October 17, 2025 • min read
How better postmenopausal health support helps to retain elite female performers
Written by

Evidence-based healthcare insights
Is postmenopausal health a hidden gap in your health plan?
Most benefits teams are confident in their maternity and fertility support offerings. But have you considered the proportion of female team members in your organization who within the menopause or postmenopause age range? This gap in women's health support coverage sees millions of employees struggling in silence during a stage of life that can define both their personal wellbeing and their professional trajectory.
Nearly 20 percent of the U.S. workforce—about 27 million women—are in menopause or postmenopause¹. This stage is not a brief transition but a third of a woman’s life², often overlapping with her peak career years. Symptoms linked to menopause and pelvic health, such as bladder leakage, fatigue, hot flashes, and sleep disruption, directly affect daily comfort and performance³.
Yet the workplace is rarely designed to accommodate these needs. One in five women has quit or considered quitting her job due to unmanaged symptoms⁴, and global productivity losses tied to menopause are estimated at 150 billion dollars annually⁵. These are not marginal figures; they represent a systemic business issue hiding in plain sight.
For organizations committed to equity and talent retention, addressing postmenopausal health is no longer optional. It is the next frontier in workforce wellbeing and an opportunity to retain the very leaders who hold teams, culture, and institutional knowledge together.
The business case for postmenopausal health support: retain elite female talent for longer
Women in postmenopause are often senior professionals, executives, and experienced domain experts. They manage teams, mentor younger employees, and embody decades of experience. When unmanaged health challenges push these women out of the workforce, companies lose precious decades of experience, strong institutional knowledge, and for female leaders; strategic capability, leadership continuity, and diversity in senior roles.
- Replacing one senior leader can cost up to 200 percent of their annual salary when factoring in recruitment, lost productivity, and training⁶.
- Nearly half of working women in menopause report bladder symptoms, and one in three struggles with moderate to severe difficulty coping at work⁷.
- Add to that the ripple effect of morale loss and institutional knowledge drain, and the cost of inaction becomes even clearer.
Symptoms such as urinary leakage, sleep loss, or chronic discomfort impact the day-to-day working lives of women in postmenopause, and these factors erode confidence. Many take time off or decline advancement opportunities without ever disclosing the real reason.
Ignoring these challenges undermines workforce equity. Investing in postmenopausal support is about about equity, compassion, and performance protection. A benefits leader who enables women to stay comfortable and productive at this stage protects the comapny's leadership pipeline and builds a culture of loyalty and inclusion.
What is the real impact of postmenopause at work?
Postmenopause brings physiological changes that can affect multiple body systems. Declining estrogen weakens the pelvic floor, reduces muscle and bone density, and impacts sleep and mood³. These changes can make even simple tasks, like sitting in long meetings or traveling for work, so much more physically taxing.
Common symptoms of postmenopause include:
- Bladder leakage and urgency
- Bowel dysfunction
- Pelvic organ prolapse
- Vaginal dryness and pain
- Fatigue, night sweats, and brain fog
Nearly half of postmenopausal women live with pelvic-floor dysfunction⁸. Forty-nine percent of working women experience bladder symptoms, and 74 percent of women aged 40–59 experience pelvic organ prolapse⁹.
The physical challenge of the postmenopause life stage for working women clear. The significant emotional burdens are just as impactful, especially for women considering how long they intend to stay in the workforce. Women with pelvic floor dysfunction are 3.6 times more likely to develop depression¹⁰. Shame and silence often keep women from seeking help. Many fear judgment or feel menopause is “not a professional topic.” As a result, they work through exhaustion, mask discomfort, and quietly disengage.
How does a lack of postmenopause support erode employer healthcare costs?
The outcomes of a lack of postmenopause health support is measurable: increased absenteeism, presenteeism, and early exits from the workforce. Many women simply endure symptoms until they require surgical interventions, which can exceed 29,000 dollars per case¹¹. For employers managing self-insured plans, these preventable procedures represent a significant expense.
Pelvic health is a prime example. It is clinically complex but often excluded from traditional benefits plans. Employers who lack targeted pelvic care support leave a major driver of discomfort and healthcare costs untreated. Pelvic floor dysfunction affects up to 50 percent of postmenopausal women⁸ yet remains one of the least discussed and least reimbursed health issues.
What’s needed instead is a structured, clinically grounded approach that meets women where they are: at home, on their schedule, and with expert guidance. Most workplace health programs stop at surface-level wellness. Menopause support, when available, often appears as an awareness campaign or a small stipend for therapy. While well-intentioned, these initiatives fail to address the specific physiological drivers of postmenopausal symptoms.
Adding coverage for postmenopausal health benefits is straightforward
Leading employers are rethinking women’s health benefits through the lens of inclusivity and outcomes. The next generation of benefits strategies includes digital, evidence-based programs that focus on accessibility, scalability, and measurable results. A smart postmenopausal health strategy should:
- Identify coverage gaps: evaluate where menopause and pelvic care are missing from your benefits portfolio.
- Prioritize privacy and flexibility: solutions should integrate seamlessly into women’s daily lives without stigma or disruption.
- Focus on outcomes, not awareness: track improvements in symptom relief, mental health, absenteeism, and ROI.
- Address pelvic care directly: provide clinically validated tools and specialist support to manage bladder control, pain, and confidence.
This approach reflects the future of effective women’s health care. Move away from generic wellness programs and token perks by introducing partners that use a value-based care model. This gives you measurable care pathways that deliver proven health outcomes and supporting commercial impact. In this case, supporting postmenopausal women in the workplace will help employers boos productivity, reduce absenteeism, and retain elite female talent for longer.
Digital health care programs provide more accessible support for working women
For most women who are entering menopause or postmenopause, traditional clinic-based pelvic care can be impractical. Appointments conflict with demanding work schedules and family commitments. Many avoid in-person consultations due to embarrassment or because of a lack of specialized clinicians nearby. Digital-first solutions remove these barriers. Programs like Bloom by Sword Health bring personalized pelvic care into the home, allowing women to access expert-guided care at any time that fits their life.
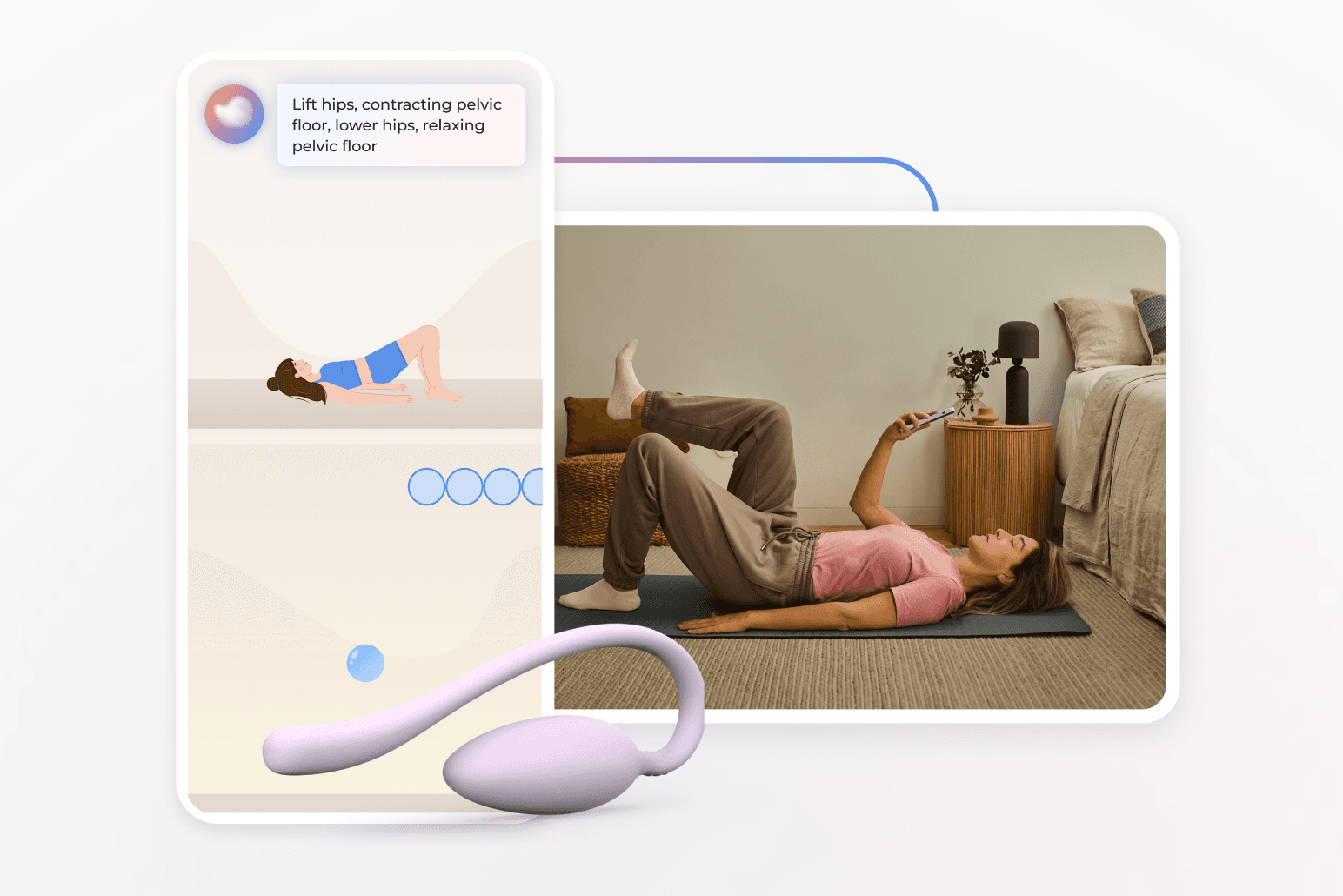
Bloom integrates technology and compassion. The Bloom Pod, an FDA-listed intravaginal biofeedback sensor, connects to the Bloom app, guiding members through short, customized exercises. The program fits flexibly into daily life: 50 percent of sessions occur after hours and 22 percent on weekends¹². Bloom's healthcare impact for working women is consistently powerful and clinically-validated with 65 percent of women reporting improvement from moderate or severe pain to mild or no symptoms¹³.
Bloom's proven health outcomes for women
61%
of women with moderate-to-severe symptoms achieve meaningful improvement.⁹
9/10
The average member satisfaction rating of Bloom members⁹
56%
of Bloom members report a reduction in anxiety
50%
average improvement in productivity after nine sessions using Bloom
These results demonstrate that digital pelvic care can deliver measurable improvements to both physical and mental health while supporting productivity and retention.
Sword's Menopause at Work Whitepaper shows that 90 percent of users are employed full- or part-time¹⁴, many of them in leadership roles. Among them, 25 percent are underrepresented minorities, underscoring Bloom’s reach across diverse populations¹⁴. Nearly half of Bloom members live in moderate-to-high social deprivation areas yet achieve equivalent outcomes¹². For employers, this means equitable impact across demographics and roles. which is a critical factor in advancing workplace inclusion.
Help postmenopausal women bring their best selves to work
Supporting postmenopausal health is both a moral and commercial imperative. Organizations that close this care gap can expect measurable improvements in productivity, retention, and culture. Employers who add Bloom to their benefits are already seeing the return:
- Average annual healthcare savings of 5,203 dollars per member, including 2,276 dollars in pelvic-specific savings¹³.
- ROI of 2.9:1, validated by Risk Strategies Consulting¹³.
- Productivity improvements of nearly 50 percent¹³.
The broader impact extends beyond financial metrics. When women feel supported through menopause, they stay longer, lead stronger, and contribute at their highest capacity. Employers who act now will not only reduce costs but redefine what it means to create a truly equitable workplace.
Stop women suffering in silence with pelvic pain
Offer women life-changing support and slash claim costs driven by pelvic health conditions with Bloom's digital pelvic care plans.
Footnotes
Sword Health. Menopause at Work Whitepaper. 2024. https://swordhealth.com/resources/whitepapers/menopause-at-work
North American Menopause Society. Menopause Practice: A Clinician’s Guide. 2023.
Palmieri S, et al. Int J Gynaecol Obstet. 2022;158(2):346–351.
Biote. Women in the Workplace Survey. 2022. https://biote.com/resources/women-in-the-workplace
Reed, A. Axios. 2022. “Menopause costs the global economy $150 billion a year.” https://www.axios.com/2022/08/10/menopause-work-productivity-cost
Society for Human Resource Management (SHRM). Replacing an employee costs employers 50–200% of annual salary. 2023.
D’Angelo D, et al. Int J Environ Res Public Health. 2022;19(3):1441.
Janela D, et al. JMIR mHealth UHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Kenne K, et al. Sci Rep. 2022;12:9878. https://doi.org/10.1038/s41598-022-13515-4
Molina R, et al. Int J Gynecol Obstet. 2024;164(1):154–162. https://doi.org/10.1002/ijgo.14790
Lamin E, et al. Int Urogynecol J. 2016;27(1):65–72. https://doi.org/10.1007/s00192-015-2773-8
Sword Health. Bloom Health Equity Whitepaper. 2024. https://swordhealth.com/insights/gated-reports/bloom-health-equity
Sword Health. Bloom ROI Whitepaper. 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi
Sword Health. Menopause at Work Whitepaper. 2024. https://swordhealth.com/resources/whitepapers/menopause-at-work