October 20, 2025 • min read
How to reduce and prevent joint pain in menopause
Discover why menopause affects your joints and how movement, nutrition, and Bloom’s personalized care plans can all help you to stay active and comfortable.
Written by

Evidence-based healthcare insights
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Many women notice new stiffness or joint pain during menopause, often in the hands, knees, shoulders, or throughout the body.
- These sensations are linked to natural hormonal changes that affect collagen, muscle strength, and inflammation.
- The good news: joint pain during menopause is common and manageable. With movement, nourishment, and guided support, you can feel stronger and more comfortable.
Why joint pain becomes more common during menopause
For many women, menopause brings subtle changes that are easy to overlook at first. Your hands might feel tight when you wake up, your knees may click a little when you climb the stairs, or your shoulders may feel sore after activities that once felt effortless. Over time, these sensations can add up, making your body feel heavier or slower to respond.
Joint discomfort during menopause is both common and understandable. Studies suggest that more than half of women in midlife experience some form of joint stiffness or pain². The reason lies in how closely estrogen is tied to your body’s connective tissues.
Estrogen helps maintain collagen, lubricate the joints, and regulate inflammation. As hormone levels decline, cartilage may become less hydrated, and tissues can lose a bit of their natural elasticity. These shifts make the joints more sensitive to everyday strain, especially in areas like the knees, hands, hips, and spine.
But while hormonal changes create the conditions for stiffness, they don’t make joint pain inevitable. Your body remains capable of healing, adapting, and regaining strength. Prevention and management strategies are highly effective when you start early. Make sure you prioritize movement, good nutrition, hydration, and sleep.
This guide will help you understand how to reduce joint pain during menopause and how to prevent it from happening altogether.
Remember, that some low-level pain is okay
Movement is absolutely necessary. Regular exercise is almost always a great idea!
If you slip with your routine or habits from time to time, that’s absolutely fine. Don’t beat yourself up.
But if you maintain consistency with exercise over the long term, you will improve your health and keep your joints feeling good through every stage of menopause.
Discomfort during menopause is not a sign that something is wrong. It is your body asking for care, now you know what steps to take and how you can find expert support. With the right approach, you can regain control of your body to keep yourself moving for the decades to come.
5 ways to prevent joint pain in menopause
This stage of life often brings new sensations, but your body is still capable of strength and adaptability.
The decline in estrogen during menopause affects the entire musculoskeletal system. This hormone influences collagen production, inflammation, and the body’s ability to repair tissue. When estrogen levels fall, joints may lose some of their elasticity, and recovery after exertion can take longer⁹.
These changes are not permanent. They are part of the body’s process of adjusting to a new balance. Your joints can stay mobile for decades to come with steady care, movement, nourishment, and guided support.
First, learn how menopause can impact your joints
Menopause affects every part of your body’s movement system. When estrogen levels drop, your body produces less collagen, the protein that gives structure and elasticity to cartilage, tendons, and ligaments⁴. Estrogen also helps maintain joint lubrication, keeping movements smooth and pain-free.
As this hormone declines, the tissues that surround your joints can lose hydration, and the fluid that cushions your knees, hips, and shoulders becomes less abundant⁵. Over time, this can make your joints feel stiff or creaky, especially after periods of sitting or when you first wake up. Without regular motion, that stiffness can build up, making movement feel more effortful and less natural.
It is important to remember that this change is not permanent or harmful. It is your body’s way of adjusting to a new hormonal rhythm, and movement is key to helping it adapt.
Next, we will explore how to manage joint pain effectively and why each step matters.
1. Keep moving to improve your joint health
Gentle, consistent movement keeps your joints nourished and flexible. When you move, you increase circulation, deliver nutrients to tissues, and help your body produce more synovial fluid, the natural lubricant that protects your joints⁶.
This is not about intense workouts or pushing through pain. It is about showing your body that movement is safe and beneficial.
- Move a little, often. Aim for 30 minutes of light activity most days. Walking, swimming, cycling, or yoga are gentle ways to improve mobility and reduce inflammation⁷.
- Add small bursts of movement into your day. Try standing every hour, rotating your wrists, or rolling your shoulders while waiting for the kettle to boil.
- Stretch after sitting. Hip circles, knee bends, and gentle spinal twists release tension that builds during long periods of stillness.
- Start slow if you have been inactive. Even a five-minute walk after meals can improve circulation and reduce stiffness.
Movement reminds your body that it is adaptable and strong. Each step helps rebuild comfort, stability, and confidence.
2. Strengthen your core and pelvic alignment
Your pelvis forms the foundation for posture and movement. During menopause, hormonal changes can affect the muscles that stabilize your pelvis and core. These muscles may become tighter or weaker, altering your balance and placing more strain on the hips and lower back¹⁷.
This imbalance can make everyday tasks like walking, bending, or sitting feel slightly less stable. Supporting pelvic and core alignment improves posture and reduces joint stress.
How you can strengthen your core and improve alignment
Strengthening your core and pelvic muscles helps your whole body move more efficiently.
- Breathe with awareness. Deep breathing activates your diaphragm and deep core muscles that stabilize your posture.
- Add simple core exercises. Bridges, bird-dog, and side-lying leg lifts build coordination and support.
- Avoid straining. Exhale as you lift, reach, or bend to protect your spine and pelvic floor.
- Check posture throughout the day. Keep your shoulders relaxed and your core lightly engaged.
Programs like Bloom provide guided pelvic care tailored to your needs, helping you strengthen safely and consistently.

Bloom is a digital women’s health solution designed to help women manage perimenopausal symptoms like joint stiffness, back discomfort, and pelvic tension.
Each member is paired with a Women’s Health Specialist (Doctor of Physical Therapy) who creates a personalized care plan focused on strength, posture, and mobility. Members access short, guided sessions through the Sword Health app and use the Bloom Pod which is a safe, FDA-listed biofeedback device that provides real-time feedback during exercises.

3. Manage inflammation after exercise
Hormonal changes influence how your body manages inflammation. Estrogen helps regulate immune activity and antioxidant balance. When levels drop, inflammation can rise more easily, especially in the joints and connective tissues¹¹.
This means your body may feel more sensitive after exercise or during stressful weeks. You might notice stiffness that lingers longer than before, or a general feeling of heaviness in your limbs. Lifestyle factors such as sleep and nutrition can amplify or reduce these sensations.
This inflammation is not harmful in itself. It is your body’s way of adjusting to new hormonal patterns. With the right support, your system can rebalance.
How you can calm inflammation and support recovery
Your diet and hydration influence how your joints feel and heal. Choosing anti-inflammatory foods and prioritizing hydration can help reduce soreness and support repair.
- Include omega-3s often. Foods like salmon, flaxseed, and walnuts reduce inflammation and protect joint tissue¹².
- Eat colorful foods. Berries, spinach, and peppers supply antioxidants that fight oxidative stress.
- Stay hydrated. Water supports joint lubrication and helps remove metabolic waste¹³.
- Limit highly processed foods and excess sugar, which can increase inflammation.
If meeting nutritional needs through food alone is difficult, discuss supplements such as vitamin D, magnesium, or omega-3s with your clinician.
4. Restore muscles by prioritizing flexibility and rest
Many women notice their muscles feeling tighter or less responsive during menopause. Estrogen affects not only the joints but also muscle tone throughout the body. When hormone levels drop, muscles can lose elasticity, especially around the hips, shoulders, and back¹⁴.
Sleep can also become disrupted, slowing recovery. When you do not sleep well, your body produces more cortisol, a stress hormone that increases inflammation and pain sensitivity¹⁵. Over time, this can create a cycle of stiffness and fatigue.
You can interrupt this cycle with a few restorative habits that improve both rest and flexibility.
How you can improve flexibility and get better rest
A combination of gentle stretching and good sleep hygiene helps your body relax, repair, and restore strength.
- Stretch before bed. Spend a few minutes loosening your hips, shoulders, and back while breathing deeply.
- Create a calming routine. Reduce screen time and lower lights before bed to signal your body it is time to rest.
- Practice mindful breathing during movement. Inhale through your nose and exhale through your mouth to release tension.
- Keep consistent sleep times. Going to bed and waking up at the same time each day supports hormonal balance and tissue recovery¹⁶.
Better rest supports better movement. You will likely notice less morning stiffness and improved energy.

5. Prevent pain by building muscle strength
During menopause, changes in estrogen levels affect more than flexibility. Estrogen helps maintain lean muscle mass and bone density. As levels decline, your body naturally loses some of that strength and stability, which can increase the workload on your joints⁸.
When muscles around the joints weaken, those joints bear more pressure. Over time, this can lead to fatigue, stiffness, and slower recovery after activity.
This loss of strength is not permanent. Muscles respond quickly to consistent, gentle training. Building strength protects your joints and restores energy to daily movement.
How you can rebuild muscle strength and protect your joints
Strength training is one of the most effective ways to restore support around your joints. You do not need heavy weights or a gym. A few short sessions each week can make a noticeable difference in how your body feels⁹.
- Start with simple, low-impact exercises. Try wall sits, bridges, or supported squats to build hip and leg strength without stressing joints.
- Focus on form, not intensity. Move slowly and breathe evenly, exhaling through effort.
- Balance strength with flexibility. Combine resistance work with stretching or yoga to maintain fluid movement.
- Stay consistent. Two or three short sessions each week can rebuild muscle and reduce strain on joints¹⁰.
Sword Move gives you the expert guidance to overcome pain and build the whole-body strength you need to prevent injury.
Get started with Sword Move for whole-body strength
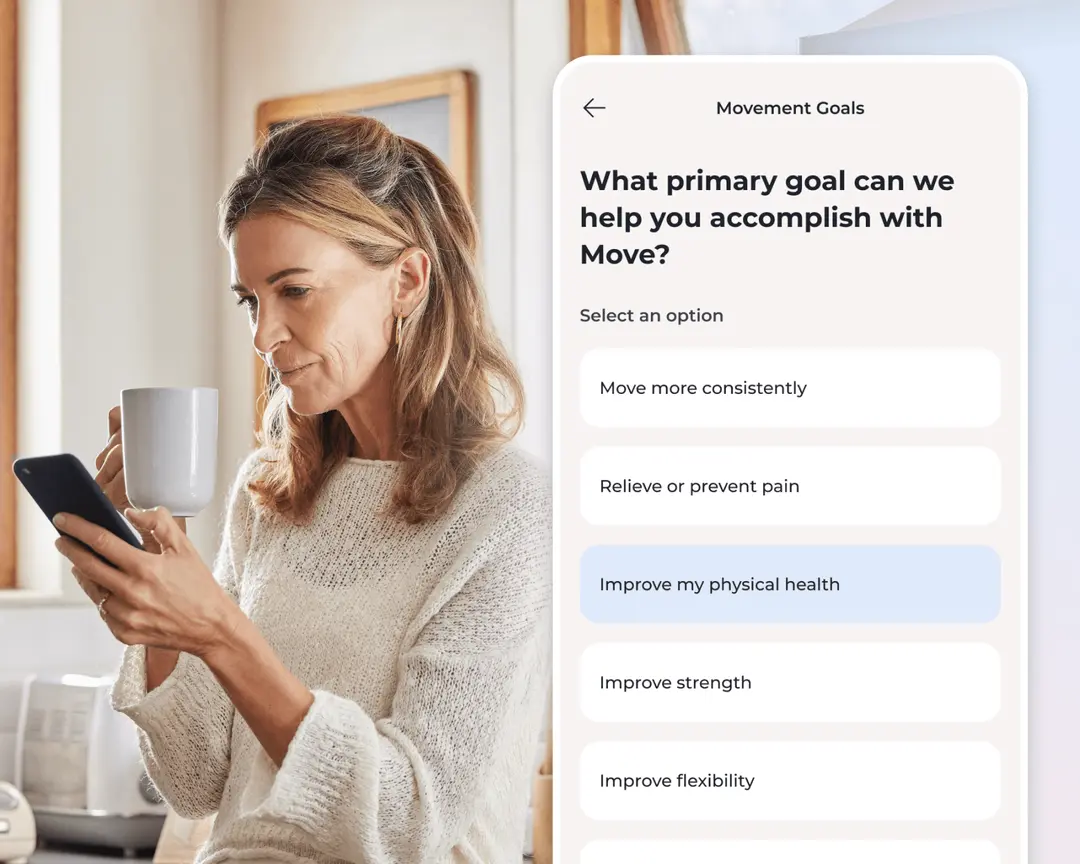
1. Tell us about you
We’ll learn about your goals, job type, lifestyle, and movement history.

2. Match with a Physical Health Specialist
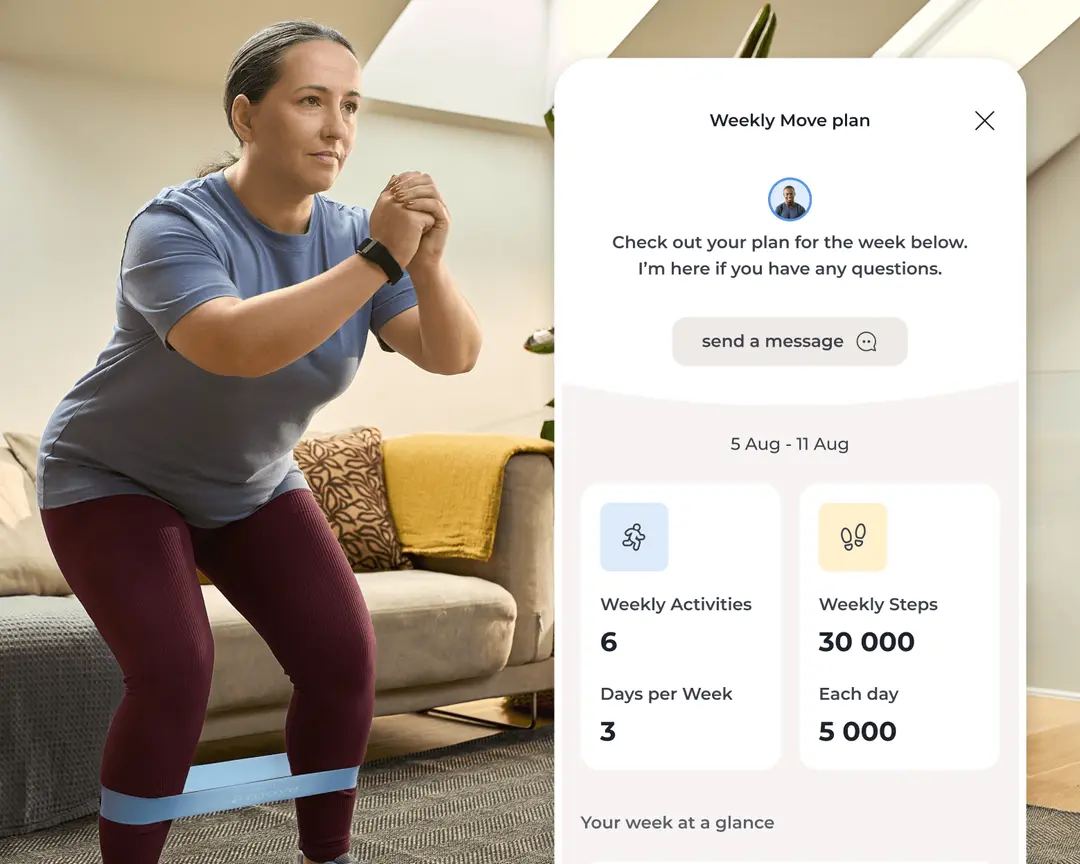
Your dedicated Sword Move specialist will create a personalized plan just for you.

3. Receive your Move kit
You’ll get a free Move wearable and resistance bands delivered to your door.
4. Start moving with your personalized plan
Pair your Move wearable and begin weekly goals built around your activity level, routines, and progress.
You’ll be matched with a Physical Health Specialist who gets to know your goals, lifestyle, and movement history. Based on that, you’ll follow a plan tailored to your specific health goals with short, guided sessions (10 minutes or less) and daily step targets, all delivered through the Sword mobile app.
Take the next step toward moving with confidence
Physical activity is a great protector for women during any life stage, but regular movement is particularly helpful for women managing joint pain in menopause.
Sword Move makes it easy to protect your strength, prevent joint pain, and reduce the impact of any body aches or muscle stiffness.
Move was created for exactly this purpose, to help you build healthier routines with simple, personalized guidance you can follow from home. With the guidance of 24/7 expert support and the Move Wearable keeping you on track, every step brings you closer to feeling stronger and more resilient.
By joining Move, you are making a commitment to better health, greater energy, and a future with fewer limits.
Check your coverage today to see if Move is available to you and take the first step toward lasting progress.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Avis NE, et al. JAMA Internal Medicine. 2015;175(4):531–539. https://doi.org/10.1001/jamainternmed.2014.806
Roman-Blas JA, et al. Arthritis Research & Therapy. 2009;11(5):241. https://doi.org/10.1186/ar2791
Vina J, et al. Aging Research Reviews. 2016;26:1–7. https://doi.org/10.1016/j.arr.2015.12.008
Finan PH, et al. The Journal of Pain. 2013;14(12):1539–1552. https://doi.org/10.1016/j.jpain.2013.07.005
Calder PC. Nutrients. 2021;13(1):146. https://doi.org/10.3390/nu13010146
Kenefick RW. Sports Medicine. 2018;48(S1):31–37. https://doi.org/10.1007/s40279-017-0845-3
Irwin MR. Physiological Reviews. 2015;95(2):553–605. https://doi.org/10.1152/physrev.00032.2014
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Angelou K, et al. Cureus. 2020;12(4):e7586. https://doi.org/10.7759/cureus.7586
Warburton DE, et al. CMAJ. 2006;174(6):801–809. https://doi.org/10.1503/cmaj.051351
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Janela D, et al. Healthcare. 2024;12(2):141. https://www.mdpi.com/2227-9032/12/2/141