October 20, 2025 • min read
How pelvic care can help with cramps during perimenopause
Learn what causes cramps during perimenopause, how to manage discomfort safely, and how pelvic care with Bloom can support your comfort and confidence.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Hormonal changes during perimenopause can cause new or stronger cramps.
- Paying attention to your body’s signals helps you manage discomfort and know when to seek guidance.
- Bloom offers expert pelvic care that helps women feel stronger, more comfortable, and supported from home.
Familiar cramps can start to feel different in perimenopause
You might notice that the cramps you have always had are changing. They may last longer, appear between periods, or feel sharper than before. Many women experience these shifts in the years leading up to menopause.
Perimenopause can begin in your late 30s or early 40s. During this time, estrogen and progesterone levels rise and fall unevenly¹. These hormonal changes influence your uterus, ovaries, and muscles, which can lead to more noticeable cramps or bloating².
It is understandable to feel concerned when your body behaves differently. While these sensations are common, you do not need to tolerate them in silence. Understanding what is happening is the first step to finding relief and staying comfortable.
Why cramps change during perimenopause
It's very common to experience increased sensations of body aches, joint pain, and stomach cramps during perimenopause. This is not “just another part of aging" that you simply have to accept and suffer through. Changes in the way you experience cramps can be a part of a temporary hormonal transition that occurs during perimenopause. Recognizing what’s happening in body can help you understand how to reduce the pain and prevent the frequency of the cramps.
How hormonal shifts and uterine changes impact cramping
Estrogen and progesterone guide the menstrual cycle. When they fluctuate more unpredictably during perimenopause, the uterine lining may build up more thickly or shed unevenly³. This can make uterine contractions stronger or less regular, which leads to cramps that feel different from earlier years.
A decline in estrogen can also affect how muscles and tissues respond to inflammation and pain signals⁴. These physiological changes explain why cramps can feel sharper or radiate differently during perimenopause.
Other factors that can intensify cramps
Perimenopause affects the whole body, not just hormones.
- Stress and poor sleep can increase pain sensitivity⁵.
- Muscle tension in the abdomen and pelvic floor can worsen discomfort⁶.
- Changes in exercise or nutrition can influence circulation and inflammation⁷.
- Digestive changes, such as constipation or bloating, often occur because the same hormones that affect the uterus also affect the gut⁸.
These factors can make cramping feel more intense, even when the cause is benign. Recognizing these influences helps you respond with care and self-awareness.
When should you be more concerned about cramps?
Cramping is one of the most common physical changes women notice during perimenopause. Some feel mild tightening only around their cycles, while others experience more frequent or longer-lasting cramps that appear between periods⁹. For many, these sensations come and go, lasting from a few hours to several days.
The frequency of cramps depends on how hormone levels fluctuate. During perimenopause, irregular ovulation can cause the uterine lining to thicken unevenly, which may lead to unpredictable contractions and more frequent cramping³. While this is a usual part of hormonal change, it is important to notice patterns that persist or grow more intense over time.
When to consider escalating to a doctor
You know your body best. Some changes are worth discussing with a clinician to rule out underlying causes.
- Cramping that becomes stronger, lasts more than a few days, or interrupts sleep or work.
- Cramps that appear between cycles or continue after periods become infrequent.
- Pain that radiates into the lower back, hips, or thighs, or seems to worsen over time.
- Other symptoms such as heavy bleeding, clotting, pelvic pressure, bloating, or fatigue.
If you experience any of these, contact a healthcare professional. These patterns can sometimes signal conditions such as fibroids, adenomyosis, or endometriosis, which are all treatable¹⁰⁻¹².
Does the intensity of the pain matter?
Yes. The level and quality of pain can offer helpful clues. Mild cramps that ease with rest, stretching, or warmth are usually linked to hormonal activity. However, cramps that are sharp, deep, or stabbing, or that begin suddenly after a period of no discomfort, should be evaluated. Severe or worsening pain should never be ignored.
Can cramps be reduced or prevented?
While perimenopause-related cramps cannot always be prevented, their frequency and severity can often be reduced through consistent self-care and support.
- Stay active: Regular, low-impact movement such as walking or yoga supports circulation and muscle relaxation¹³.
- Prioritize nutrition and hydration: Foods rich in magnesium, calcium, and omega-3 fats support muscle function and hormone balance¹⁴.
- Manage and reduce stress: Relaxation techniques such as mindfulness or gentle stretching lower cortisol and reduce muscle tightness⁵.
- Focus on specific pelvic care: Strengthening and relaxing pelvic muscles improves blood flow and flexibility, which can reduce cramp frequency and intensity (Sword Bloom is the ideal care program to help)⁶.
For some women, cramping appears for a few months and then eases as hormones stabilize. Others experience cycles of discomfort that fluctuate throughout perimenopause⁹. Tracking when cramps occur, how long they last, and what helps can reveal whether the pattern is short-term or might benefit from extra support.
Perimenopausal cramps are common, but they are not something you need to simply accept. Paying attention to changes and seeking guidance early can help you find relief and reassurance.
Bloom gives women expert pelvic care during perimenopause

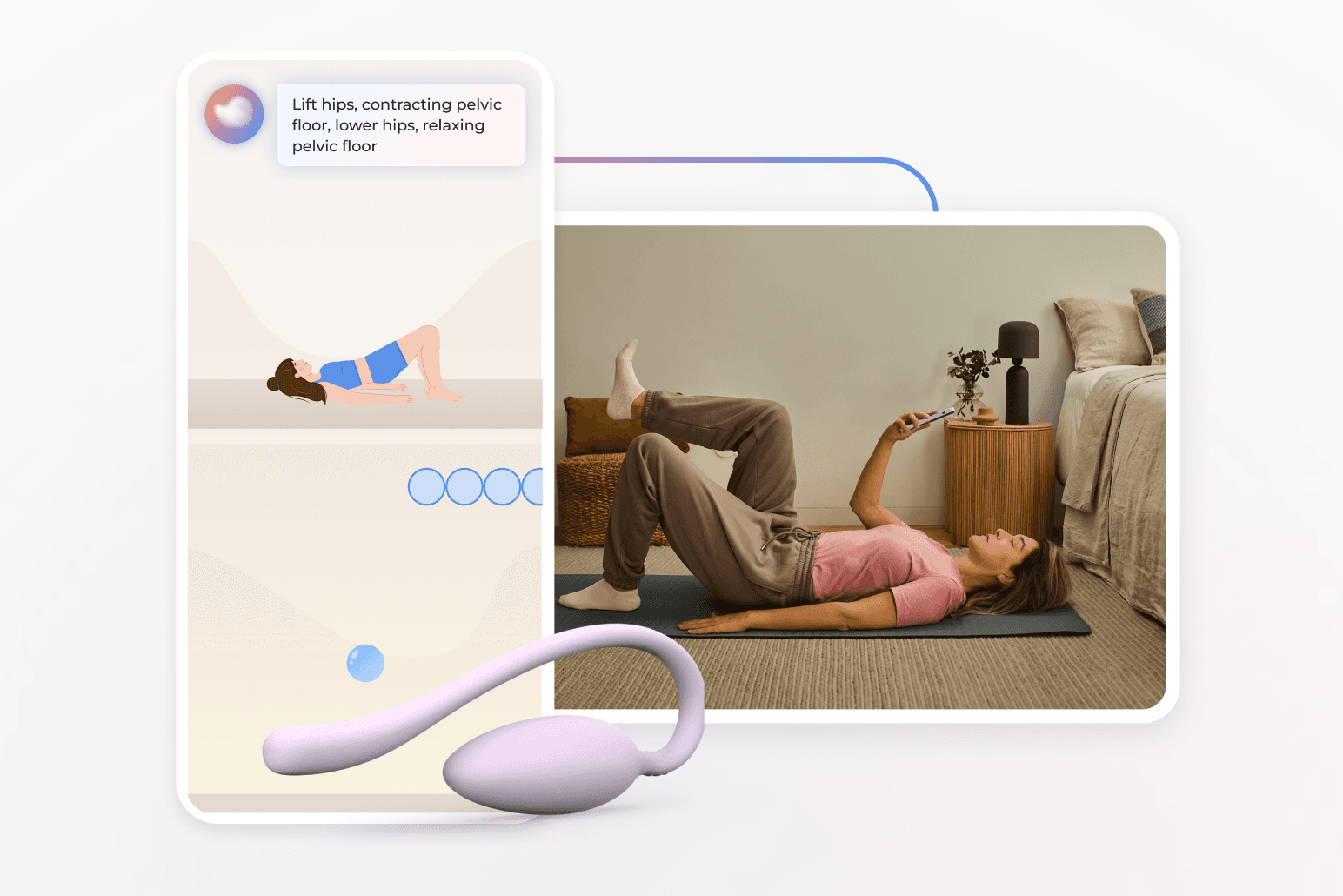
Bloom is a digital women’s health solution designed to support women in every life stage, including perimenopause. Members are paired with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. Each member receives a personalized pelvic care plan through the Sword Health app. The optional Bloom Pod, an FDA-listed biofeedback sensor, which measures muscle movement and provides real-time feedback to help women perform their exercises.
Each session lasts 10 to 15 minutes and fits easily into your day and your personalized program is updated by your care specialist as you progress to keep you adapting and improving. This specialist is also on hand to keep you accountable to your exercise plan, and to escalate your situation to a doctor if your symptoms warrant this action.
Bloom’s results speak for themselves:
- 65% of women report meaningful improvement in daily life¹⁵.
- 56% experience higher productivity and 50% report less anxiety¹⁵.
- 77% complete their program, exceeding typical in-person adherence rates¹⁶.
These outcomes show that consistent, guided pelvic care can reduce discomfort and rebuild body confidence from the privacy of home.
Get started with Sword Bloom in 4 easy steps
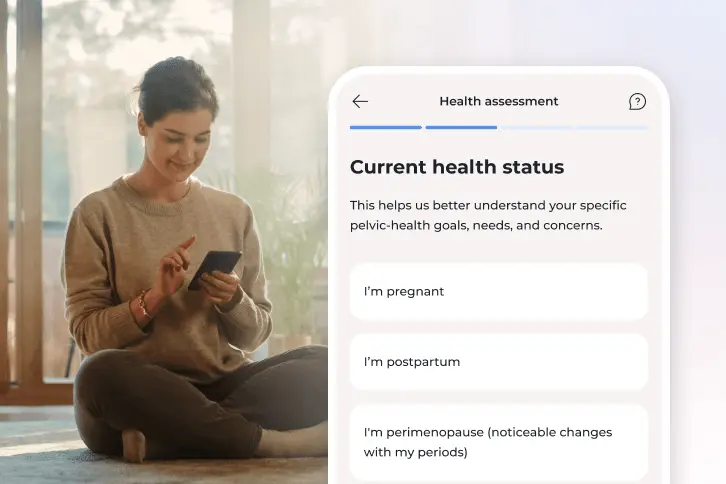
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
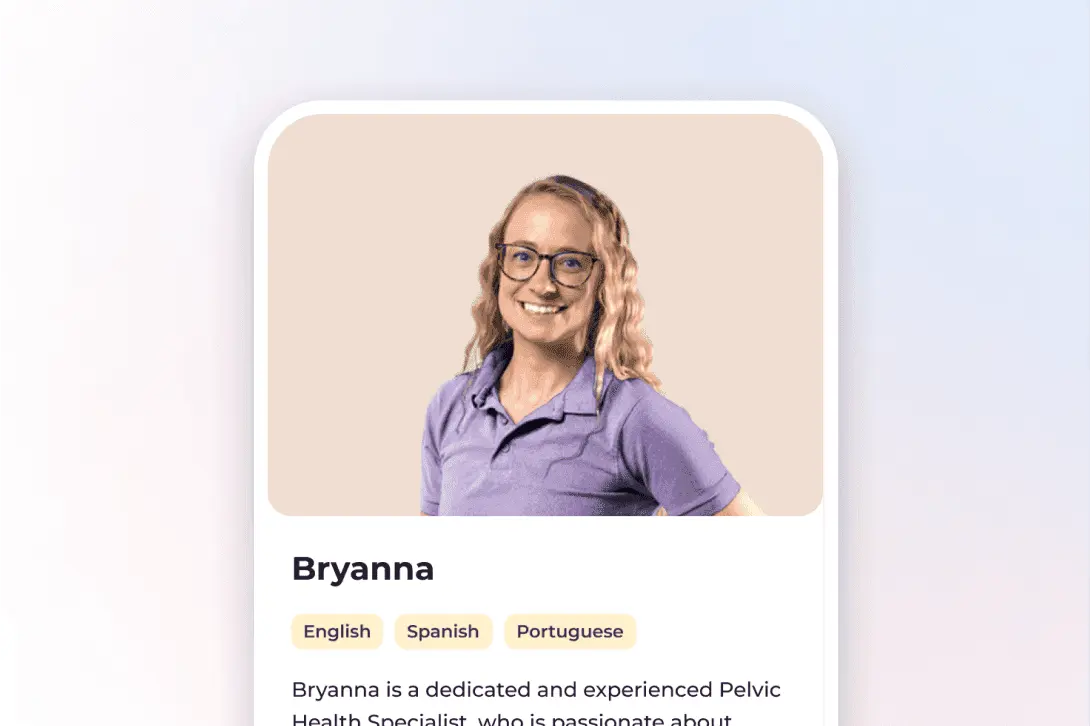
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Why Bloom's easy from-home access is so important
Many women who experience perimenopausal cramps never receive the support they need. In the United States, there is a shortage of pelvic care specialists, and average wait times can exceed 12 weeks¹⁷. Clinic visits may also feel uncomfortable or require time off work.
Bloom removes these barriers. You can access expert guidance privately from home, on your own schedule. About half of Bloom sessions occur after work hours, and one in five take place on weekends¹⁵. Nearly half of Bloom members live in higher-deprivation areas yet achieve the same outcomes as others¹⁵.
Bloom is inclusive, safe, and built for women of all ages, helping more women feel supported and confident through every stage of life.
How to get started with Bloom to better manage your symptoms
Many employers and health plans now include Bloom as a covered benefit¹¹. You may have already coverage within your health insurance to access personalized pelvic and musculoskeletal care at no cost to you.
Checking your eligibility is simple:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Avis NE, et al. JAMA Internal Medicine. 2015;175(4):531–539. https://doi.org/10.1001/jamainternmed.2014.806
Angelou K, et al. Cureus. 2020;12(4):e7586. https://doi.org/10.7759/cureus.7586
Vina J, et al. Aging Research Reviews. 2016;26:1–7. https://doi.org/10.1016/j.arr.2015.12.008
Roman-Blas JA, et al. Arthritis Research & Therapy. 2009;11(5):241. https://doi.org/10.1186/ar2791
Tiidus PM, et al. Exercise and Sport Sciences Reviews. 2011;39(4):151–157. https://doi.org/10.1097/JES.0b013e3182297e92
Tiidus PM, et al. Exercise and Sport Sciences Reviews. 2011;39(4):151–157. https://doi.org/10.1097/JES.0b013e3182297e92
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Warburton DE, et al. CMAJ. 2006;174(6):801–809. https://doi.org/10.1503/cmaj.051351
Calder PC. Nutrients. 2021;13(1):146. https://doi.org/10.3390/nu13010146
Finan PH, et al. The Journal of Pain. 2013;14(12):1539–1552. https://doi.org/10.1016/j.jpain.2013.07.005
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Janela D, et al. Healthcare. 2024;12(2):141. https://www.mdpi.com/2227-9032/12/2/141
American Physical Therapy Association. Workforce Analysis Report: Women’s Health Section. 2023. https://www.apta.org