August 27, 2025 • min read
How to minimize pelvic floor treatment costs with proactive digital care
Written by

Evidence-based healthcare insights
Pelvic floor disorders (PFDs) are among the most prevalent, underdiagnosed, and expensive conditions impacting women today¹. For employers and health plans, this means hidden costs in the form of surgical claims, specialist referrals, and pharmacy spend. All of this can be mitigated with earlier, more accessible care.
Yet most care models wait until symptoms are severe to offer treatment, presenting a huge missed opportunity for employers and health insurers alike.
The key to reducing pelvic floor treatment costs lies in shifting some investment into proactive pelvic health treatment to reduce symptoms and pains early before treatment requirements and costs of intervention escalate.
In this article, we’ll explore the true cost of traditional pelvic floor care, how digital solutions like Bloom by Sword Health lower spend through proactive support, and why an outcomes-based model guarantees ROI for employers.
The high cost of reactive pelvic floor care
Pelvic floor conditions often start small. This might include leakage when laughing or discomfort while sitting. But these symptoms don’t stay small for long. Without timely support, they escalate and lead to a cascade of high-cost interventions:
- Urology consults
- Gynecologic exams and imaging
- Physical therapy referrals
- Prescription medications for pain or urgency
- Invasive surgical procedures like pelvic organ prolapse repair
This presents a massive burden for the individual and increased costs on employer-sponsored plans. According to Sword Health internal claims analysis, delayed intervention in pelvic floor disorders leads to a 4–6x increase in total treatment cost over time².
Traditional care pathways tend to be reactive, not preventive. Most women aren’t offered treatment for pelvic floor disorders until their symptoms become disruptive to daily life which is often long after they begin experiencing early warning signs. Care is typically initiated only after quality of life has been severely impacted, and at that stage, costs can escalate for medical intervention due to the acute nature of symptoms.
This reactivity stems from a range of factors. Fragmented healthcare systems often don’t screen for early pelvic health issues, and employers and health plans often don’t provide specific coverage for pelvic floor physical therapy³.
A more challenging aspect of pelvic floor conditions is the perceived cultural stigma, which can deter women from seeking care⁵. It can be uncomfortable and intimidating for women to travel to an in-person clinic and discuss intimate symptoms in a public setting⁵.
Traditional treatment pathways are hard to access
As a result, many suffer silently with bladder leakage, discomfort, or urgency for months or years without engaging care⁶. The result? Missed opportunities for early, low-cost interventions.
Instead of catching symptoms when they’re manageable, traditional care waits for them to become severe. At that point, downstream costs escalate: advanced imaging, surgical consults, and long-term medication use all enter the picture².
Women also often delay even initiating care due to embarrassment, lack of time, or difficulty accessing specialists⁵. That delay amplifies both physical and financial consequences. One study showed that more than half of women with pelvic organ prolapse had never discussed their symptoms with a clinician⁷. By the time they do seek care, surgery is often the only option.
By contrast, proactive care options provide earlier access, education, and engagement. They reduce symptom progression, prevent chronic pain, and contain costs long before claims and productivity loss spiral out of control.
Why women delay treatment (and why this increases costs)
Many women never receive timely care for PFDs. Embarrassment, lack of awareness, long waitlists, and limited provider access all create barriers.
Even when treatment is available, it's often siloed across different specialties and settings, so navigating the system can be tricky for women busy with work and family responsibilities.
Delay have a measurable impact. One study showed that more than half of women with pelvic organ prolapse had never discussed their symptoms with a clinician⁶. By the time they do seek care, surgery is often the only option on the table.
This lag in diagnosis and treatment drives up cost:
- More advanced symptoms = more complex care
- Fragmented referrals = duplicated spend
- Delayed recovery = extended time off work
Early, proactive care offers a better path.
But to make it work, care has to be accessible, private, and easy to complete.
The cost of pelvic floor dysfunction at work
Pelvic floor dysfunction can silently drive up musculoskeletal (MSK) care costs for employers, even before a formal diagnosis⁸. Symptoms that start as minor discomfort or occasional leakage can progress into more serious issues if they aren’t addressed early¹.
Pelvic floor dysfunction is one of the most costly and commonly undetected health issues affecting women in the workforce today¹. And yet, because it’s so stigmatized and difficult to talk about, the conditions often go untreated for years⁵.
For employers, this creates a hidden drain on productivity and a major risk factor for avoidable MSK spend⁴.
Traditional care pathways make it hard for women to access support. To get help, they often need to travel to a clinic, take time off work, and explain intimate symptoms in an unfamiliar setting⁴. That process can be discouraging, even intimidating, and many choose to delay care or avoid it altogether⁵.
When women can’t access care early, symptoms worsen. The longer treatment is postponed, the higher the cost of recovery becomes². Claims increase. Productivity declines. Outcomes worsen².
Digital pelvic health care breaks this cycle.
Solutions like Bloom allow women to access expert care in a private, convenient, and clinically guided format, without disruption to their schedule or personal privacy. And the results are proven.
Sword Bloom: proactive pelvic care accessible from home
Bloom is a digital pelvic health solution that enables proactive, early-stage care to address these conditions before they result in costly specialist referrals, surgeries, or long-term disability³.
Unlike reactive care models that only intervene after symptoms become severe, Bloom gives women an option to address any symptoms, pain, or feelings of discomfort from the comfort of their home.
This helps women resolve issues like urinary incontinence, prolapse, and pelvic pain in a more private and accessible way. The barriers to delaying treatment are reduced.
By offering treatment from home with expert support and biofeedback-guided therapy, Bloom empowers women to manage their pelvic health before it becomes a complex, expensive medical issue³.
Get started with Sword Bloom in 4 easy steps
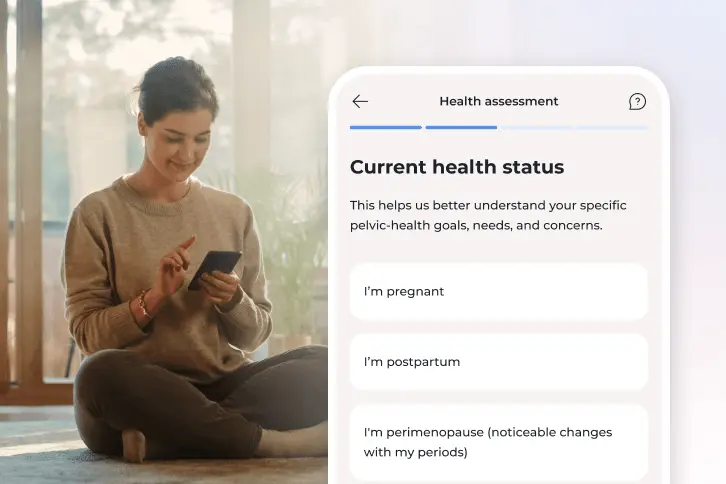
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
What makes Bloom different?
Bloom by Sword Health is a digital pelvic health program that provides early, discreet, and effective care before symptoms become high-cost claims³.
Bloom is different from traditional in-clinic PT or consult-based care:
- It is fully digital and accessible from home
- Each member is paired with a Doctor of Physical Therapy who specializes in pelvic health
- Care plans are tailored and include real-time biofeedback via the Bloom Pod device
This proactive model empowers women to address bladder leakage, pain, urgency, prolapse, and related issues early. The result? Fewer escalations to specialist care, better symptom control, and lower spend.
How Bloom reduces downstream healthcare costs
Because Bloom engages members early, it intercepts symptoms before they require invasive or expensive treatment. Sword Health’s internal data shows Bloom delivers:
- 56% reduction in presenteeism³
- 67% reduction in intent to seek additional care (e.g., surgery, further PT)³
- $3,177 average per-member per-year savings³
These savings are possible because Bloom prevents unnecessary escalation. By supporting women consistently and privately from the start, it eliminates many of the common reasons conditions spiral out of control.
Outcomes-based pricing means ROI guaranteed
Unlike traditional vendor models that charge per license or engagement, Bloom operates on an outcomes-based pricing structure.
That means Sword Health ties its reimbursement to patient improvement, not participation alone. Employers only pay when care works.
This model removes risk and aligns incentives. It also reflects Bloom’s confidence in its clinical outcomes:
- 76.1% of members report reduced anxiety symptoms³
- 54.1% report improved depression³
- 8.6/10 average satisfaction score³
For employers, this structure provides financial predictability, outcome assurance, and built-in ROI.
Proactive pelvic care is smart cost containment
Pelvic floor dysfunction is one of the most overlooked drivers of rising women’s health costs. But it doesn’t have to be.
Digital-first programs like Bloom offer a smarter solution that meets women where they are, helps them feel better faster, and lowers total spend over time.
Innovative organizations are turning to Bloom to provide stronger womens health support with measurable outcomes and proven MSK cost reductions. Make proactive pelvic part of your strategy.
Stop women suffering in silence with pelvic pain
See how Bloom's digital pelvic care plans deliver $2,276 savings per member annually while delivering clinically-proven results.
Footnotes
Janela D, et al. JMIR mHealth & uHealth. 2025; e68242.
Sword Health. Internal Claims Analysis. 2023.
Sword Health. Bloom ROI Whitepaper. 2025.
Lamin E, et al. Int Urogynecol J. 2016;17:10.
Waetjen LE, et al. Menopause. 2018;25(1):29-37.
Kołodyńska G, et al. Menopause Review. 2019;18(1):1-7.
Nygaard I, et al. JAMA. 2008;300(11):1311-1316.
Molina R, et al. Int J Gynecol Obstet. 2024;164(2):362-369.