August 22, 2025 • min read
GLP-1 muscle loss: The hidden cost of weight loss without movement
Up to 39% of lean muscle mass can be lost during GLP-1 treatment. Learn why structured movement is critical to protecting long-term health.
Written by

Head of Clinical Strategy, Sword Move
Does GLP-1 use cause muscle loss?
Early indications show the drugs are helping patients lose weight. But as more research and analysis is collected, concern around GLP-1 muscle loss is building. While GLP-1s promote fast weight loss, the type of weight lost matters.
Clinical research shows that up to 39% of lean body mass is lost during GLP-1 usage. Lean muscle loss from GLP-1 use presents an invisible but dangerous risk, for health insurers and patients alike.
Lean muscle loss isn’t cosmetic. This has serious implications for physical health, mobility, long-term function, and cost exposure. For health plan administrators sarcopenia muscle loss adds nearly $900 in excess healthcare costs per employee annually. Lean muscle is essential. Lose it, and you compromise strength, movement, and future health.
Medications are redefining how obesity is treated. Once primarily used to manage diabetes, GLP-1 drugs like semaglutide (Ozempic, Wegovy, and others) are now commonly prescribed in weight loss plans, especially for employers and health insurers aiming to support the metabolic health of their members. This guide explains how to support GLP-1 programs with prescribed movement plans designed to help GLP-1 users precent muscle loss to provide a lasting platform for success.
GLP-1 use and muscle loss are a dangerous mix
When most people hear "muscle," they often think of strength or fitness. But medically, lean muscle tissue plays a central role in health:
- supports everyday movement like standing, climbing stairs, or getting out of a chair
- helps regulate blood sugar and metabolism
- protects against injury by improving balance and strength
Losing muscle as part of medically-induced weight loss is a risk factor for a condition known as sarcopenia, or the progressive loss of muscle tissue.
What is Sarcopenia?
Sarcopenia is the progressive loss of muscle mass and strength that occurs with age or immobility. This muscle loss increases the risk of falls, frailty, and long-term disability.
GLP-1 medications, while effective for weight loss, can unintentionally trigger or worsen sarcopenia by accelerating lean muscle loss alongside fat loss. This isn’t just risky for individual health outcomes. It’s a looming cost concern for health plans, as muscle loss directly drives up rates of injury, recovery time, and downstream chronic care needs.
That’s why pairing GLP-1s with movement-based support is essential. Structured, clinically guided physical activity helps preserve lean mass, protect function, and make weight loss safer and more sustainable.
The costs and dangers of GLP-1-induced muscle loss
Sarcopenia isn't just something that happens with age. It’s increasingly tied to prescription-based weight loss and physical inactivity. And the consequences are stark:
- 33% of chronic pain in older adults is linked to sarcopenia
- Fall risk increases by 60% for people with low muscle mass
- In people with sarcopenic obesity (muscle loss combined with high body fat), the risk of disability more than doubles
Significant lean muscle loss can compromise the ability of a person to function safely and independently.
GLP-1s trigger rapid weight loss but not all weight is equal
GLP-1 medications reduce appetite and slow digestion. That leads to lower calorie intake and, often, significant weight loss.
This type of weight loss comes at a cost. Without proper support, the body breaks down both fat and muscle for energy. Clinical studies confirm: up to 39% of lean body mass lost with GLP-1 use is lean muscle. That number is a red flag. Especially because the majority of GLP-1 users are already physically inactive when starting GLP-1 medication.
Less than 1 in 4 U.S. adults meet the CDC’s recommended physical activity levels. The vast majority of GLP-1 users are starting from a place of deconditioning with low muscle mass and few habits to protect against further loss. When GLP-1 medication causes weight loss, lean muscle mass can be lost quickly.
This creates a dangerous paradox: while weight loss occurs as intended, the patient may also become physically weaker and more metabolically vulnerable.
The rebound problem (and what muscle loss has to do with it)
One of the biggest concerns with GLP-1 use is sustainability. So many people rebound to old habits after stopping treatment.
- Up to 70% of GLP-1 users stop taking the medication within one year
- And up to two-thirds of lost weight is regained within the first year after stopping
Here’s where muscle loss becomes critical. Muscle is metabolically active, meaning it helps burn calories even at rest. When muscle is lost during weight loss, the body’s resting metabolic rate drops. If a GLP-1 patient stops using the medication, the person is burning fewer calories than before, setting the stage for fat to return faster and more aggressively.
This triggers a harmful cycle:
Medication → muscle loss → weight regain → re-prescription
For employers and health plans, this creates ongoing pharmaceutical costs with diminishing returns and little functional health improvement.
The invisible cost of muscle loss for employers
Muscle loss rarely shows up as a diagnosis. But the impact and costs are obvious:
- Rising MSK (musculoskeletal) claims
- Chronic pain, falls injuries, and fatigue-related disability
- Increased absenteeism and reduced productivity
These indirect outcomes are expensive. Sarcopenia is associated with $900 in excess healthcare costs per employee, per year, mostly tied to pain management, falls, and downstream care.
That’s just one layer. Physical inactivity overall accounts for 27% of total employee medical spend. These are overwhelmingly preventable costs related to chronic conditions, injuries, and recovery expenses.
If GLP-1 users are losing lean muscle and not adding physical activity to their treatment plan, then employers risk paying for short-term success with long-term risk.
GLP-1s without movement? A high-cost gamble
GLP-1s offer a powerful start. But weight loss without muscle preservation is a risky proposition at any scale. Consider this:
- GLP-1s can cost up to $10,000 per member per year
- Projections for GLP-1s to make up 9% of total medical spend in some plans
That’s a massive investment. Without structured movement to offset the muscle loss, employers are often footing the bill for temporary change without long-term return.
Prescribing GLP-1 medication without supporting behaviour change is like putting out a fire, then walking away without fireproofing the building. The immediate crisis is addressed, but the risk of damage returns unless the root vulnerability is resolved.
Movement + medication is part of the GLP-1 prescribing guidance
Matching structured movement programs with GLP-1 prescriptions is documented as standard protocol by pharmaceutical providers. GLP-1 medications like semaglutide are only approved for weight management as an adjunct to a reduced-calorie diet and increased physical activity. That’s not a recommendation. It’s part of the actual prescribing indication.
Yet despite this, many patients start treatment without any structured movement plan, putting them at risk of lean muscle loss, slower progress, and weight regain.
Muscle retention > habit formation > better outcomes
Build movement plans into your GLP-1 strategy
Movement is part of the prescribing recommendations for GLP-1s, it’s not just a lifestyle suggestion. Physical activity plays a direct role in:
- Preserving lean muscle mass
- Improving metabolic efficiency
- Supporting mobility and reducing fall risk
- Creating the routines that sustain health outcomes post-medication
Even modest levels of structured movement make a difference. But the key is consistency and personalization, especially for populations that may be starting from low baseline activity levels. When employers treat movement as a “wellness nice-to-have,” they miss the clinical and economic value it provides. When they integrate movement as part of the GLP-1 strategy, they protect against avoidable MSK risk and make the most of their pharmaceutical investment.
Sword Move helps close that gap with personalized activity plans designed to support the success the prescription started.
The deconditioned baseline: why most GLP-1 users start behind
Let’s look at the data from a real-world GLP-1 adjacent population members using Sword’s Move program of regular physical activity:
- 77% are overweight or obese
- 34% are current, former, or potential GLP-1 users
- 64% have an addressable condition (like diabetes or high cholesterol)
- 55% report difficulty with basic physical activity
This means most members start their journey with low functional capacity, limited movement habits, and higher MSK risk. For these individuals, the addition of GLP-1s without structured movement can actually accelerate loss of function.
The solution? Start with movement or introduce it early enough to counteract the side effects of rapid weight loss.
Behavior change is the multiplier GLP-1s are missing
GLP-1s drive weight loss. But it’s behavior change that determines whether that weight loss becomes long-term health. Physical activity is the behavioral foundation that helps:
- Maintain muscle mass
- Build confidence and capacity for movement
- Reduce the risk of re-prescription and rebound weight gain
This is both good medicine and good economics. Every dollar spent supporting movement has the potential to reduce future MSK costs, medication dependency, and disability risk. When structured programs are used, they create a scalable and measurable path to ROI.
How to prevent GLP-1 muscle loss for members
Simply, GLP-1 prescriptions should be accompanied by structured movement programs to help retain lean muscle and trigger positive behavior change. Sword Move is built to close this clinical gap.
Move gives employers and health plan providers a simple solution that delivers lasting movement habits for GLP-users.
What is Sword Move?
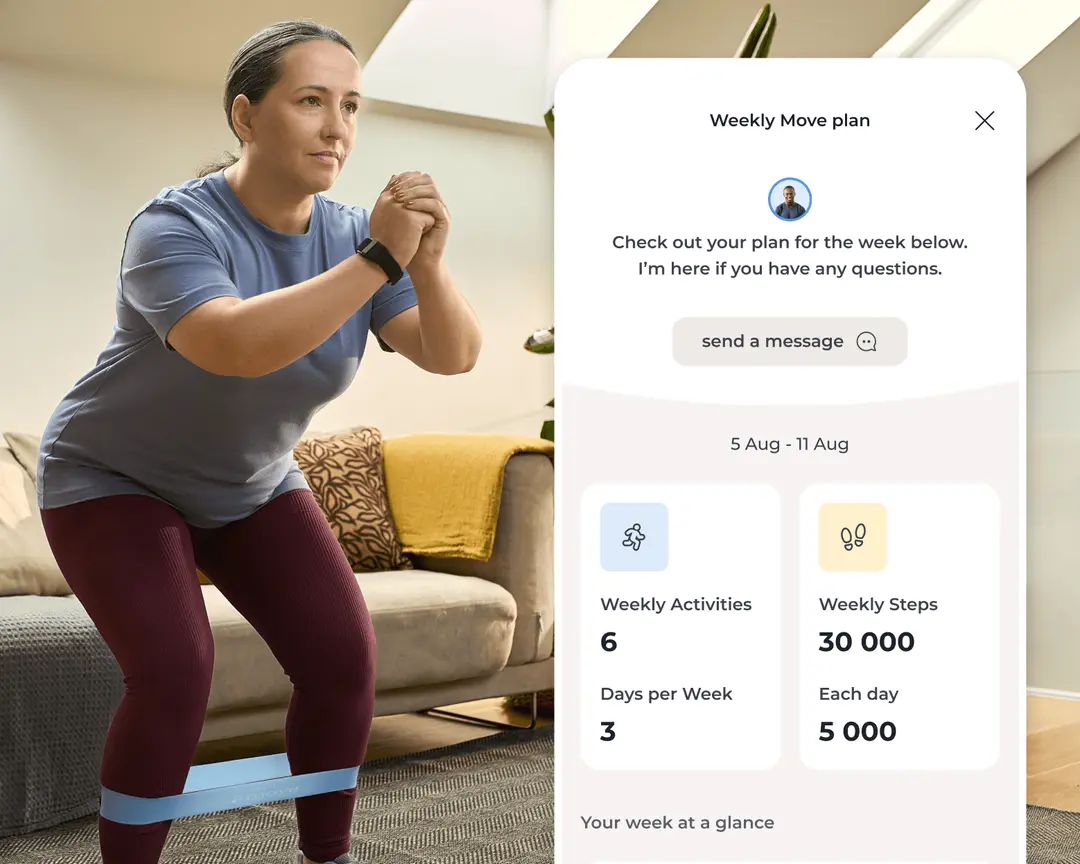
Move delivers whole-body, movement-first exercise programs to help members build sustainable activity habits, retain lean muscle, and reduce the risk of MSK conditions. Each Move member is assigned a physical health specialist with a Doctor of Physical Therapy. The personalised care plan is adapted as the patient progresses, with ongoing expert support from their assigned PHS.
How Sword Move helps members retain muscle
1. Members explain their goals
Members outline their specific health targets, job type, lifestyle, and movement history.

2. Match with a Physical Health Specialist
Each member's dedicated Sword Move specialist created a personalized care plan.

3. Member receive a Move kit
The Move wearable and resistance bands are delivered to the member.
4. The exercises build strength and movement
Exercises begin and the matched care specialist adjusts the plan and gives feedback as the member progresses.
Evidence-based benefits of pairing GLP-1s with movement
Many Move members begin their health journey with low physical activity, high health risk, and reduced physical capacity. Move supports these members with accessible, personalized activity — and the results show some significant improvement.
Outcomes among Inactive and Insufficiently Active members
- 69% of “Inactive” and “insufficiently active” members reach “active or healthy active” status within 10 weeks16
- Sedentary time reduced by 1 hour 22 minutes per day for previously “inactive” or “insufficiently active” members18
Outcomes across the entire Sword member base
- 4.5 sessions per week completed on average19
- 78% of Move users report feeling moderately better or much better17
These outcomes are not specific to GLP-1 users but they address the exact risks that GLP-1-only strategies leave behind. While long-term ROI data is still in development, early results are compelling. Sword Move is already showing measurable improvements in behavior, health, and clinical engagement with target populations.
- Increased activity and engagement
- Lower sedentary time
- Improved member-reported well-being
Because Sword uses outcome-based pricing with payments tied to individual member outcomes, employers can deploy Move confidently, knowing they only pay when results are delivered.
Support GLP-1s with movement plans to retain muscle and protect ROI
GLP-1 medications suppress appetite and slow digestion. But they don’t build strength or long-term resilience.
Patients don't recognise the dangers of medication-only service.
GLP-1s offer a promising start, but without physical activity, that progress often doesn’t last. Up to two-thirds of weight lost is regained within one year of stopping the medication⁵. When it returns, it’s often fat, not muscle.
Medication + Movement drives lasting GLP-1 weight loss success
- Weight loss needs muscle preservation
- Support GLP-1 prescriptions with structured movement plans
- Regular physical activity drives long-term behavior change
- Avoid re-prescription, weight regain, and costly downstream MSK issues
Frequently Asked Questions
Does GLP-1 cause muscle loss?
Yes. Up to 39% of lean muscle mass can be lost during treatment, especially in inactive users.
Isn’t weight loss the goal? Why does muscle matter?
Muscle isn’t just for strength, it supports metabolism, balance, and daily function. Losing it can increase health risks and costs.
How can we prevent muscle loss during GLP-1 use?
Structured physical activity (including things like resistance training, mobility exercises, and regular movement) helps preserve lean mass.
Is physical activity realistic for inactive members?
Yes, especially with personalized plans that adapt to members’ lives. Even modest increases can reduce MSK risk and improve outcomes.
What should employers do today?
Download the whitepaper and explore movement-first strategies. Audit current GLP-1 spend. Look for vendors that offer outcomes-based pricing so their success is tied to measurable health improvements for your people.
Slash MSK costs and stop pain for your people
Stop wasting healthcare spend on short-term fixes and get the industry’s top validated ROI of 3.2:1.
Footnotes
Janssen, I., Shepard, D. S., Katzmarzyk, P. T., & Roubenoff, R. (2004). The healthcare costs of sarcopenia in the United States. Journal of the American Geriatrics Society, 52(1), 80–85.
Baumgartner RN et al., Obesity Research, 2004
International Foundation of Employee Benefit Plans, 2024
Baumgartner RN et al., Obesity Research, 2004