October 21, 2025 • min read
The ROI boost of value-based health insurance design
See how value-based insurance design and outcome-based MSK care deliver measurable ROI and better outcomes for health plans and employers.
Written by

Evidence-based healthcare insights
Healthcare costs continue to climb while clinical outcomes stagnate. Despite employers and health plans spending record amounts on musculoskeletal (MSK) care, members often cycle through unnecessary imaging, invasive procedures, and persistent pain.
Value-based insurance design (VBID) is reshaping this equation. By tying benefit design and member cost-sharing to the value of care rather than the volume of services, value-based insurance providers give enables payors and employers accountability that is otherwise lacking in the common fee-for-service health insurance model.
When paired with a outcome-based pricing, VBID becomes a measurable engine for both health improvement and return on investment (ROI).
How value-based insurance design realigns incentives
VBID emerged from research led by Dr. A. Mark Fendrick and the University of Michigan Center for Value-Based Insurance Design.
- The value-based insurance design principle is simple: remove or reduce cost barriers for high-value care, and increase cost-sharing for low-value or ineffective interventions.
This approach tackles one of healthcare’s deepest flaws, the problem of misaligned incentives when a fee-for-service (FFS) model is applied. Under FFS, providers are financially rewarded for the volume of care delivered rather than for helping people recover efficiently and sustainably.¹ This structure has been identified as a major contributor to the overuse of low-value care, unnecessary procedures, and avoidable healthcare spending.²
Traditional plan designs can also make evidence-based interventions like physical therapy or preventive care harder to access, while reimbursing low-value or reactive procedures without differentiation.³ For example, cost-sharing and reimbursement structures can sometimes discourage members from choosing high-value care like physical therapy, even when it’s clinically superior for MSK recovery.⁴
VBID flips that logic on its head, aligning incentives with evidence-based outcomes by lowering or eliminating financial barriers for high-value services and reducing payment for low-value ones.⁵
For employers and payers, this creates a structure that encourages prevention, reduces waste, and anchors every dollar spent to measurable improvement.
Why is MSK care the ideal proof point for value-based health insurance?
Musculoskeletal conditions are the number one driver of healthcare costs in the United States, exceeding $500 billion annually in combined medical and productivity losses.⁶ These disorders also produce wide variation in treatment value.
Research shows that 36% of MSK surgeries are unnecessary, and 80% of those costs could be avoided if high-quality physical therapy was used as first-line care.⁷ An estimated $90.9 billion is wasted every year on low-value MSK interventions such as avoidable surgeries and excessive imaging.⁸
The problem isn’t both clinical and structural. Under fee-for-service models, providers are paid for activity, not outcomes. VBID corrects this by rewarding early, evidence-based interventions that prevent escalation and future high-cost claims.
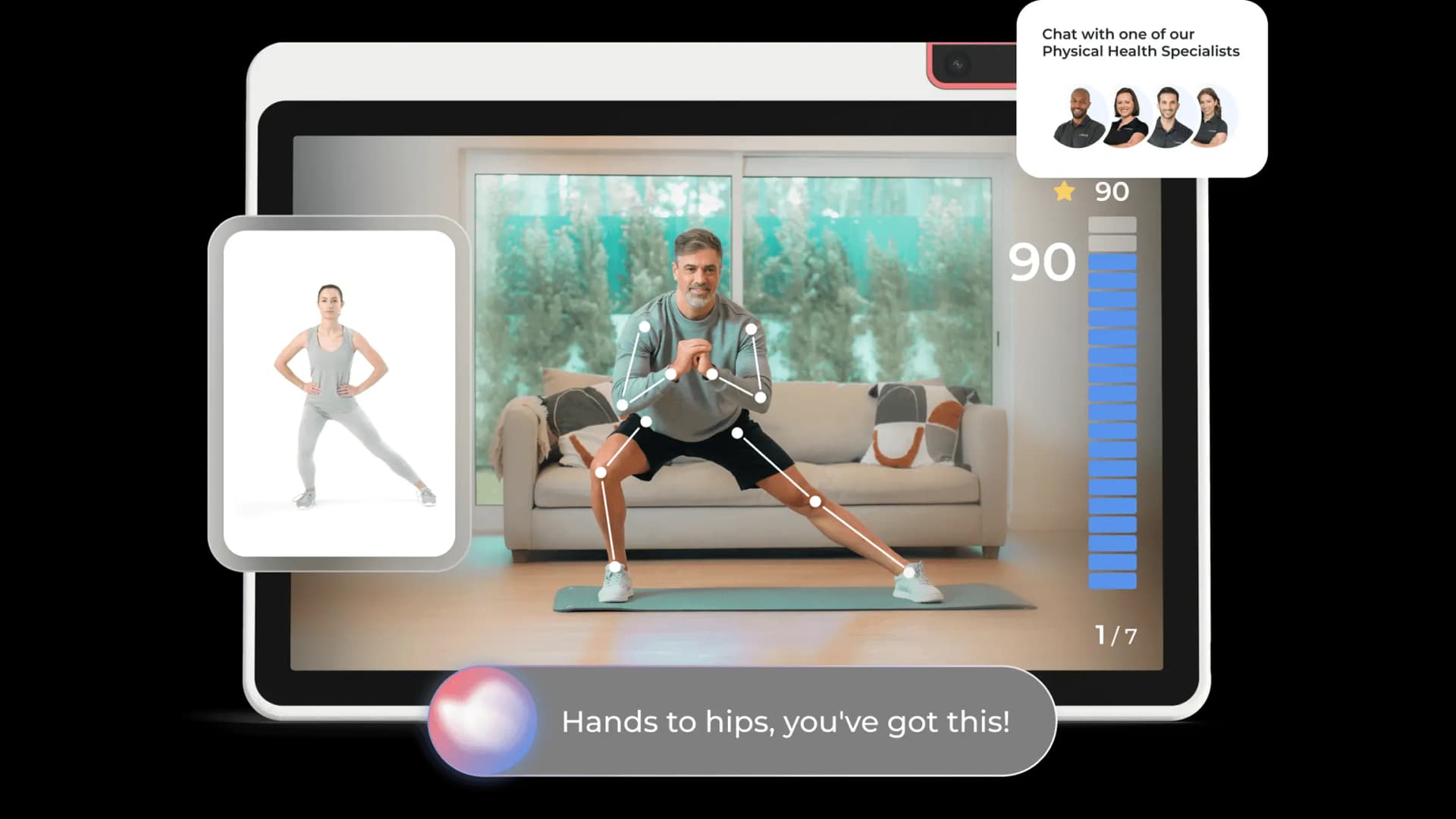
Digital MSK programs remove traditional barriers to care. Members can access expert-guided, personalized care plans, from the comfort of home. That means no travel, flexible 24/7 access, and ongoing support from a dedicated care specialist who carries a Doctorate in Physical Therapy.
All of these factors help members complete treatment plans and achieve recovery faster that with traditional in-clinic care. When access is simplified and incentives are aligned, adherence rises and outcomes improve, proving the promise of VBID in action.¹⁷ ¹⁸ ¹⁵ ¹⁹
Look for outcomes pricing when selecting healthcare vendors
Across healthcare, benefit leaders are increasingly demanding payment models that tie cost to performance. Outcome-based pricing (OBP) is emerging as one of the most credible mechanisms to ensure that payers and employers only pay for measurable health improvement.
Unlike traditional fee-for-service or subscription arrangements, outcome pricing contracts define success in advance and link payment directly to those results (whether that’s pain reduction, function improvement, or recovery milestones). This approach creates alignment across all stakeholders: members get personalized, goal-oriented care; providers are incentivized to deliver effective treatment; and payers gain predictable spend with transparent reporting.
For benefits leaders and plan sponsors evaluating digital health partners, outcome-based pricing serves as a critical trust signal. This demonstrates that a vendor is confident enough in its clinical efficacy to share financial risk. In an environment where many digital solutions still charge per user regardless of engagement or outcomes, outcome pricing separates evidence-based partners from those driven by volume or utilization.
Sword Health was one of the first digital MSK providers to formalize this approach at scale. Our Outcome Pricing model applies VBID principles directly to care delivery, ensuring payment only when members achieve real progress.
Employers and health plans only pay for activation, and for member outcomes as follows:
- 50 % of fees at activation, covering the FDA-listed hardware and individualized program setup.
- The remaining 50 % only after outcomes are achieved, defined as either member goals met or clinically meaningful improvement on the Patient Global Impression of Change (PGIC).⁹
This structure ensures that payment is aligned with real health improvement rather than utilization. It also gives employers and payers transparent, auditable insight into what they’re paying for, which is a level of accountability that fee-for-service models struggle to match.
The data to show how VBID delivers MSK care results
Empirical data shows how value-based insurance design performs when applied to MSK care. The objective: pay for interventions that deliver measurable improvement while reducing unnecessary spend. Sword’s outcomes data below illustrates how this alignment works in practice.
| Metric | Outcome | Source |
|---|---|---|
Members pain-free at discharge | 69 % | Sword Clinical Outcomes 2025¹⁰ |
Members disability-free at discharge | 65 % | Sword Clinical Outcomes 2025¹⁰ |
Reduction in costly surgeries | 50 % | Sword Clinical Outcomes 2025¹⁰ |
ROI (average per member/year) | ≈ $3,177 savings | Sword ROI Guide 2025¹¹ |
ROI in high-risk cohorts | Up to 4.4× return | Sword Predict ROI Whitepaper 2025¹² |
Absenteeism savings per member/year | ≈ $2,916 | Sword Productivity Impact 2025¹³ |
Time to first treatment | 3.8 days average | Sword Member Operations 2025¹⁴ |
Program completion rate | 81 % (vs 30–50 % for in-person PT) | npj Digital Medicine 2023¹⁵ |
How these results validate VBID principles
- Reducing barriers accelerates engagement: VBID’s premise is that lowering friction for high-value care increases participation. The 3.8-day start time and 81 % completion rate prove that when access is simple, adherence follows.
- Evidence-based care amplifies outcomes: High rates of pain relief, recovery, and surgery avoidance show that when members are steered toward evidence-based digital therapy, clinical and economic value align.
- Paying for results produces predictable ROI: Average annual savings of $3,177 per member and 4.4× ROI in high-risk groups confirm that tying payment to outcomes creates measurable financial performance—the core objective of VBID.
- Aligned incentives create shared value: Productivity recovery and absenteeism savings demonstrate that VBID’s reach extends beyond claims. When members recover faster and return to work sooner, payers, employers, and employees all benefit.
Together, these findings confirm VBID’s foundational logic: when incentives align around outcomes, not volume, both clinical and financial performance improve.
Bonus tip: Predictive analytics deliver even higher ROI rates with preventative healthcare
The next evolution of VBID integrates predictive analytics to target and prevent rising-risk claims. Sword’s innovative AI-powered Predict solution identifies members up to 40 times more likely to require surgery and reduces surgery intent by 60 % through early digital engagement.¹⁶
By linking predictive insights to benefit design (such as waived copays or immediate access for high-risk members) payers can move VBID from a static policy to a dynamic, data-driven system that intervenes before costs escalate.
GUARANTEED SAVINGS
Get the industry's highest ROI rate with Sword
$3,177 savings per member, per year
Independent validation shows Sword reduces MSK costs by $3,177 per member annually
3.2:1 validated ROI ratio
Sword's delivers average MSK healthcare savings of over 3x
50% reduction in costly surgeries
Sword halves the number of costly MSK surgeries and related claims
39% fewer lost workdays from MSK pain
Sword members report significantly fewer absences, reducing productivity losses
Start using value-based insurance design as your competitive advantage
As healthcare purchasing shifts toward performance accountability, VBID offers payers and employers a strategic edge:
- Predictable spend: outcome-linked contracts minimize financial volatility.
- Regulatory alignment: CMS and CMMI now reward value-based contracting readiness.
- Employer confidence: self-insured buyers increasingly demand results-based vendors.
- Member loyalty: transparent, cost-aligned benefits improve satisfaction and retention.
Embedding VBID within MSK benefits positions organizations as leaders in modern, results-driven care financing. The success of VBID in MSK care demonstrates that the model is no longer theoretical. Instead, you can partner with value-based care providers to realise cost savings at enterprise scale.
If you’re ready to turn MSK care from a cost center into a strategic asset, request a demo and a Sword expert will walk you through the solutions you can add to improve your MSK healthcare offering.
Start saving $3,177 per member per year
Slash MSK costs for your health plan and get the industry’s top validated ROI of 3.2:1.
Footnotes
Porter ME, Lee TH. The strategy that will fix health care. Harvard Business Review. 2013. https://hbr.org/2013/10/the-strategy-that-will-fix-health-care
Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. https://doi.org/10.1001/jama.2012.362
Agency for Healthcare Research and Quality (AHRQ). Reducing Low-Value Care: The Role of Payment and Delivery Reform. 2020. https://www.ahrq.gov/workingforquality/reports/lowvalue.html
Friedly JL, et al. Impact of a value-based insurance design for physical therapy to treat back pain. Journal of Pain Research. 2021;14:2957–2965. https://doi.org/10.2147/JPR.S317286
University of Michigan Center for Value-Based Insurance Design. Value-Based Insurance Design: Better Health Through Smarter Deductibles. 2022. https://ihpi.umich.edu/sites/default/files/ihpi-vbid.pdf
Dieleman JL, et al. Tracking US health care spending by health condition and county. JAMA. 2020;323(9):863–884. https://doi.org/10.1001/jama.2020.0734
Sword Health. The MSK Money Pit Report. 2024. https://swordhealth.com/landing/msk-money-pit
Sword Health. Low-Value Care Analysis. 2024.
Sword Health. Outcome Pricing Overview. 2024. https://swordhealth.com/newsroom/outcome-pricing
Sword Health. Clinical Outcomes Summary. 2025. https://swordhealth.com/resources/clinical-studies
Sword Health. ROI Guide. 2025. https://swordhealth.com/insights/reports-and-guides
Sword Health. Predict ROI Whitepaper. 2025. https://swordhealth.com/insights/reports-and-guides/sword-predict-roi
Sword Health. Productivity Impact Report. 2025. https://swordhealth.com/insights/reports-and-guides/productivity-impact
Sword Health. Member Operations Data. 2025.
Correia R, et al. Digital PT engagement and outcomes. NPJ Digital Medicine. 2023;6:121. https://doi.org/10.1038/s41746-023-00811-x
Sword Health. Predictive MSK Care: How to Unlock a 3.7× ROI. 2025. https://swordhealth.com/insights/reports-and-guides/sword-predict-roi
Bini SA, et al. Digital health interventions for musculoskeletal pain: systematic review and meta-analysis. NPJ Digital Medicine. 2022;5(1):97. https://doi.org/10.1038/s41746-022-00642-0
Cottrell MA, et al. Adherence to telehealth-delivered exercise therapy for musculoskeletal conditions: systematic review. Journal of Telemedicine and Telecare. 2021;27(8):510–523. https://doi.org/10.1177/1357633X20904094
Mani S, et al. Effectiveness of internet-based exercise therapy for chronic musculoskeletal pain: systematic review and meta-analysis. Pain Physician. 2021;24(5):E485–E499. https://www.painphysicianjournal.com/current/pdf?article=NzU1Nw%3D%3D&journal=148