August 20, 2025 • min read
Weight loss drugs and muscle loss: MSK risks to avoid
Written by

Head of Clinical Strategy, Sword Move
Weight loss drugs are rewriting the obesity care playbook. GLP-1s like semaglutide, liraglutide, and others are helping members lose weight, improve metabolic markers, and avoid high-risk interventions like surgery.
Many employers and health plans have fast-tracked these medications into formularies as a cornerstone of chronic condition management. But there’s one effect that most treatment programs overlook and it’s not related to fat loss. It’s about muscle loss.
Clinical data shows up to 39% of lean body mass is lost during GLP-1 usage.¹ Muscle loss is linked to increased fatigue, a higher risk of falls, MSK conditions, and costly downstream care.
A silent risk in your obesity care strategy
This isn't just an unfortunate side effect. It’s a systemic risk factor that can increase falls, injuries, chronic pain, and long-term musculoskeletal (MSK) claims. Worse, muscle loss often flies under the radar. It’s not coded, rarely discussed, but relatively easy to prevent, even at scale over a large member population. For forward-thinking benefit leaders, this is a crucial blind spot to address.
Most anti-obesity medications work by suppressing appetite or altering satiety signals. Whether it's semaglutide (GLP-1), phentermine/topiramate (Qsymia), or bupropion/naltrexone (Contrave), the result is a significant calorie deficit.
That deficit drives weight loss but it doesn’t tell the body to preserve muscle. Unless a member is consistently engaging in muscle-preserving physical activity, their body sheds both fat and lean mass. This is especially problematic because most GLP-1 candidates already start out inactive: fewer than 1 in 4 U.S. adults meet the CDC’s recommended activity guidelines.² In other words, the majority of weight loss drug users may be losing strength along with weight and entering a physically deconditioned state.
Lean muscle loss is a dangerous side effect of GLP-1 weight loss drugs
Muscle isn't just about movement:
- Supports joint integrity and spinal alignment¹¹
- Powers metabolism, burning more calories even at rest¹²
- Prevents falls and injuries⁴
- Enables independence in daily living³
When muscle mass declines:
- Balance worsens, fall risk increases⁴
- Joint pain becomes more common as muscles fail to support the skeleton³
- Recovery slows following injury or illness³
- Energy drops, reducing adherence to positive behavior change³
Muscle loss changes the risk profile of a member’s health, even if the scale shows an objectively positive result of weight lost. Employers and health insurers need to look beyond this weight loss number and support weight loss treatment plans with structured movement programs to retain lean muscle mass.
The MSK claims you don’t see coming
Muscle loss doesn’t appear in a line item on your claims dashboard. But its impact is there, just delayed, and disguised. Clinical research shows that muscle loss (sarcopenia):
- Drives 33% of chronic pain in older adults³
- Increases fall risk by 60%, even among younger inactive adults⁴
- Raises disability risk by 2.5x when combined with obesity (sarcopenic obesity)⁵
And when members on weight loss drugs lose muscle, the signs don’t show up in weight management metrics. They show up in the months and years after treatment in the form of musculoskeletal issues that require significant (and expensive) medical intervention:
- Joint pain and mobility complaints
- Fall-related injuries and ER visits
- Referrals to orthopaedic specialists
- Slower return-to-work after minor incidents
- Increased pain medication use
Even though GLP-1 patients see short term weight loss results, the lurking risk factor of sarcopenia (lean muscle loss) may quietly become an escalating MSK cost driver.
Who’s most at risk of muscle loss during weight loss?
The muscle loss effect isn’t evenly distributed. The following groups are especially vulnerable to sarcopenia:
- Infrequently active members: most GLP-1 users fall into this group
- Adults over 40: natural sarcopenia in middle and older age amplifies the risk
- Desk-based workers: sedentary time increases lean tissue degradation
- Those with chronic MSK pain or injury history: weakened muscles accelerate recurrence
- Women post-menopause: hormonal shifts reduce muscle preservation capacity
These populations often overlap with high-prescription segments meaning muscle loss is a common risk for weight loss patients considering GLP-1 usage. The solution is prevention.
By partnering GLP-1 weight loss drug treatment with structured movement plans, you can help patients retain and even increase their strength. Prescribed physical activity will help inactive people with positive behavior change, developing regular exercise habits that can be sustained after treatment ends.
Prescribe structured movement alongside GLP-1 weight loss drugs
Supplements aren’t the answer. You can’t count on nutrition alone. Advice on healthy physical activity also doesn’t create behavior change at scale. The only proven way to preserve muscle during weight loss is structured, strength-based movement, delivered early and consistently. Movement isn’t just a helpful addition to consider for GLP-1 users. Prescribed physical activity is a clinical protection mechanism.
Movement + medication is part of the GLP-1 prescribing guidance
What we’re suggesting isn’t just good practice, it’s standard protocol. GLP-1 medications like semaglutide are only approved for weight management as an adjunct to a reduced-calorie diet and increased physical activity. That’s not a recommendation. The manufacturers of GLP-1s advise supporting movement programs to retain lean muscle mass.⁶
Yet despite this, many patients start treatment without any structured movement plan, putting them at high risk of lean muscle loss, slower progress, and weight regain. Sword Move helps close that gap with clinical-guided activity plans designed to support the success the prescription started.
Structured physical activity:
- Preserves lean muscle mass to support metabolism
- Reduces fall and injury risk by strengthening stabilizing muscles
- Builds habits that help members transition successfully after discontinuing medication
Healthcare providers can proactively embed movement into a GLP-1 weight loss care model to prevent the dangerous side effect of lean muscle loss before it becomes a downstream cost driver. That’s exactly what Sword’s Move solution is designed to do.

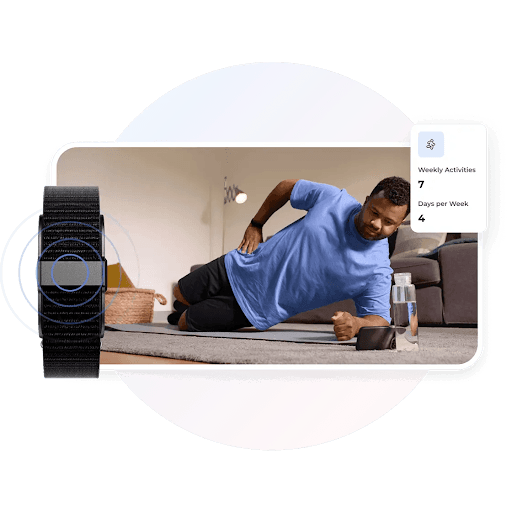
Sword Move: Clinical movement that multiplies impact
Sword Move is a digital, clinically-guided movement solution designed to support GLP-1 prescriptions and reduce the risk of lean muscle loss. Move directly protects against the risks that standalone GLP-1 strategies leave behind.
You can simply prescribe a Move program to each GLP-1 patient with the confidence of established, clinically validated results. You also get the reassurance of Sword’s outcome-based pricing where payments are tired to each individual’s specific healthcare targets.
That means you only pay when members achieve real, clinically significant improvements. No more paying for unused sessions or flat fees that don’t guarantee results.
- Ongoing support from expert physical therapists
- Real-time wearable tracking (with your own Apple Watch, Fitbit, or a Sword Move wearable included in program)
- Adaptive weekly movement plans, tailored to members’ jobs, needs, and lifestyles
- Feedback loops to keep accountability, evolve care, and maintain engagement
Sword Move’s proven results
- 69% of “inactive” and “insufficiently active” members reach “active” or “healthy active” status within 10 weeks⁷
- 91% of members reported feeling moderately or much better⁸
- Sedentary time reduced by 1 hour 22 minutes per day for previously “inactive” or “insufficiently active” members⁹
- 4.5 sessions/week completed on average¹⁰
Sword Move offers personalised movement support delivered at scale to drive proven positive healthcare outcomes. These are not just engagement metrics, they’re leading indicators of reduced MSK risk and improved resilience post-weight loss.
GLP-1s initiate change. Move makes it last.
GLP-1 medications are not the problem. The medication alone does not cause lean muscle loss. Inactivity is the danger, but prescribing Move protects against the risk. Without movement, members lose muscle, resilience, and long-term value. Sword Move is the multiplier, protecting muscle, building positive physical activity habits, and amplifying positive health outcomes. If you're offering GLP-1s, Move helps you protect your members and drive lasting success.
Stop your healthcare spend leaking away
Invest in the healthcare platform that predicts, prevents, and eradicates pain with guaranteed return on investment.
Footnotes
Prado, Carla M. et al. The Lancet Diabetes & Endocrinology, Vol. 12, Issue 11, 785–787
NCHS Data Brief No. 443, CDC. https://dx.doi.org/10.15620/cdc:120213
Hicks GE et al., Pain Medicine, 2004;5(2):125–134
Sousa AS et al., Clin Nutr ESPEN, Aug 2022; 50:63-73
Baumgartner RN et al., Obesity Research, 2004
Novo Nordisk Limited. (2024). Wegovy 2.4 mg solution for injection in pre-filled pen – Summary of Product Characteristics. Electronic Medicines Compendium. https://www.medicines.org.uk/emc/product/15481/smpc
Sword Health. PGIC scores, Sword database (2023–2024). (Internal data)
Sword Health. PGIC scores, Sword member base (2023–2024). (Internal data)
Sword Health. Member reassessment data (5+ weeks into program). (Internal data)
Sword Health. Move Book of Business, H1 2024. (Internal data)
NCBI Bookshelf. Exercise and Physical Activity: Benefits for the Musculoskeletal System. https://www.ncbi.nlm.nih.gov/books/NBK558997/
Wolfe RR. The underappreciated role of muscle in health and disease. Am J Clin Nutr. 2006;84(3):475–482