December 9, 2025 • min read
Menopause and incontinence: how to find relief
Menopause can affect bladder control. Learn why leaks happen, how estrogen changes play a role, and the steps that help women feel more comfortable and supported.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Bladder leaks during menopause are common and often linked to estrogen changes that affect pelvic tissues and the pelvic floor.
- These symptoms can feel surprising or confusing, but they are highly manageable with supportive habits and personalized pelvic care.
- Bloom provides expert pelvic support at home and helps women strengthen and coordinate their pelvic floor muscles to reduce leakage and regain confidence.
Why bladder leaks often begin during menopause
Many women are surprised to notice bladder leaks for the first time during menopause. These symptoms can feel unsettling, especially for women who have never experienced leakage before. Menopause brings natural hormonal changes, especially a decrease in estrogen, that affect the bladder, urethra, and the muscles that support them.
Estrogen helps keep pelvic tissues flexible, cushioned, and able to respond to daily movement. As estrogen levels decline, these tissues may become drier or less elastic². The pelvic floor muscles may also weaken or become less coordinated as they adjust to these hormonal shifts. Together, these changes can make it easier for small bladder leaks to occur during lifting, sneezing, laughing, or sudden urges.
These symptoms reflect changes in the body, not a lack of strength or effort. Understanding what is happening can make the experience far less stressful and help you decide what steps to take next.
How estrogen loss affects bladder control
Estrogen supports the tissues that help regulate bladder function. When estrogen levels fall during menopause, the pelvic tissues that support the bladder and urethra lose some of their natural thickness and elasticity. This can make it more challenging to hold urine during movement or when the bladder fills quickly².
Many women notice leaks during coughing or exercise, while others feel sudden urges that are difficult to delay. Some begin waking at night to use the bathroom or feel that their bladder has become more sensitive.
These changes are common and understandable based on how the body adapts during menopause. With the right support, most women are able to reduce these symptoms and feel more comfortable again.
The most common types of incontinence in menopause
Understanding the type of leakage you are experiencing can help you make sense of your symptoms and guide your next steps.
Stress incontinence
Stress incontinence refers to leakage that happens during movement or activities that increase pressure on the abdomen. This may include sneezing, coughing, laughing, lifting, or exercise. During menopause, reduced estrogen and changes in pelvic support can make these leaks more noticeable².
Urge incontinence
Urge incontinence involves a sudden, strong need to urinate, sometimes followed by leakage before reaching the bathroom. This often relates to bladder sensitivity or tension in the pelvic floor muscles.
Mixed incontinence
Mixed incontinence combines both stress and urge leakage. Many women experience a blend of symptoms, and this is a normal part of how menopause can affect bladder function.
Consider your symptoms and these terms as this will help you to communicate more effectively during conversations with a clinician or when exploring supportive pelvic care options.
How to recognize what is causing your bladder leaks
Because the pelvis is a compact space where muscles, organs, and nerves sit close together, bladder-related sensations can feel difficult to pinpoint. You can learn a great deal by observing the patterns that surround your symptoms. It helps to know that patterns offer clues rather than answers. They help build awareness and can be helpful to share with a clinician.
- If your leakage tends to happen during movement or laughing, your pelvic floor may need more support
- If leakage accompanies sudden urges, the bladder may be reacting more quickly than expected
- If symptoms shift based on hydration, stress, or bowel habits, your pelvic system may simply be asking for a bit of adjustment
Why menopause-related bladder leaks feel confusing
Bladder control relies on teamwork between the bladder, urethra, pelvic floor muscles, and surrounding tissues. During menopause, hormonal changes affect each of these structures differently. As they adapt, bladder sensations may change in ways that feel unpredictable.
Many women worry that leaks mean they have done something wrong or failed to maintain strength. This is not true. Bladder leakage during menopause reflects the way your tissues and muscles are responding to hormonal shifts. Once you understand this, it becomes easier to approach your symptoms with clarity and confidence rather than fear or frustration.
Most importantly, these symptoms are highly manageable. With the right support, many women experience meaningful improvement.
How to improve your bladder control during menopause
Every woman’s experience is different, but many find relief through small supportive habits that gently encourage bladder and pelvic muscle balance. These changes often help the bladder feel calmer and reduce the frequency or intensity of leaks.
Before reviewing these options, it may help to know that these are not quick fixes or rigid rules. They are gentle strategies you can experiment with in your daily routine.
- Adjusting hydration earlier in the day can reduce nighttime trips to the bathroom
- Limiting bladder irritants such as caffeine or carbonated drinks may ease urgency
- Supporting bowel regularity can also help, as constipation increases pressure on the bladder²
- Taking movement breaks, softening your abdomen, and avoiding strain during lifting can also lessen tension around the bladder
These small shifts can work together to create a more supportive environment for your pelvic organs. After trying these changes, many women say their bladder feels steadier and more predictable.
Pelvic floor support can reduce menopause-related incontinence
The pelvic floor muscles provide essential support for the bladder and urethra. During menopause, these muscles may weaken, tighten, or lose coordination due to hormonal changes². When the pelvic floor is not working smoothly, leaks and urges can become more common.
This is why pelvic floor support is an important part of menopause-related bladder care. Strengthening can reduce stress leaks, while learning to relax can ease urge-related symptoms. Many women find that once they understand how their pelvic floor behaves, they feel more in control of their day-to-day comfort. Pelvic floor support is most effective when guided, gradual, and personalized, which is where Bloom can help.
Bloom supports women with bladder leaks
Bloom is a digital pelvic care program created by Sword Health. It offers women a private, supportive way to understand their bladder symptoms and strengthen their pelvic floor at home. Bloom combines expert clinical guidance with personalized sessions designed to fit into a busy life.
Every member works one-on-one with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. This specialist learns about your symptoms, routines, and goals, then builds a plan tailored to your needs. Your guided sessions may include gentle strengthening, relaxation strategies, breathing work, posture support, and clear education about bladder health.
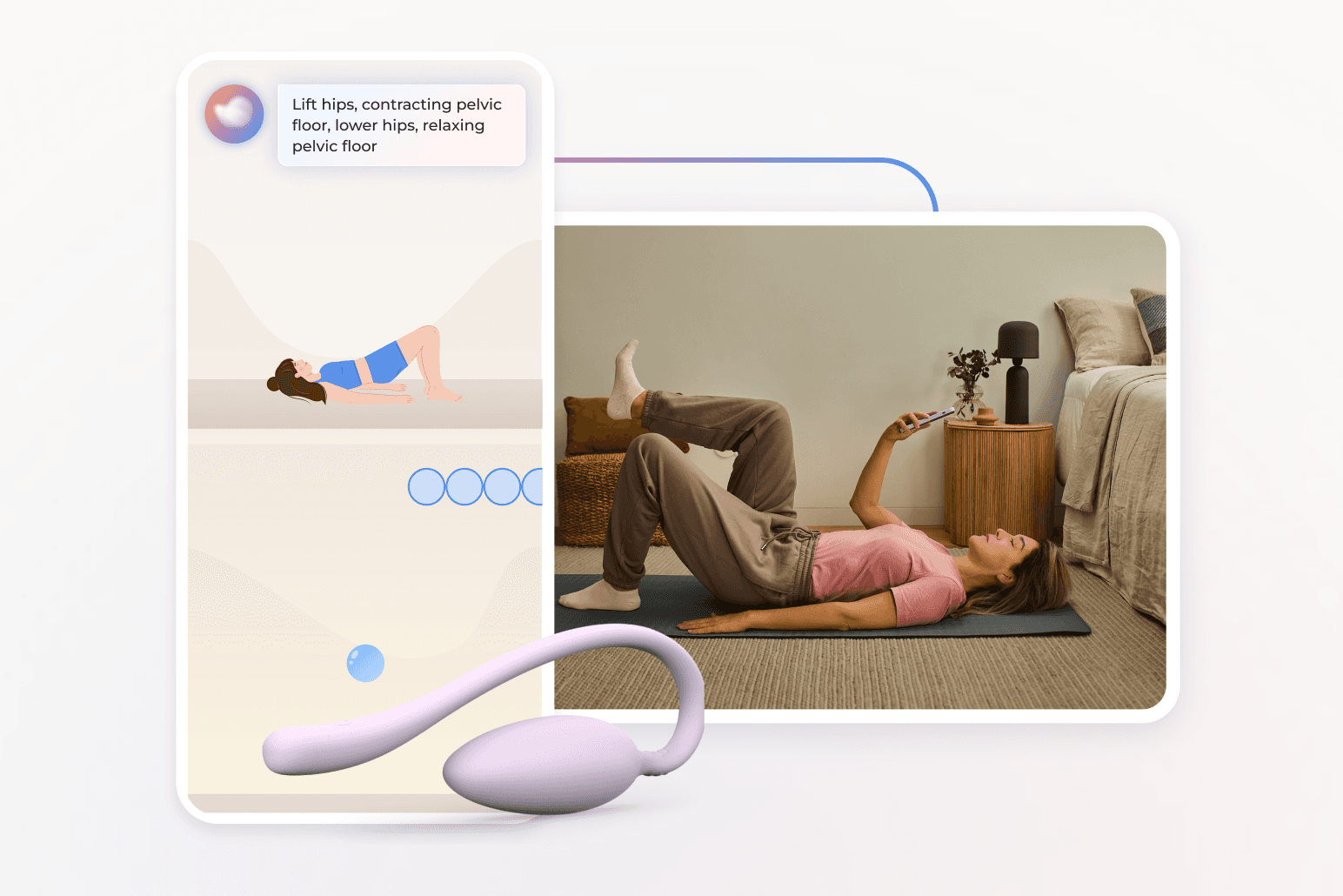
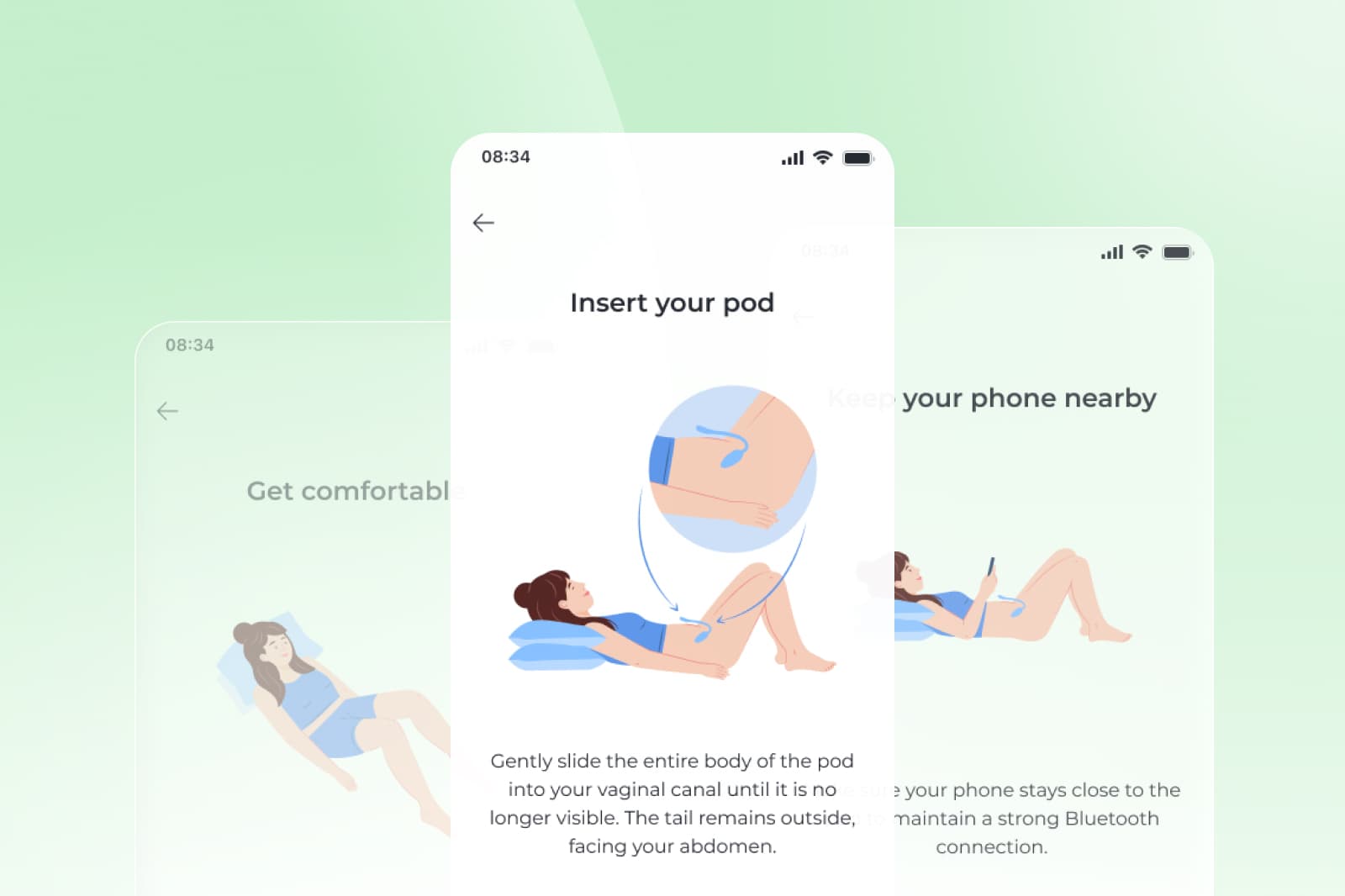
Sessions take about 10 to 15 minutes and can be done at home. For women who are appropriate candidates, Bloom includes an FDA-listed intravaginal sensor called the Bloom Pod, which provides real-time feedback during pelvic floor exercises.
This combination of expert guidance, personalized support, and optional real-time feedback helps many women feel more confident, more aware of their pelvic health, and more in control of their symptoms.
Get started with Sword Bloom in 4 easy steps
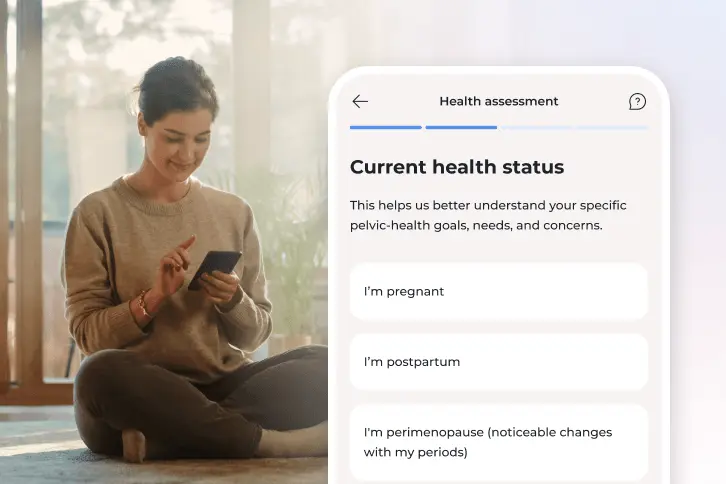
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
What to expect when using Bloom for menopause incontinence
Bloom is designed to feel calm, private, and easy to follow. Many women complete their sessions at times that work best for them such as in the morning or before bed. Through the Sword Health app, your Women’s Health Specialist checks in regularly to help adjust your plan, answer questions, and encourage your progress.
Over time, women often describe feeling more coordinated, less tense, and more confident in managing their bladder habits. Regular practice helps the pelvic floor respond more smoothly during daily movements, which supports improved bladder control.
Bloom member outcomes
Results that show Bloom reduces incontinence
57%
of women with urinary incontinence report symptom relief³
69%
report feeling better or much better overall⁴
When to talk to a clinician about urinary leakage
If you notice symptoms that feel unusual, persistent, or concerning, a clinician can help provide clarity and guidance. This includes symptoms such as:
- blood in your urine
- fever, pain, or burning
- worsening leakage
- sudden or severe symptoms
- signs of urinary tract infection
- pelvic heaviness or pressure
These signs do not necessarily indicate something serious, but they help your clinician decide whether additional care is needed.
How to decide when to seek care and what to do next
Bladder changes during menopause can feel confusing, and it can be difficult to know when symptoms are normal or when a clinician should take a closer look. A helpful starting point is noticing how often leaks occur, what triggers them, and whether they feel different from your usual patterns. These observations can make conversations with a clinician easier and help you understand whether additional support may be useful.
You should reach out to a clinician if you notice symptoms such as blood in your urine, fever, pain, burning, or signs of a urinary tract infection. Persistent or worsening leakage, or bladder symptoms paired with pelvic heaviness or pressure, also deserve clinical evaluation. These clues help a clinician determine whether further testing is needed and what type of care will support your comfort.
Bladder leakage during menopause is common, but it is also highly manageable. You deserve support that is compassionate, clear, and easy to access. Understanding what is happening in your body is the first step toward feeling more in control.
If Bloom is available through your employer or health plan, it can help you understand your symptoms, strengthen your pelvic support system, and feel more confident navigating menopause. Remeber that Bloom does not replace medical evaluation for bladder conditions or incontinence. Instead, it works alongside it. Many women find that understanding how their pelvic muscles work and learning how to calm and coordinate these muscles reduces discomfort and increases confidence in their body’s resilience.
Check your eligibility now to see if you are already covered for Bloom. Many health plans and employer benefits plans offer Bloom at $0 cost to members.
You may already be able to get 24/7 access to your own personalized Bloom care plan with expert guidance from the comfort of home.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Faubion SS, et al. Menopause symptoms and pelvic health changes. Mayo Clinic Proceedings. 2023. https://mcpress.mayoclinic.org/menopause/menopause-unexpected-symptoms-catch-women-by-surprise/
Menopause at Work Whitepaper. Sword Health. Data sourced from Bloom’s 2022 to 2023 book of business. https://swordhealth.com/resources/whitepapers/menopause-at-work
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi
Bloom Book of Business Data 2024. Member overall improvement outcomes. Internal proprietary data.