August 27, 2025 • min read
The hidden cost of pelvic floor dysfunction in the workplace
Written by

Evidence-based healthcare insights
Pelvic floor dysfunction (PFD) isn’t just a private health issue. It’s a workplace problem hiding in plain sight.
Despite affecting one in three women at some point in their lives¹, PFD often goes undiagnosed, untreated, and unspoken. But the impact of pelvic floor pain shows in the form of medical claims, absenteeism, presenteeism, and lost productivity. For employers, the financial cost is substantial. For women, the burden is immense.
The financial toll of untreated pelvic floor disorders
- Nearly 20% of the U.S. workforce (roughly 27 million people) are currently experiencing menopause, and 49.1% of them report bladder issues like leakage².
- $3 billion in direct healthcare costs are tied to menopause-related health concerns each year in the U.S.²
- $150 billion in annual global productivity loss has been linked to menopause-related symptoms³.
- 1 in 5 women have considered leaving the workforce due to menopause-related issues, including pelvic pain and bladder symptoms³.
For women, the toll is personal, emotional, and threatening to their career trajectory. Pelvic floor dysfunction, pelvic pain, and discomfort associated with these conditions is life-altering. PFDs have an ongoing impact on health, confidence, and career continuity for too many women in the workplace.
This article explores the often-overlooked burden of pelvic floor MSK issues. We’ll quantify its financial and human cost, explain why traditional healthcare fails to address it, and show how digital-first pelvic care like Bloom by Sword Health gives employers a proven path forward.
What is pelvic floor dysfunction?
Pelvic floor dysfunction refers to a range of conditions involving the weakening, tightness, or poor coordination of the muscles and connective tissues that support the bladder, bowel, and reproductive organs.
It can affect anyone, but it disproportionately impacts women due to the physical stresses of pregnancy, childbirth, hormonal changes, and aging⁶.
Common symptoms of PFD
- Urinary leakage (stress or urgency incontinence)
- Fecal incontinence
- Chronic pelvic pain
- Pelvic organ prolapse
- Painful intercourse
- Constipation or incomplete bowel movements
Despite its prevalence, pelvic floor dysfunction is rarely discussed in healthcare settings or workplaces. Women often suffer in silence due to stigma, embarrassment, or the mistaken belief that their symptoms are simply part of aging.³
As a result, the issue remains invisible. This invisibility creates a hidden drain on both health and workplace productivity that needs attention from both employers and health plan providers.
Sword Bloom is a ready-made solution for PFDs
Pelvic floor dysfunction doesn't just create personal and professional challenges. It creates solvable ones. Employers who want to meaningfully reduce the burden of PFD in their workforce have a clear, scalable option: Bloom by Sword Health.
Bloom is a digital pelvic health program that removes barriers to care and supports women with personalized treatment they can complete from the privacy and convenience of home. It was built specifically to help working women overcome the challenges that keep them from seeking care, including long clinic waitlists, discomfort with in-person visits, and the scheduling inflexibility that often excludes those juggling caregiving or demanding careers. The program delivers expert care through three key components:
- A dedicated Women's Health Specialist who creates and guides a tailored treatment plan.
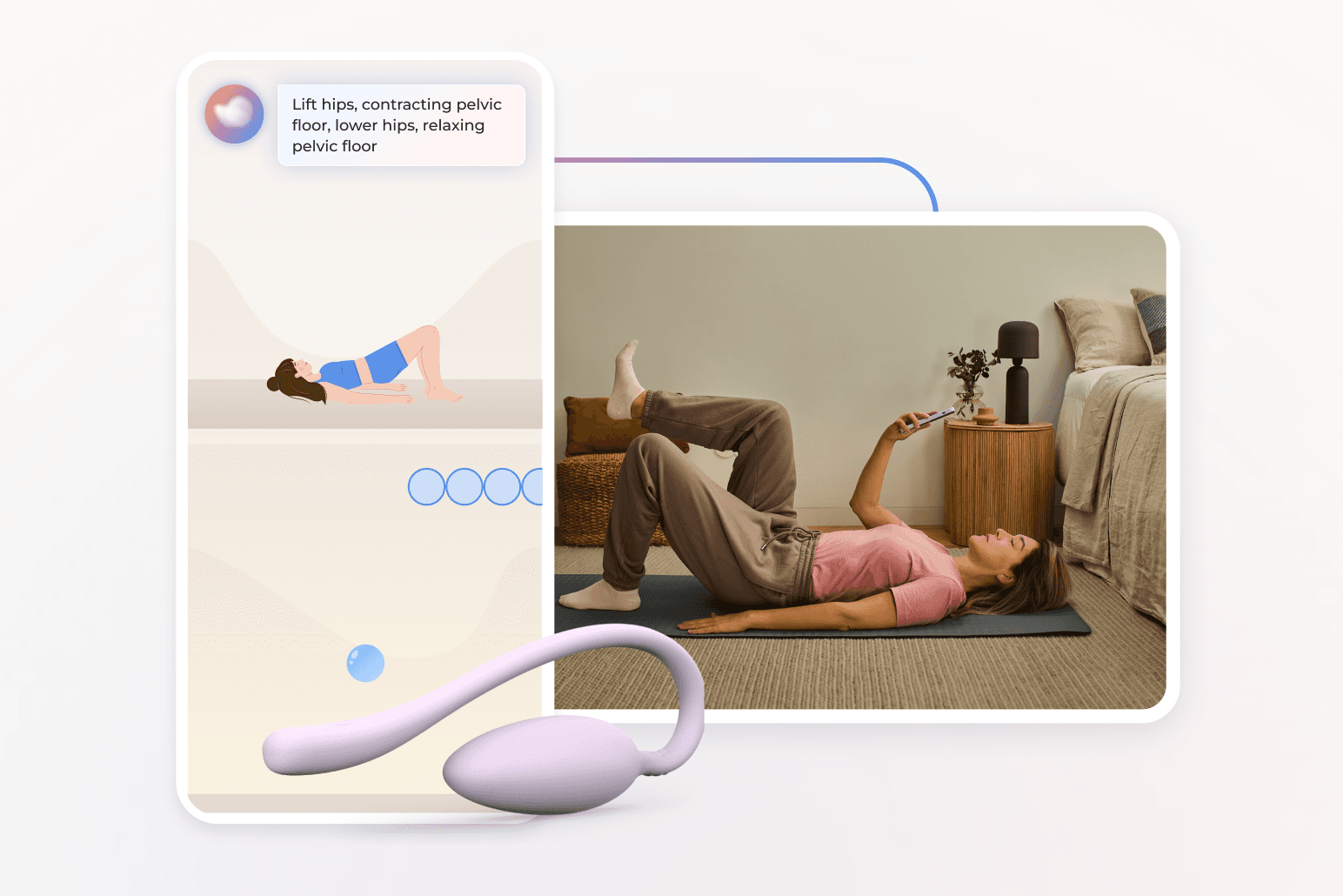
- The Bloom Pod, an intravaginal biofeedback device that connects to a secure mobile app for real-time sensor feedback.
- A library of clinician-developed educational content, personalized to the member's symptoms and goals.
Women complete their care on their own schedule, with real-time support from the Bloom app and asynchronous communication with their provider. The result is increased engagement, higher adherence, and better outcomes, all without the friction of traditional in-person therapy. For employers, Bloom offers a proven, cost-effective solution with measurable ROI alongside powerful clinical impact:
- average savings of $3,177 per member per year⁴
- 56% reduction in presenteeism⁴
- 67% reduction in further medical intervention⁴
Bloom helps women overcome PFD early, privately, and effectively. The combined results of improved individual well-being and worklpace productivity, enhances workforce retention, and contributes to more equitable health benefits across the organization.
Get started with Sword Bloom in 4 easy steps
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
How pelvic floor dysfunction affects women at work
For many women, pelvic floor dysfunction makes the simplest workday tasks difficult. Sitting through long meetings, giving a presentation, or commuting to the office becomes a minefield of discomfort, anxiety, and shame. This isn’t just a medical issue. It’s a barrier to full participation in the workforce.
The emotional toll of pelvic pain at work
The emotional toll is severe. Women with PFD often describe feeling embarrassed, isolated, or even broken⁴. The fear of leakage or accidents causes some to withdraw from leadership opportunities or social interactions at work.³ They may avoid travel, client-facing roles, or physically demanding tasks.¹
These effects can have serious implications for a woman's ability to stay fully engaged at work. The symptoms of pelvic floor dysfunction don’t just cause physical discomfort. They also bring emotional distress, social withdrawal, and reduced self-confidence. This combination leads to reduced productivity, missed opportunities, and even career stagnation⁴.
The physical impact of pelvic floor dysfunction at work
Physically, women with PFD often contend with urgent and frequent bathroom visits, fear of visible leakage, or the need to manage accidents discreetly. This can mean leaving meetings, missing calls, or stepping away from collaborative tasks without warning.
Pain and discomfort may make it hard to stand, walk, or sit for extended periods. This is especially prevalent for women in difficult physical roles or those that require extended desk work at an on-premise office. A team leader who can’t comfortably stand through a presentation or a customer service agent who must frequently excuse herself from her work station is navigating challenges most coworkers don’t see. This physical toll builds over time, reducing energy and making it so much harder for women to maintain their performance at work.
Some women cope by avoiding high-effort tasks or rearranging schedules around their symptoms. But when basic job duties become difficult or embarrassing, performance evaluations may suffer. And that, in turn, limits career advancement opportunities⁵.
These effects on productivity and job participation have economic implications for employers, especially when symptoms go unaddressed. A study by Kjerulff et al. found that women with chronic pelvic symptoms incurred significantly higher health expenditures and workplace absenteeism⁵.
The mental burden of coping with symptoms at work
Mentally, pelvic floor dysfunction contributes to significant stress and emotional strain. The uncertainty of when symptoms might flare creates a low-grade, constant anxiety. Women may worry about whether they can make it through a meeting, a commute, or even just a normal day without an incident.
Over time, this anxiety compounds. Add to it the shame and stigma of what’s considered a “private issue,” and many women begin to internalize a sense of failure or inadequacy. They may feel less capable or professional, regardless of their actual performance. Studies show that chronic symptoms can trigger or exacerbate mental health issues, including depression and burnout⁴.
When these struggles are combined with limited understanding from peers or leaders, they can lead to disengagement or even decisions to exit the workforce entirely⁴. In short, untreated pelvic health issues drain not only physical energy, but emotional resilience and mental focus. That hidden cost adds up quickly across a workforce.
Challenges confronting women with PFD in the workplace
Anxiety and shame, especially in high-visibility roles
- Loss of confidence, fear of judgment
- Struggles with concentration due to pain and distraction
- Avoidance of leadership or travel opportunities
- Overreliance on sick leave or PTO to manage symptoms
- Hesitation to disclose or seek help due to stigma
The employer’s blindspot: what PFD costs your business
From an employer’s perspective, pelvic floor dysfunction is rarely on the radar. It’s often not coded in claims data with a level of significance that matches the prevalence of these conditions across the workforce⁵.
But so many PFDs and pelvic pain related issues go unreported⁵. Those that do often come at a much larger cost as women delay seeking treatment until much more acute symptoms develop, meaning more expensive intervention is required.
The business impact is often misattributed as pelvic health issues disproportionately affect women in midlife, often during their most productive years³. It's hard to quantify the lost potential of women who make sacrifices in their career to deal with the harrowing restrictions of suffering from some pelvic floor disorders.
The hidden costs of pelvic health disorders in the workplace
According to Sword Health’s internal claims analysis, untreated pelvic floor issues significantly drive up direct healthcare costs³. More importantly, these issues disproportionately affect women during the peak of their careers, which can have long-term implications for leadership pipelines and gender equity².
One 2022 study found that 49.1% of menopausal working women experience bladder symptoms like leakage². Another revealed that nearly 20% of women had considered leaving work due to menopause-related issues³, many of which overlap with PFD symptoms.
Potential employer costs of untreated PFDs
- Presenteeism: Employees showing up but performing below capacity due to discomfort, fatigue, or distraction⁵
- Absenteeism: Sick days, unplanned leave, or schedule changes to accommodate symptoms⁵
- Short-term disability claims: Extended absences related to pain, surgery, or mental health consequences⁵
- Specialist visits, imaging, and surgery: Invasive and costly procedures often pursued when early intervention fails or is delayed⁶
If employers fail to support early and discreet treatment, costs multiply⁵. This can manifest for the employer in the form of more expensive claims, increased absenteeism, lost productivity, and even increased staff turnover⁵.
Why traditional pelvic health care falls short
Traditional pelvic health care often fails to reach the women who need it most. In-clinic appointments require time off work, access to nearby specialists, and the confidence to openly discuss symptoms that are deeply personal. This creates significant barriers, especially for hourly employees, caregivers, rural workers, or those already dealing with shame or stigma.
These barriers lead to care delays, drop-off, and worse outcomes. And when women don’t complete care, conditions worsen and costs rise.
That’s why digital-first care models like Bloom matter. By bringing evidence-based pelvic health therapy into the home, Bloom removes friction and increases engagement.
Digital pelvic health care is more accessible
Digital-first pelvic health care is reshaping how women access the treatment they need. Traditional in-clinic care comes with multiple barriers: time off work, transportation challenges, long waitlists, and the emotional discomfort of discussing sensitive symptoms face-to-face with a stranger.
Too many women don’t ever seek help, especially those managing full-time jobs, caregiving responsibilities, or living in rural or underserved areas.
Bloom by Sword Health was designed specifically to address and overcome these problems. The program combines:
- Virtual access to Doctors of Physical Therapy who specialize in pelvic health
- Personalized care plans tailored to each woman’s symptoms and goals
- A connected biofeedback device for real-time guidance during exercises
- Secure, judgment-free communication via app messaging
- Clinically validated outcomes and patient satisfaction
What sets Bloom apart from other pelvic care solutions?
Bloom offers expert pelvic health care that’s flexible, private, and accessible from anywhere. Women can work on the exercises in their care plan on their own schedule in the privacy of their own home. Gone is the need to rearrange their lives to fit into a clinic’s hours. The result is higher adherence, better outcomes, and reduced spend for employers.
What sets Bloom apart is its combination of clinical expertise and digital convenience. Every member is paired with a Doctor of Physical Therapy who specializes in pelvic health. Care is guided through the Sword mobile app, which integrates a discreet biofeedback sensor, the Bloom Pod, to provide real-time guidance during pelvic floor exercises.
Sessions are designed to fit around a woman’s daily life. Whether it’s early morning before the kids wake up or late at night after work, members can complete care when it suits them. This eliminates the most common reasons for care drop-off and helps women stick with their treatment. The added accountability of a specialist checking in on performance and progress helps improve engagement and adherence rates.
Offer Bloom and tackle the costs of PFDs in the workplace
Bloom’s proven results improve quality of life for women who are able to reduce their pain and discomfort. Employers and health plans also see the measurable business impact:
- $3,177 average per-member per-year (PMPY) savings for employers⁴
- 56% reduction in presenteeism, helping women stay more productive at work⁴
- 67% of users reduce or avoid further medical interventions like specialist care or surgery⁴
These numbers reflect real savings, real engagement, and real health improvements. Importantly, Bloom doesn’t just provide flexible logistics. It delivers better clinical engagement and measurable results.
Women report high satisfaction, improved symptoms, and reduced need for further intervention. And for employers, this translates into real financial ROI. It’s inclusive by design. Approximately 25% of members are from underrepresented minority groups⁴, and 90% of those using Bloom for menopause-related concerns are employed full- or part-time⁴. By removing the barriers to care, Bloom empowers more women to seek and stick with treatment, driving better outcomes at scale.
End pelvic pain with Bloom’s discrete at-home care
Offer women life-changing support and slash claim costs driven by pelvic health conditions.
Footnotes
D'Angelo S, Bevilacqua G, Hammond J, Zaballa E, Dennison EM, Walker-Bone K. Impact of Menopausal Symptoms on Work: Findings from Women in the Health and Employment after Fifty (HEAF) Study. Int J Environ Res Public Health. 2023;20(1):295. doi:10.3390/ijerph20010295
Bloom Book of Business, 2022–2023. Menopause focus area.
Reed T. The growing menopause-at-work market. Axios. November 2022. https://www.axios.com/2022/11/17/menopause-workplace-support-market
Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531–539. doi:10.1001/jamainternmed.2014.8063
Kjerulff KH, Frick KD, Rhoades JA, Hollenbeak CS. The cost of being a woman: a national study of health care utilization and expenditures for female-specific conditions. Womens Health Issues. 2007;17(1):13–21. doi:10.1016/j.whi.2006.11.004
Awwad J, Sayegh R, Yeretzian J, Deeb ME. Prevalence, risk factors, and predictors of pelvic organ prolapse: a community-based study. Menopause. 2012;19(11):1235–1241. doi:10.1097/gme.0b013e31826d2d94