October 20, 2025 • min read
Joint pain in perimenopause: How to prevent body aches
Learn how hormones influence joint and muscle pain during perimenopause, and what you can do to move comfortably and confidently again.
Written by

Head of Clinical Affairs, Sword Bloom
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Hormonal shifts during perimenopause affect more than your cycle—they can also impact how your joints, muscles, and connective tissue feel.
- Understanding why these changes happen helps women recognize that body aches and stiffness are common and manageable with movement, nourishment, and expert care.
Sword's Bloom program provides personalized, expert-led pelvic and musculoskeletal care to help women stay active, strong, and comfortable through perimenopause—all from home and often at no cost through their health plan.
During perimenopause familiar movements can start to feel different
Many women in their 40s notice new stiffness or soreness in their back, hips, or knees. These changes often begin gradually, showing up after sitting for long periods, during morning routines, or after light exercise.
Perimenopause is a key driver of these sensations. During this stage, estrogen and progesterone levels rise and fall unevenly¹. These hormones influence collagen production, joint lubrication, and muscle tone. As levels fluctuate, the body’s natural elasticity and recovery slow².
How hormones influence joint and muscle comfort
It's very common to experience increased sensations of body aches, joint pain, and back pain in particular during perimenopause. This is not “just aging.” These changes are part of a normal, temporary hormonal transition. Recognizing what’s happening can help you support your body with care rather than concern. There are three elements that contribute to these changes, and it's helpful to understand the science between what's happening in your body during this life stage:
1. Estrogen’s role in flexibility and joint health
Estrogen helps maintain connective tissue elasticity and joint lubrication³. As levels fluctuate, inflammation may increase, and cartilage can become less pliable, making joints feel stiffer⁴. Studies have shown that estrogen receptors exist in cartilage and muscle tissue, confirming that hormonal balance directly affects joint function⁵.
2. Muscle recovery and inflammation
Estrogen also supports efficient muscle repair and antioxidant balance⁶. When levels drop, muscles recover more slowly from exercise or strain, which can make soreness last longer. Mild inflammation may linger, contributing to sensations of tightness or fatigue. Gentle movement and consistent physical activity help counter these effects.
3. Pelvic alignment and posture
Changes in hormone levels can influence the pelvic floor and deep core muscles. When these muscles weaken or tighten unevenly, it affects posture and spinal alignment. This can create tension through the lower back, hips, and legs⁷. Supporting the pelvic floor through targeted exercises can reduce stress on surrounding muscles and improve overall comfort. Sword Bloom is designed to make this easy by giving women personalized pelvic care plans, accessible from home.
Common patterns of pain during perimenopause
It is common to notice new or changing sensations in your body during perimenopause. Some women experience mild stiffness or tenderness that comes and goes. Others notice deeper or longer-lasting aches, particularly in the back, hips, or joints. Many women move through this stage without pain at all.
Pain during perimenopause can look very different from one person to another. Hormonal fluctuations can affect muscles and joints for a few weeks or months, then ease as hormone levels stabilize. For others, these changes may linger or fluctuate throughout the transition. None of these experiences mean something is wrong; they are simply signs of your body adapting.
Because pain can have many causes, it helps to notice patterns. Perimenopausal pain often:
- Appears or intensifies during months when cycles are irregular or skipped.
- Feels like stiffness, tightness, or dull aching rather than sharp or localized pain.
- Improves with gentle movement, stretching, or warmth.
- May coincide with other changes such as fatigue, disrupted sleep, or bloating.
If you are unsure whether pain is related to hormonal changes or another cause, consider these simple steps:
- Track timing: Note whether pain patterns match your menstrual cycle or other perimenopausal symptoms.
- Assess response: Hormonal aches tend to improve with movement and self-care, while structural or acute injuries often worsen.
- Check persistence: Pain that does not fluctuate with cycles or becomes more severe over time should be evaluated by a clinician.
Understanding these distinctions helps you interpret your body’s signals with more confidence. If your discomfort is related to perimenopause, steps such as movement, nutrition, and guided pelvic and musculoskeletal care can help you stay active and comfortable.
Causes of common perimenopause pain include:
- Lower back pain: Often linked to posture changes, sleep disruption, or muscle tension.
- Hip discomfort: Caused by reduced joint lubrication and surrounding muscle stiffness.
- Knee or leg pain: Related to collagen decline, which affects shock absorption and joint cushioning.
- Generalized body aches: Driven by inflammation and changes in muscle recovery.
These experiences are common and usually temporary. Early care focused on movement and strength helps maintain comfort and flexibility.
4 ways to prevent pain in perimenopause
Understanding why your body feels different is important, but you don’t need to just accept pain and suffer in silence. You can take action and learn what you can do to reduce symptoms and retain your comfort and mobility.
Small, consistent choices around movement, nutrition, rest, and pelvic caremake a measurable difference. Each of the following habits helps women reduce inflammation, strengthen muscles, and keep joints flexible through the menopause hormonal transition.
1. Gentle, consistent movement
Daily, low-impact movement such as walking, yoga, swimming, pilates, or resistance training supports circulation, reduces inflammation, and keeps joints lubricated⁸. The goal is consistency, not intensity. Even short sessions can improve your flexibility and mood.
Sword’s Move program makes this process easy. You get a weekly movement plan tailored to your personal preferences and goals, all accessible through the Sword mobile app. You just need a 10-minute block and you can complete your Move exercise from the comfort of home.
2. Watch your nutrition and hydration
Nutrients like omega-3 fatty acids, vitamin D, and magnesium play important roles in muscle recovery and inflammation regulation⁹. These nutrients help reduce joint stiffness, support energy levels, and maintain tissue strength as hormone levels fluctuate. You can get many of these nutrients naturally through food:
- Omega-3 fatty acids: Found in salmon, mackerel, sardines, flaxseeds, chia seeds, and walnuts. They help calm inflammation and support joint flexibility.
- Vitamin D: Produced by the skin when exposed to sunlight and found in fortified dairy, eggs, and fatty fish. It helps your body absorb calcium and maintain muscle function.
- Magnesium: Present in leafy greens, almonds, avocados, whole grains, and legumes. It helps muscles relax and supports healthy nerve function.
Some women find it difficult to meet daily needs through food alone, especially for vitamin D and omega-3s. In that case, supplements can be helpful. Look for products that meet recommended daily values and are verified by independent testing (such as USP or NSF). A healthcare professional can help you determine what dosage and form are right for you.
Hydration is equally important. Water supports circulation and nutrient delivery to tissues, while limiting sugary or highly processed drinks helps reduce inflammation. Aim for small, steady sips of water throughout the day rather than large amounts at once.
3. Prioritize rest and recovery
Creating a simple, restorative bedtime routine helps the body recover and regulate hormone balance. Try these steps:
- Set a consistent bedtime and wake-up time. Going to bed and waking up at the same time each day helps your body’s natural rhythms reset.
- Reduce screen exposure. Blue light from phones or laptops delays melatonin production, making it harder to fall asleep.
- Stretch before bed. Gentle hip and back stretches or breathing exercises calm the nervous system and relax tense muscles.
- Keep the room cool and dark. Temperature regulation becomes more sensitive during perimenopause, and a cool environment promotes deeper sleep.
- Practice mindfulness or journaling. Writing thoughts down before bed or doing short guided meditations can lower cortisol levels and quiet the mind. Apart from helping your mental health, this practice can make it much easier for you to fall asleep.
If sleep disturbances continue, a healthcare professional may suggest checking hormone levels, ruling out thyroid issues, or exploring low-dose magnesium glycinate supplements, which can support relaxation. Better-quality sleep improves energy, recovery, and overall body comfort.
4. Get support from pelvic and core care
The pelvic floor is a group of muscles that form the base of your core. These muscles work together with the hips, lower back, and abdominal wall to support your posture, balance, and mobility. During perimenopause, hormonal shifts can cause these muscles to tighten or weaken unevenly, leading to hip, back, or pelvic discomfort⁷.
Improving pelvic and core strength can enhance spinal alignment and stability throughout the body. Practical ways to support these muscles include:
- Practice mindful breathing. Deep diaphragmatic breathing helps relax overactive pelvic and abdominal muscles and restores coordination between your diaphragm and core.
- Incorporate gentle strength work. Exercises such as bridges, wall sits, or supported squats activate pelvic and hip muscles safely and effectively.
- Stretch the hips and lower back. Targeted stretches improve circulation and reduce tension in connective tissues that may feel tight from hormonal shifts.
- Avoid overstraining. Movements like heavy lifting or holding your breath during effort can increase pelvic pressure; instead, exhale as you move.
Regular pelvic and core exercises relieve tension and improve balance, bladder control, and everyday stability. You can also check to see if your health plan or employer has coverage for Bloom, which provides personalized pelvic care plans supported by one-on-one guidance from a Women’s Health Specialist. These programs are customized to your body and can be done privately from home. Find even more practical pelvic health tips to help reduce pelvic floor dysfunction.
How Bloom helps women move comfortably again

Bloom is a digital women’s health solution designed to help women manage perimenopausal symptoms like joint stiffness, back discomfort, and pelvic tension.
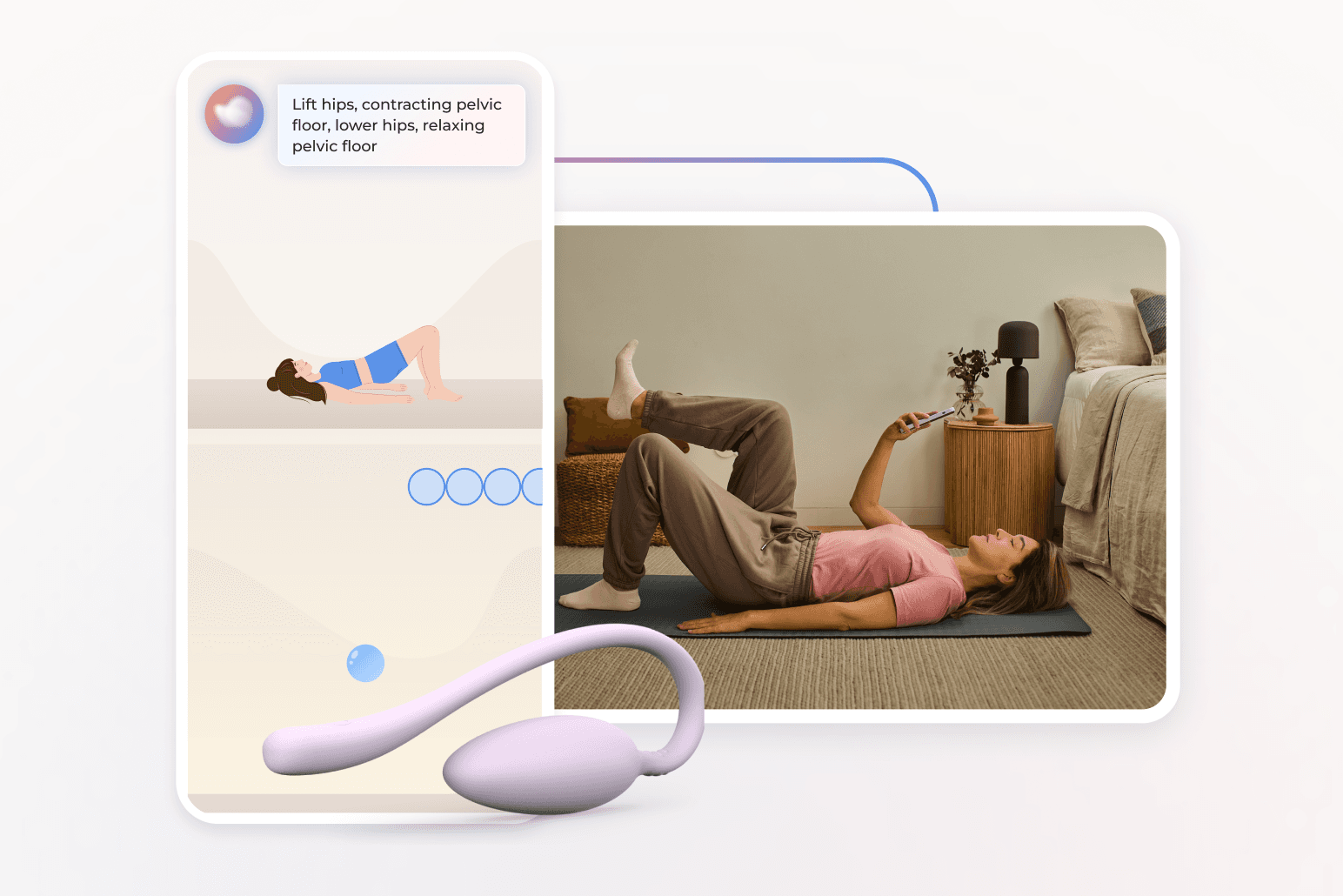
Each member is paired with a Women’s Health Specialist (Doctor of Physical Therapy) who creates a personalized care plan focused on strength, posture, and mobility. Members access short, guided sessions through the Sword Health app and use the Bloom Pod which is a safe, FDA-listed biofeedback device that provides real-time feedback during exercises.
Bloom’s outcomes demonstrate measurable improvement:
- 65% of members report meaningful improvement in daily life¹¹.
- 56% experience better productivity and 50% report reduced anxiety¹¹.
- 77% complete their programs, far exceeding in-person adherence rates¹².
With Bloom, women gain accessible, private, and expert-guided care from home, on their schedule, and at their own pace.
Accessing care from-home makes success with Bloom easy
Many women who experience joint pain or stiffness during perimenopause want help but struggle to find it. In-person pelvic and musculoskeletal specialists can be difficult to access, and appointments often require time off work or long travel times. For some, waitlists can stretch beyond 12 weeks¹³. Others may not feel comfortable discussing private symptoms in a clinic setting. Many don’t realize this kind of care even exists.
That’s where Bloom makes the difference. Bloom was created to remove the most common barriers to care by providing expert, one-on-one support from the privacy of home. Each member is guided by a Women’s Health Specialist who personalizes their program based on comfort level, progress, and lifestyle.
Bloom is designed for real life. You can complete sessions anytime, anywhere, using your phone or tablet. About half of Bloom sessions take place outside regular working hours, and nearly one in five occur on weekends¹¹. This flexibility means you can focus on your comfort and health without rearranging your schedule or missing work.
Accessibility is built into Bloom’s model. Nearly half of members live in higher-deprivation areas and still achieve the same positive outcomes as others¹⁰. Care is discreet, supportive, and adaptable, making it so much easier for women of all ages, locations, and backgrounds to strengthen their bodies and feel like themselves again. With Bloom, you don’t have to rearrange your life to prioritize an appointment within working hours. Whenever you have a spare 10 minutes, you can get started on your personalized recovery program. All you need is the Sword mobile app and your Bloom Pod.
Get started with Sword Bloom in 4 easy steps
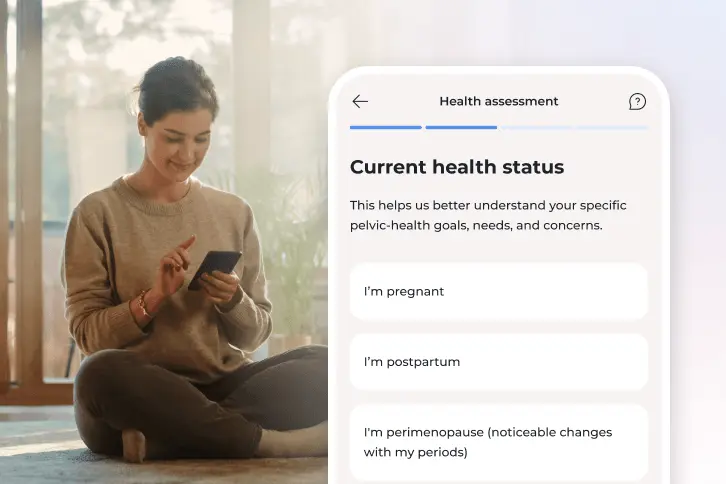
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
How to get started with Bloom to better manage your symptoms
Many employers and health plans now include Bloom as a covered benefit¹¹. You may have already coverage within your health insurance to access personalized pelvic and musculoskeletal care at no cost to you.
Checking your eligibility is simple:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Avis NE, et al. JAMA Internal Medicine. 2015;175(4):531–539. https://doi.org/10.1001/jamainternmed.2014.806
Angelou K, et al. Cureus. 2020;12(4):e7586. https://doi.org/10.7759/cureus.7586
Vina J, et al. Aging Research Reviews. 2016;26:1–7. https://doi.org/10.1016/j.arr.2015.12.008
Roman-Blas JA, et al. Arthritis Research & Therapy. 2009;11(5):241. https://doi.org/10.1186/ar2791
Tiidus PM, et al. Exercise and Sport Sciences Reviews. 2011;39(4):151–157. https://doi.org/10.1097/JES.0b013e3182297e92
Tiidus PM, et al. Exercise and Sport Sciences Reviews. 2011;39(4):151–157. https://doi.org/10.1097/JES.0b013e3182297e92
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Warburton DE, et al. CMAJ. 2006;174(6):801–809. https://doi.org/10.1503/cmaj.051351
Calder PC. Nutrients. 2021;13(1):146. https://doi.org/10.3390/nu13010146
Finan PH, et al. The Journal of Pain. 2013;14(12):1539–1552. https://doi.org/10.1016/j.jpain.2013.07.005
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Janela D, et al. Healthcare. 2024;12(2):141. https://www.mdpi.com/2227-9032/12/2/141
American Physical Therapy Association. Workforce Analysis Report: Women’s Health Section. 2023. https://www.apta.org