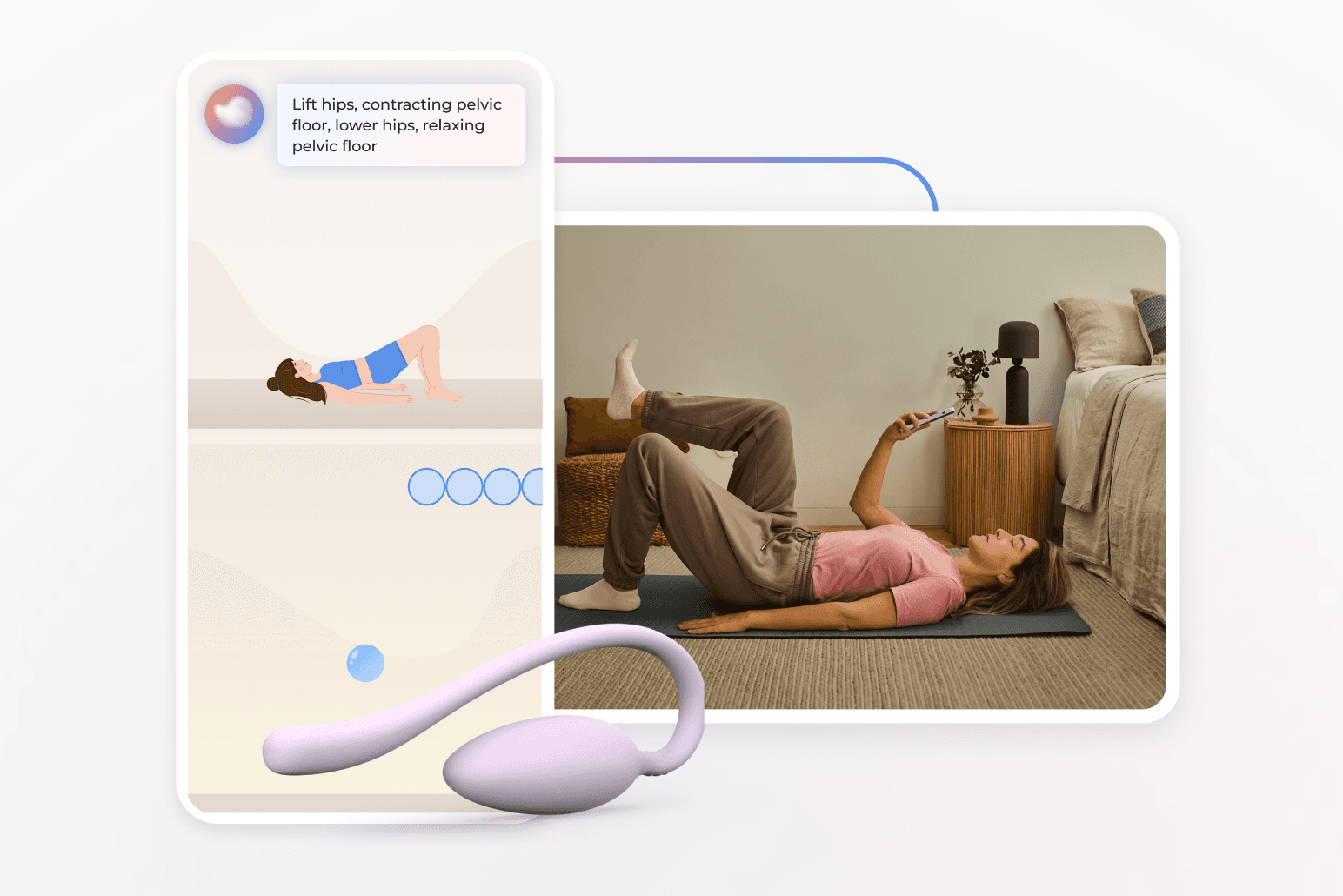
Sessions are short, discreet, and flexible. Because care is delivered virtually and members only need the Bloom pod and the Sword app, Bloom overcomes those access barriers to traditional in-clinic care. Women can work on their programs from the comfort and security of home at any time that suits their schedule. Nearly half take place outside standard business hours, and one in five happens on weekends.⁸ This leads to strong engagement and adherence levels, and better health outcomes as a result.⁸
How Bloom works in practice: the member experience
Members begin their Bloom journey with a virtual assessment from a Pelvic Health Specialist who designs a personalized program based on each woman’s symptoms and goals.
- The member receives her Bloom kit, which includes the Bloom Pod and app access.
- She completes interactive sessions with real-time guidance and feedback.
- Her specialist reviews progress and adjusts the plan as needed.
- For employers, anonymized dashboards report engagement, improvement, and cost trends across populations.
This combination of expert support and digital convenience enables lasting progress without the barriers of traditional in-person care.
Bloom's proven health outcomes for women
61%
of women with moderate-to-severe symptoms achieve meaningful improvement.⁹
9/10
The average member satisfaction rating of Bloom members⁹
56%
of Bloom members report a reduction in anxiety
50%
average improvement in productivity after nine sessions using Bloom
The employer and health plan cost savings of Bloom
For employers and health plans, the business case is clear:
- $2,276 in annual healthcare savings per member.10
- A 2.9:1 gross return validated by Risk Strategies Consulting.10
- A matched-control analysis showing 148 fewer pelvic surgeries among program participants, representing millions in avoided costs.10
- Implementation in under 90 days with minimal lift.
These results are validated through peer-reviewed research and independent actuarial review, giving decision-makers confidence in both the clinical and financial outcomes.
Pelvic health access is an equity imperative
Health equity is one of the defining challenges of today’s workplace. Employers and health plans are under pressure to deliver benefits that are inclusive, equitable, and measurable. Pelvic health sits at the intersection of gender equity, health equity, and workforce performance.
Expanding pelvic health access allows organizations to:
- Close long-standing gaps in women’s benefits.
- Retain and support women in leadership and frontline roles.
- Reduce hidden costs across claims, productivity, and turnover.
- Demonstrate leadership in equity and inclusion.
Pelvic health has been left out of equity conversations for too long. Virtual care provides the means to change that, and Bloom gives organizations a dedicated women's health program that delivers proven results across the largest member bases.
Stop women suffering in silence with pelvic pain
Offer women life-changing support and slash claim costs driven by pelvic health conditions with Bloom's digital pelvic care plans.
Footnotes
Kenne K, et al. Sci Rep. 2022;12:9878. doi:10.1038/s41598-022-13501-w.
Palmieri S, et al. Int J Gynaecol Obstet. 2022;158(2):346–351. https://doi.org/10.1002/ijgo.14125
Waetjen L, et al. Menopause. 2018;25(1):29–37. https://doi.org/10.1097/GME.0000000000000950
Patel KV, et al. Pain Reports. 2021;6(1):e913. https://doi.org/10.1097/PR9.0000000000000913
Lamin E, et al. Int Urogynecol J. 2016;27(1):65–72. https://doi.org/10.1007/s00192-015-2817-9
Molina R, et al. Int J Gynecol Obstet. 2024;164(1):154–162. https://doi.org/10.1002/ijgo.14790
Fenton A, et al. Menopause. 2022;29(8):932–940. https://doi.org/10.1097/GME.0000000000001995
American Physical Therapy Association. Workforce Data Report. 2023. https://www.apta.org
Sword Health, Bloom Impact on Health Equity Whitepaper, 2024. https://swordhealth.com/insights/gated-reports/bloom-health-equity
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi