October 22, 2025 • min read
TENS machine (TENS unit): What is it and how does it work?
Learn TENS machine (TENS unit) basics: what it does, side effects, safety tips, and advice to help you understand when movement-based rehab is needed.
Written by

Director, Clinical Specialists
TENS stands for transcutaneous electrical nerve stimulation. TENS is a type of pain-relief therapy that uses low-voltage electrical current. A TENS machine (also called a TENS unit or TENS device) sends gentle electrical pulses through electrode pads placed on your skin to help reduce pain temporarily.
TENS devices may help reduce pain intensity while in use, but evidence does not support them as a treatment for the underlying causes of pain or long-term recovery.¹
If you’re deciding whether to try one, this guide will help you understand what to expect, how to use a TENS unit safely, how to treat the cause of the pain, and what to do when pain keeps coming back.
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- A TENS machine can lower pain intensity during or right after use for some people, but results vary.¹
- It’s commonly used for short-term relief of conditions like back pain, osteoarthritis, tendinitis, fibromyalgia, and more often as a “helper,” not a standalone plan.¹
- Most side effects are mild, with skin irritation and uncomfortable tingling being the most common.¹⁴
- Not everyone should use TENS (for example: pacemakers/implants, pregnancy, epilepsy, certain heart conditions).¹⁴⁵
- For longer-term improvement, movement-based rehab (like physical therapy) targets the strength, mobility, and habits that often drive recurring pain.⁶
What is TENS?
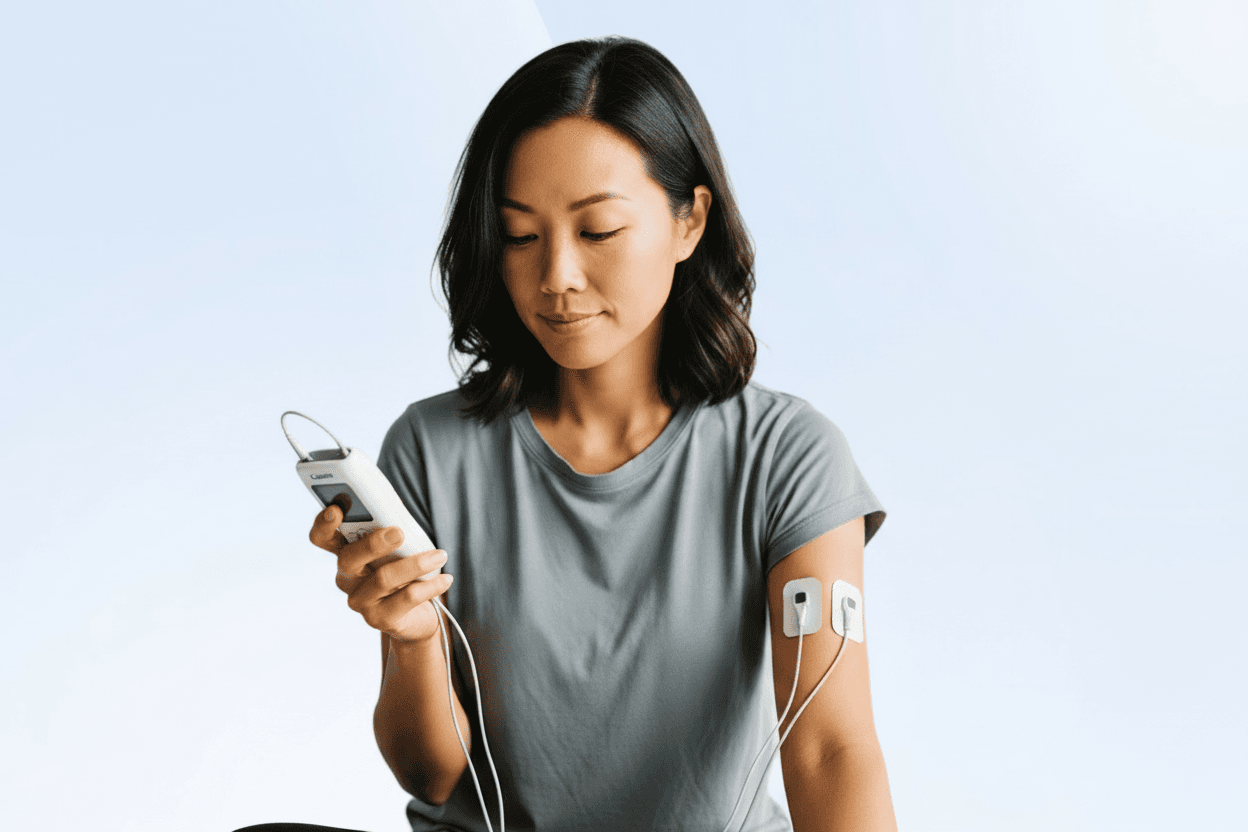
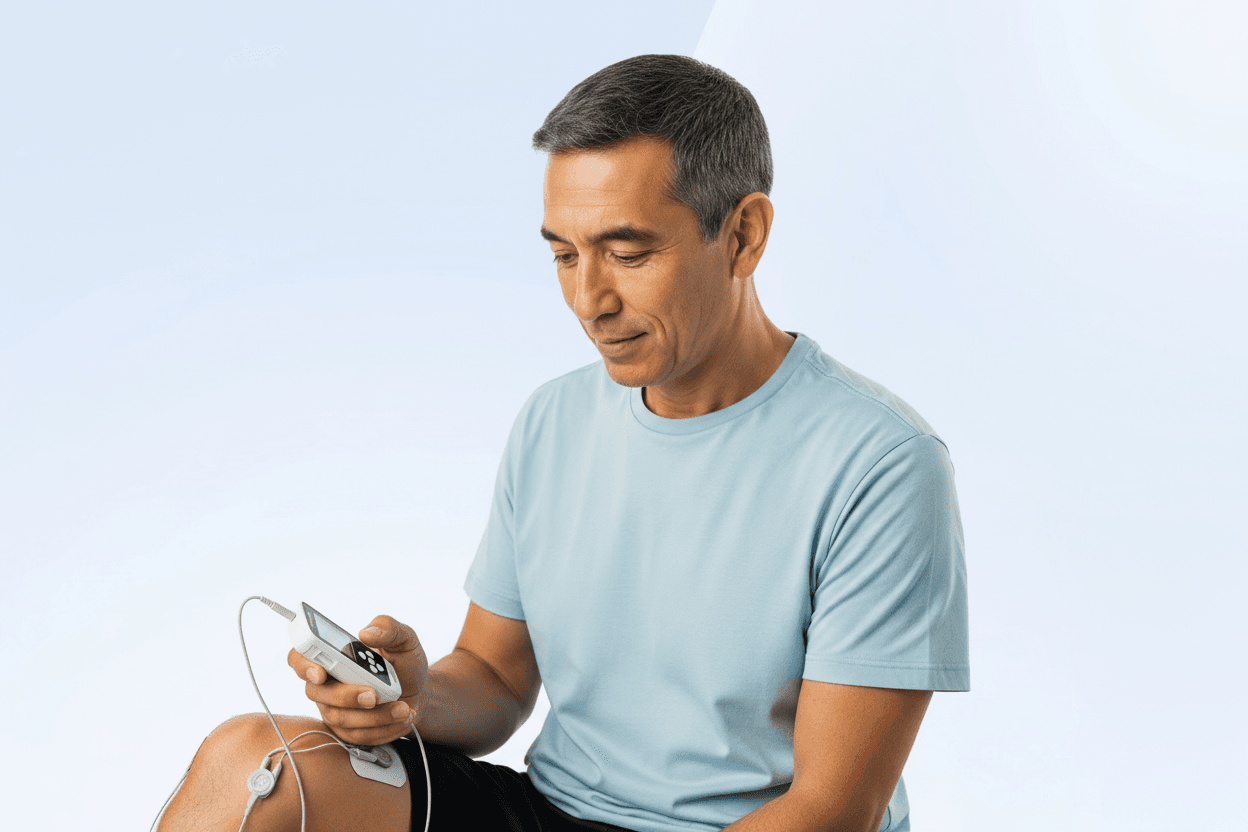
TENS stands for transcutaneous electrical nerve stimulation (often written as T.E.N.S.) and nvolves non-invasive electrode pads placed on the skin. These patches deliver mild electrical pulses to stimulate sensory nerve roots. By doing so, the therapy aims to reduce or “distract” pain signals as they travel to the brain. People often refer to the TENS device and accompanying treatment patches as a TENS unit or a TENS machine.
For more than 50 years, transcutaneous electrical nerve stimulation (TENS) therapy has been used as a non-pharmacological way to manage pain. Traditionally, a TENS device was offered as a method of reducing pain while it was in use.
What is a TENS unit?
A TENS unit is a small, battery-powered device designed to deliver low-voltage electrical impulses through adhesive electrode pads placed on the skin. Often called a TENS machine, this device is used to provide temporary pain relief by stimulating the nerves near the area of discomfort and interfering with the way pain signals are sent to the brain. While TENS units can help mask pain during use and are widely available over-the-counter and in clinical settings, they do not treat or resolve the underlying issue that triggers the pain.
This type of tens nerve stimulation is designed to provide temporary pain relief, working while the device is active. Like opioids and other symptom-based pain relief approaches, TENS can mask pain rather than address its underlying cause.TENS can mask pain symptoms rather. TENS units are not intended to repair injury or tackle the root cause of pain. Despite its widespread availability, TENS has significant limitations.
What do TENS units do?
TENS units send low-voltage electrical impulses through electrode pads on your skin. Those impulses may block or change pain signals traveling to your spinal cord and brain, and may also increase endorphins (your body’s natural pain-relieving chemicals). The result is usually a strong-but-comfortable tingling sensation and, for some people, less pain.¹⁴
Pain is both a “damage alarm” and a protection system influenced by your nervous system, your movement patterns, and your context. That’s why two people can have the same MRI and wildly different pain. A TENS machine works at the signal level. It doesn’t realign a joint, strengthen a muscle, or retrain movement habits, but it may help lower the volume enough so that you can move more comfortably.
Movement is critical for physical therapy and for recovering from pain and musculoskeletal (MSK) problems, so TENS units can sometimes be helpful additions to a rehab program.
How does a TENS unit work?
The process is relatively simple:
- Small adhesive electrodes are placed on the skin near the area of discomfort.
- The device generates low-voltage electrical currents that pass through the skin.
- These impulses stimulate nerves in the targeted region.
- The goal is to temporarily block or alter the transmission of pain signals to the brain, creating a perceived reduction in pain.
While this mechanism may temporarily relieve discomfort, it does not heal or treat the pain or its cause. Unlike physical therapy, which focuses on restoring mobility and strength, TENS works only while the device is turned on.
Do TENS units help to cure pain?
TENS therapy aims to reduce pain while the device is in use. Neither chronic nor acute pain can be solved by intermittent periods of relief. TENS machines don't help to resolve or cure pain as they do not address the trigger or cause.1
Clinical studies suggest that electrical stimulation may trigger the release of endorphins and interfere with pain signal transmission. This means some people experience short-term relief while using the device. Commonly, TENS therapy has been tried for:
- Low back pain
- Neck pain
- Arthritis
- Post-surgical pain
- Labor-related pain
However, TENS units do not treat the root causes of chronic or acute pain. Relief disappears once the device is turned off, which limits its usefulness for MSK conditions and injury recovery.1 Chronic pain and acute injuries cannot be resolved with short bursts of electrical stimulation. Because the therapy doesn’t address biomechanical dysfunction, inflammation, or behavioral factors that drive MSK pain, the underlying condition persists.
At Sword Health, we understand that solving pain requires habit-forming, guided movement, and the expertise of licensed physical therapists. That’s why TENS therapy is excluded from our care model.
Does Sword Health’s MSK programs use TENS?
At Sword Health, we focus on evidence-based treatment to deliver meaningful improvement, which means we rely on clinical results and science to deliver only the most appropriate and effective care for our patients.
We believe in a high-touch model of physical care, delivered by a team of licensed doctors of physical therapy. Their expertise, combined with sensor-based technology, is the best way to heal long-term. Because of our philosophy, we make the conscious choice to avoid TENS therapy in our approach.
End your pain with Sword Thrive
Recover faster from the comfort of home with Thrive's clinically-proven digital physical therapy plans.
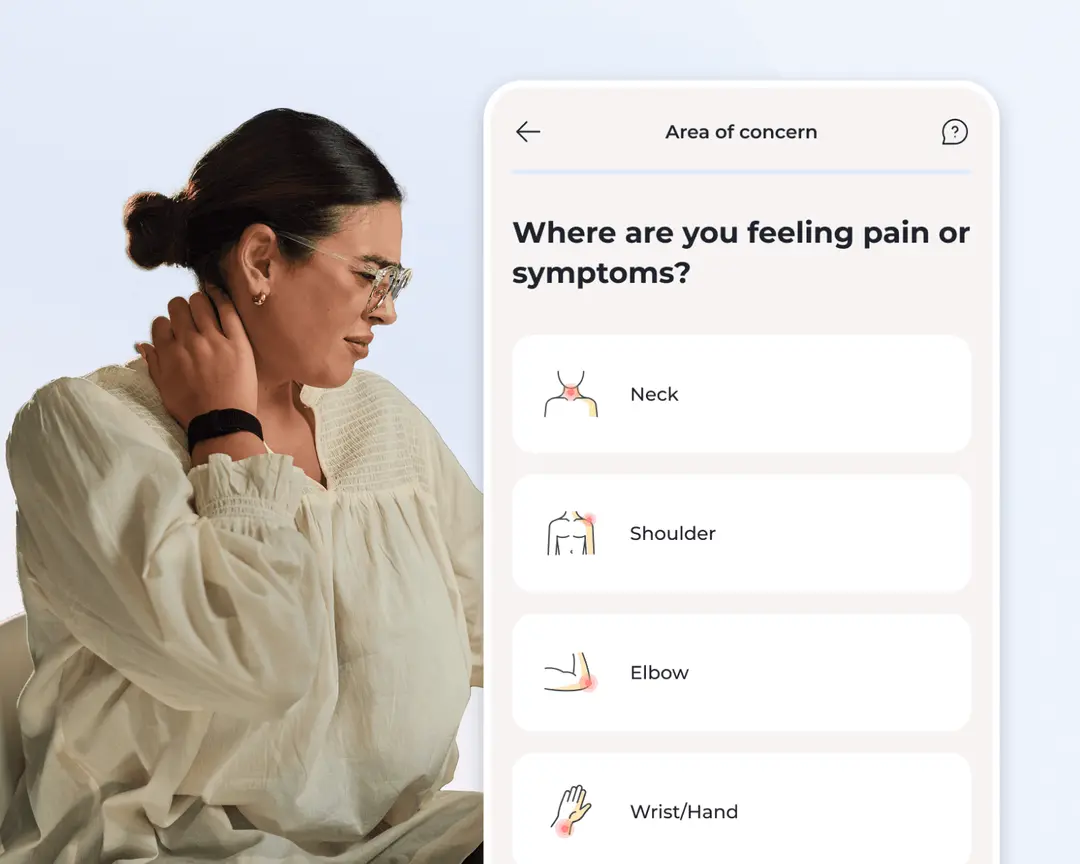
1. Tell us about you
Share where you’re feeling pain, your medical history, and your lifestyle so we can tailor your care from the start.
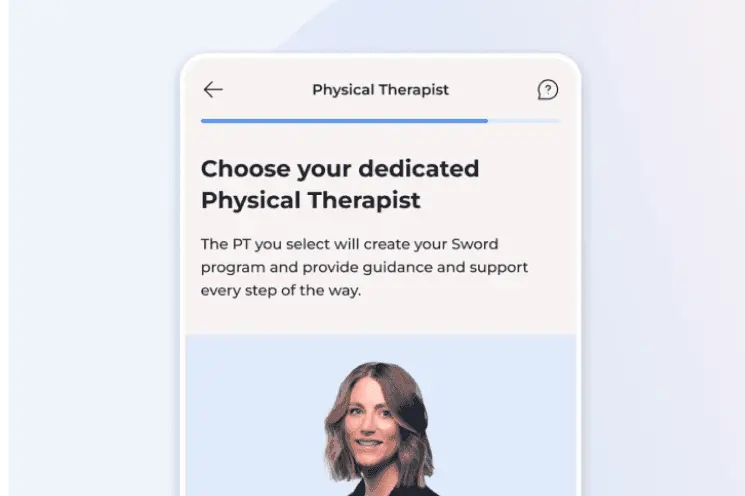
2. Choose your clinician
Pick your dedicated Doctor of Physical Therapy. They will guide your recovery and adjust your plan as you progress.

3. Receive your FDA-listed Thrive kit
We send your Thrive Pad (or motion sensors for certain conditions), equipped with AI motion tracking for real-time feedback
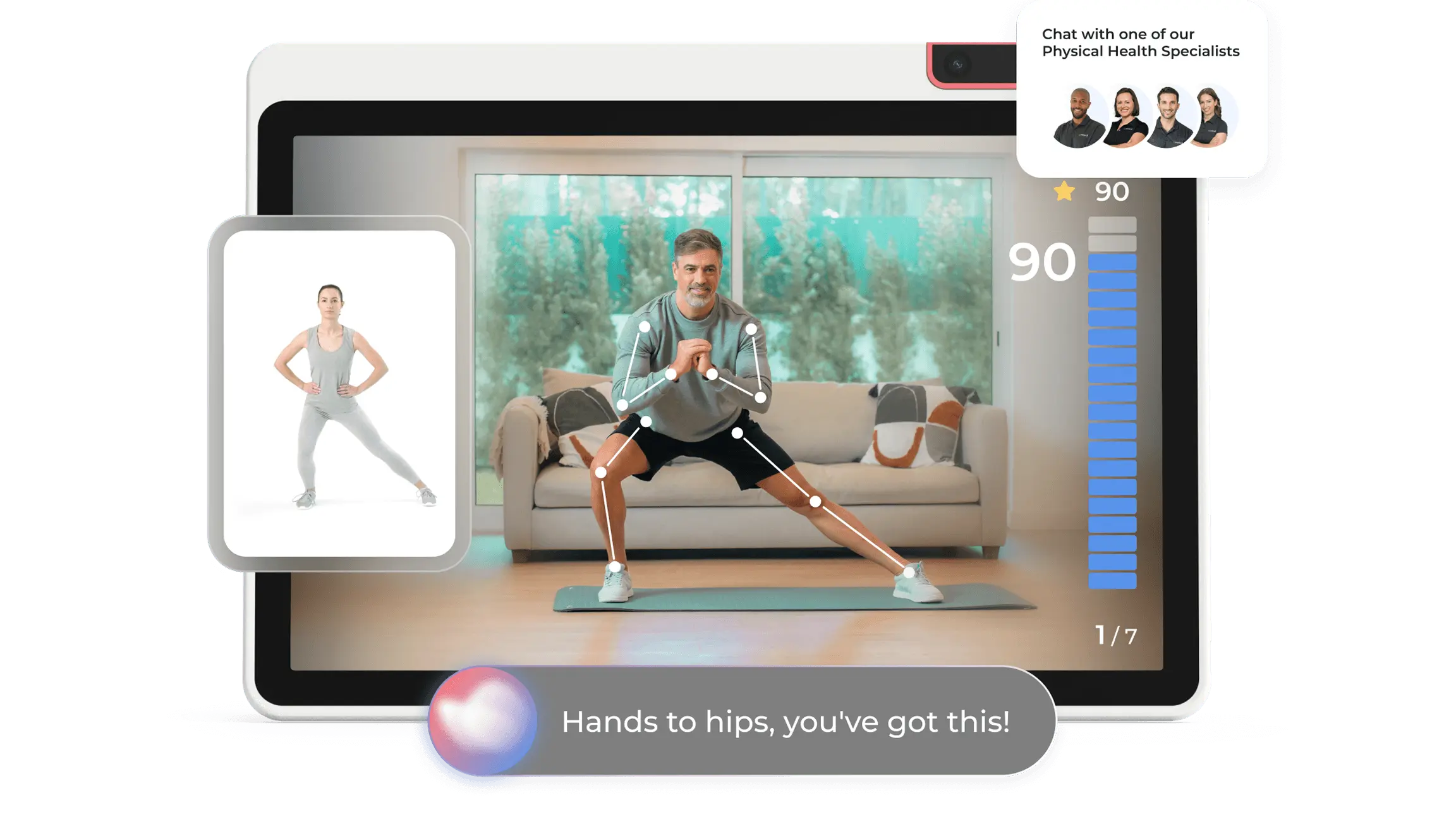
4. Recover from home at any time
Follow guided sessions at home with real-time feedback, and support from your matched Doctor of Physical Therapy.
High vs Low Frequency TENS
TENS therapy can be delivered at different frequencies, intensities, and pulse durations. Initially, devices used low-frequency stimulation. More recently, some MSK providers have experimented with high-frequency impulse therapy (HFIT), suggesting it may outperform low-frequency stimulation.
But here’s the problem: current evidence does not support this claim. While high-frequency implantable spinal cord stimulators have shown promising results, the same has not been validated for transcutaneous stimulation.
In fact, the only published study upon which solutions such as Enso have based their approach is exploratory. In this study, high-frequency stimulation was compared with no stimulation. Since the HFIT results in impulses that the member can feel (versus no stimulation), it is impossible to note placebo effects. Studies around high versus low frequency TENS have focused solely on chronic low back pain, with no evidence on acute pain, or on pain affecting other areas of the body, and significant methodological limitations.¹ ⁶
MSK solutions should be validating their care models against clinical-grade studies and results, and with the lack of clinical validation around TENS, Sword has chosen to avoid incorporation into our care model.
The problems and limitations of TENS vs physical therapy
Through the years, multiple efforts to conclude on the efficacy of TENS for acute or chronic pain have taken place, with over 160 systematic reviews and 50 meta-analyses conducted so far. With all of this, the efficacy of TENS remains unclear. While many studies show positive effects, others state negative effects, and several systematic reviews conclude that there is insufficient evidence.
In relation to MSK conditions, TENS studies have focused on chronic low back pain and neck pain, but the question of its effectiveness still remains. There is currently no consensus on its clinical worthiness.
As a result, TENS is not suggested by clinical guidelines for the management of chronic low back pain (most importantly, the American College of Physicians / American Pain Society guidelines and the NICE guidelines). Additionally, the Centers for Medicare and Medicaid CMS issued a Medicare National Coverage Determination (NCD) in 2012 that allowed for coverage of TENS for chronic low back pain, only in the context of clinical trials. Since then, this coverage has expired, which has led several health plans to stop reimbursing for TENS therapy.
Most importantly, TENS does not address the underlying root causes of MSK pain, nor has it been proven to produce long-term relief. Evidence-based MSK care stresses that non-pharmacological approaches should be the mainstay treatment in MSK conditions. For solutions with the best outcomes, education, therapeutic exercise and behavioral change are driving care.
Is TENS use safe or can it be harmful?
While TENS is generally considered safe, risks and side effects exist:
- Skin irritation or rash at electrode sites
- Tingling or uncomfortable buzzing sensations
- Muscle spasms
- Increased tolerance (requiring stronger settings over time)
For many people, TENS is considered safe when used correctly, but it’s not for everyone. You should avoid using TENS units if:
- you are pregnant (or ensure you get medical advice first)
- you have an implantable device like a pacemaker
- you have conditions such as epilepsy or heart disease/heart problems
- Make sure you don’t use it in the bath/shower or while driving.
Much like opioids, you can develop tolerance to TENS, rendering it ineffective when frequently used. Make sure you stop using the device if you experience nerve pain of any kind.
Safe use depends on where you place the TENS pads, what intensity you use, and what you’re doing while it’s on. Both NHS guidance and major clinical resources caution against using TENS on sensitive areas (like the front/side of the neck), over damaged skin, or near the heart/chest.¹ ⁴ ⁵
And while it’s tempting to treat a TENS unit like a “set it and forget it” gadget, it’s meant to be used with attention. Some guidance recommends limiting sessions to less than an hour and staying awake while it’s running.⁴
Quick TENS safety checklist
- Start low and increase until it feels strong but comfortable, not painful.⁴
- Don’t place electrodes over broken/irritated skin, and watch for redness.⁴ ⁵
- Don’t use a TENS machine in water or while driving/operating machinery.⁴ ⁵
- If you have medical conditions (especially cardiac or neurological), get clinician advice first before considering TENS use.¹ ⁴ ⁵
- If pain is severe, progressive, or paired with red flags (chest pain, shortness of breath, fainting, sudden weakness), skip the device and seek urgent care.
TENS helps dull pain, but Sword treats the cause of the pain
A TENS unit can be useful when pain is loud and you need it quieter, especially if you’re trying to sleep.
But if pain keeps returning, the long game usually looks like improving mobility, building strength, and changing the habits that keep your nervous system on high alert. That’s the heart of physical therapy and it’s why many people do best when symptom tools (like TENS, heat/ice, pacing) are paired with a progressive rehab plan.
If you’re looking for guided, movement-based care from home, Sword offers AI-powered physical pain care with licensed clinicians through Sword Thrive.
Musculoskeletal conditions are the leading cause of disability in the U.S. and one of the most expensive healthcare burdens. Evidence consistently shows that sustainable recovery comes from:
- Therapeutic exercise guided by experts
- Education that empowers individuals
- Behavioral change that supports long-term health
Sword's programs deliver all three. We offer the most clinically-effective digital solution for MSK disorders with high-quality, personalizaed physical therapy plans delivered by licensed doctors of physical therapy combined with our FDA-listed devices and supporting AI technology.
Unlike TENS, Sword’s program is designed to address the physical and mental barriers to long-term pain relief.
Recover from home with clinically-proven care
Sword’s digital physical therapy programs may already be covered in your health plan at $0 cost to you.
Footnotes
Cochrane Database Syst Rev. 2018;10(10):CD005654. doi:10.1002/14651858.CD005654.pub4
National Health Service (NHS). Transcutaneous electrical nerve stimulation (TENS). https://www.nhs.uk/tests-and-treatments/transcutaneous-electrical-nerve-stimulation-tens/
Cleveland Clinic. Transcutaneous electrical nerve stimulation (TENS).https://my.clevelandclinic.org/health/treatments/15840-transcutaneous-electrical-nerve-stimulation-tens
Qaseem A, et al. Ann Intern Med. 2017;166(7):514–530. ACP Clinical Guidelines.
National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. 2020.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for TENS for Chronic Low Back Pain (160.27). 2012.
Musculoskelet Sci Pract. 2023;63:102709. doi:10.1016/j.msksp.2022.102709
JAMA. 2020;323(9):863–884. doi:10.1001/jama.2020.0734