October 20, 2025 • min read
Stomach problems in menopause: Gentle ways to ease pain
Learn how menopause can cause stomach problems and discover gentle, effective ways to ease pain and support your core with Bloom’s expert pelvic care.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Many women experience new stomach or abdominal discomfort in menopause without clear guidance on why it happens.
- Hormonal changes affect digestion, gut sensitivity, and the pelvic floor, creating bloating, cramping, or pressure that can feel confusing or alarming.
- By understanding these changes and implementing a few preventative pelvic health safeguards, you can manage symptoms with confidence and comfort.
Why stomach and abdominal pain can increase during menopause
If you have noticed stomach aches, bloating, or general discomfort that you did not experience before, you are not alone. Many women experience these changes in midlife. Studies show that gastrointestinal symptoms, including bloating and abdominal pain, increase significantly during perimenopause and menopause¹.
This discomfort can feel like fullness after meals, dull aching near the lower belly, or cramping that comes and goes. These sensations are common, but that does not make them easy to live with.
The changes in hormones that drive menopause also affect nearly every part of your body, including your digestive system. Estrogen helps regulate muscle tone in the intestines, influences gut bacteria, and supports the nerves that control digestion. As estrogen levels fluctuate and decline, these systems become more sensitive, leading to bloating, slower digestion, or pain after eating².
The connection between hormones, digestion, and the pelvic floor
Your digestive system and your pelvic floor work closely together. When one is affected, the other often reacts.
Estrogen helps keep tissues in your abdomen and pelvis strong, hydrated, and flexible. As hormone levels fall, muscles and connective tissues lose some of that elasticity, and circulation slows. This can cause the muscles of the pelvic floor (the group of muscles that support your bladder, bowel, and uterus) to become tense or weak. When that happens, it can create pressure and pain that feels like it is coming from the stomach or abdomen³.
Bloating or constipation can make this worse by putting extra pressure on the pelvic muscles. Over time, this cycle can lead to persistent discomfort or feelings of heaviness in the abdomen.
Learning how to relax and strengthen the pelvic floor can improve circulation, digestion, and muscle coordination, helping you relieve this pressure and reduce pain.
How to tell if your pain is digestive, pelvic, or both
Abdominal discomfort in menopause can have several causes. Some are related to digestion, some to the pelvic floor, and often both systems overlap.
If your pain feels like… | It may be related to… |
Cramping, bloating, or pain after meals | Digestive changes from hormones or diet |
Pressure or aching in the lower abdomen | Pelvic floor muscle tension or weakness |
Discomfort that worsens with stress or activity | Pelvic muscle overactivity or tightness |
Constipation and abdominal fullness | Slow intestinal movement and pelvic strain |
You do not need to know which system is the main cause to start improving how you feel. Gentle movement, hydration, and targeted pelvic care can help restore balance across both areas.
Practical ways to reduce abdominal pain in menopause
Many women describe menopause-related stomach pain as one of the most confusing symptoms of this stage of life. It can feel unpredictable, with days of dull pressure followed by sharper aches that make you wonder if something more serious is happening. This uncertainty can be unsettling, especially when medical tests come back “normal.”
These sensations are often your body adjusting to hormonal shifts that affect digestion and circulation. Estrogen helps muscles contract efficiently in the gut, so when levels drop, digestion can slow, allowing more gas and pressure to build. The good news is that this discomfort can usually be eased with small, consistent changes that help your body adapt. The biggest learning is that movement is critical! Any form works. Walking, cycling, even just playing with your children or grandkids is great medicine.

Here are a few strategies that help most women feel better over time:
- Move regularly, even gently: Movement encourages circulation and digestion, helping your body process meals and relieve tension. Walking after eating or taking stretch breaks during the day can ease that feeling of fullness or tightness. Studies show that light physical activity after meals improves digestion and reduces bloating⁴.
- Hydrate and nourish consistently: Water supports every digestive process. Aim to sip water throughout the day to prevent dehydration, which can slow digestion and increase bloating. Eating a fiber-rich diet with foods such as oats, leafy greens, and legumes also helps maintain regularity and reduce abdominal pressure⁵.
- Pause and breathe deeply: Many women hold tension in their abdominal and pelvic muscles when stressed. Deep, diaphragmatic breathing relaxes these muscles, supports oxygen flow, and helps calm the nervous system. Research shows that this kind of mindful breathing can reduce both perceived and physical symptoms of pain⁶.
- Notice patterns without judgment: Tracking when discomfort appears (whether it is after meals, during stressful periods, or following long days of sitting) can help you identify triggers. Awareness helps you make gentle adjustments that work for your body rather than forcing changes that feel restrictive or stressful.
These steps may seem simple, but together they retrain your body to respond with ease instead of tension. Healing is not about doing everything perfectly; it is about progress, consistency, and compassion for yourself.
How to prevent future discomfort with simple pelvic care
One of the most overlooked contributors to abdominal discomfort in menopause is muscle imbalance. Your abdominal and pelvic floor muscles act as partners, supporting your organs and stabilizing your spine. When estrogen drops, these muscles can lose coordination — some become tight while others weaken. This imbalance can cause pressure, bloating, or even mild cramping sensations⁷.
The encouraging news is that your body is capable of remarkable adaptation. When you begin restoring balance through gentle, guided movement, your body responds quickly.
With Bloom, you are not left guessing what to do. Each member is paired with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. Together, you learn how to:
- Reconnect with your deep core and pelvic floor through safe, guided movements.
- Release tension where your muscles have become tight.
- Rebuild strength where your body needs more support.
- Move comfortably again while regaining confidence in your body.
All sessions are private and completed at home using the Bloom app. Many members say this privacy helps them relax and stay consistent. Whether you complete a session in the morning or before bed, it fits naturally into your day.
By improving coordination between your abdominal and pelvic muscles, you support digestion, posture, and daily comfort. With time, these small steps can make a major difference in how you feel each day.
When should you escalate stomach pain to see a doctor?
Even though most menopause-related abdominal discomfort is harmless and manageable, it can still be worrying, especially when pain lingers or changes unexpectedly. It is normal to feel unsure about what deserves a doctor’s attention. Understanding when to reach out helps you feel more confident and supported.
Start by listening closely to your body. If something feels new and very different, or persistent, it is always worth mentioning to your clinician. Seeking guidance early is not overreacting; it is caring for yourself with intention.
You should schedule a check-in or appointment if you notice:
- Sudden or severe abdominal pain that appears quickly or wakes you from sleep.
- Pain with fever, nausea, or vomiting, which can signal an infection or inflammation that needs prompt evaluation.
- Unexplained weight loss or appetite changes that last more than a couple of weeks.
- Blood in your stool or dark, tarry bowel movements.
- Pain that continues to worsen or disrupts sleep and daily activities.
Most of the time, these symptoms have simple explanations and can be treated easily once identified. Your clinician can perform a physical exam, discuss your hormonal history, and rule out conditions such as gallbladder issues, fibroids, or digestive sensitivities that sometimes surface during menopause.
Remember that getting checked does not mean something is wrong. It means you are taking ownership of your health and getting the reassurance you deserve. Early evaluation often brings quick peace of mind and, if needed, a clear plan to help you feel better.
If your pain is mild but persistent, programs like Bloom can complement medical care by helping you rebuild strength, relieve tension, and improve comfort from home. Also, Bloom has in-built mechanisms to refer you to a doctor if you need more acute care. All members are matched with a women’s health specialist who also carries a Doctorate in Physical Therapy. This specialist will be able to escalate your care when needed.
Bloom gives women expert pelvic care during menopause
Bloom is a digital women’s health solution designed to support women in every life stage, and it provides particularly strong support for women experiencing stomach, bowel, and bladder issues. Members are paired with a Women’s Health Specialist who holds a Doctor of Physical Therapy degree. Each member receives a personalized pelvic care plan through the Sword Health app. The optional Bloom Pod, an FDA-listed biofeedback sensor, which measures muscle movement and provides real-time feedback to help women perform their exercises.
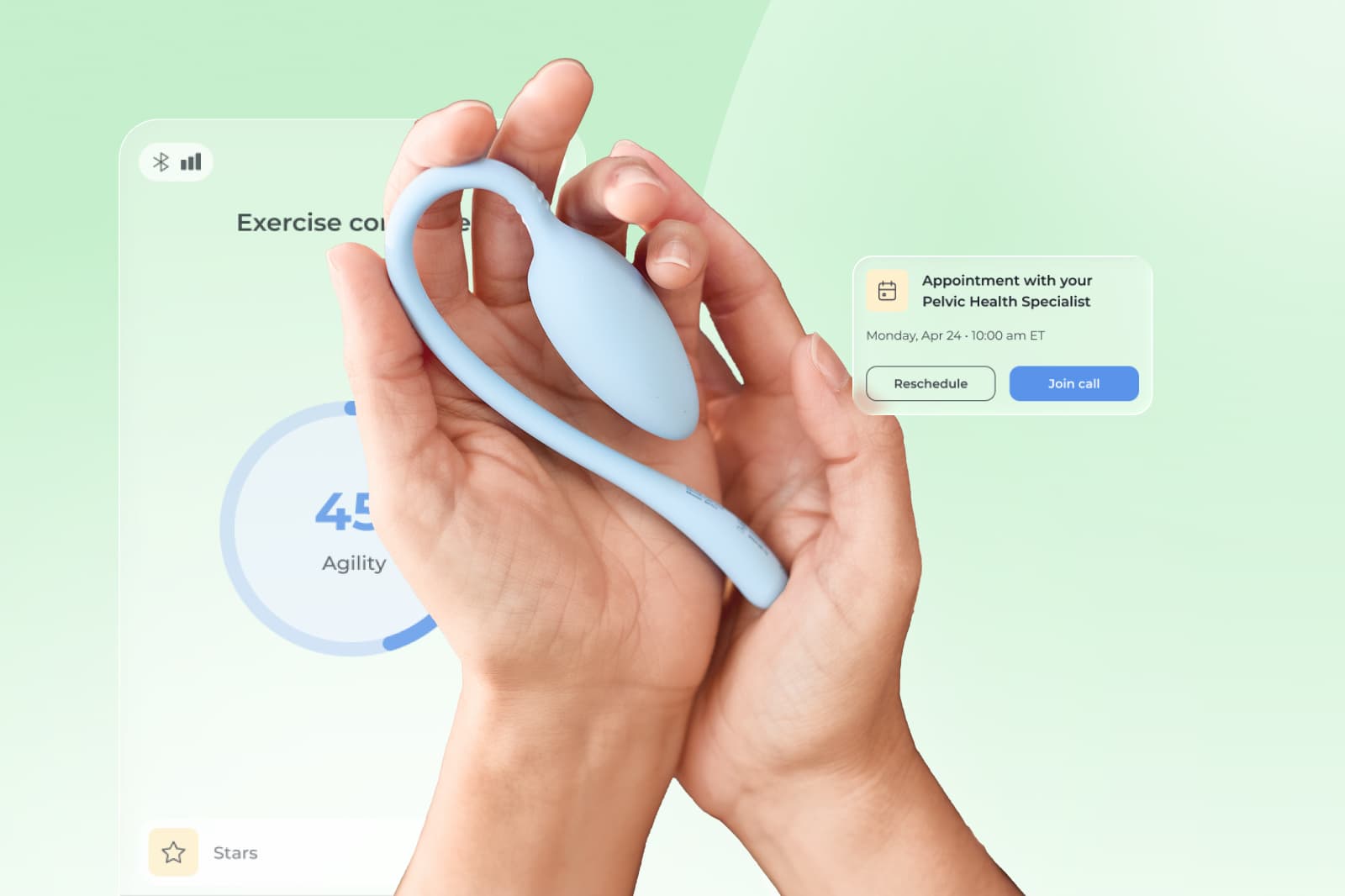
Each session lasts 10 to 15 minutes and fits easily into your day and your personalized program is updated by your care specialist as you progress to keep you adapting and improving. This specialist is also on hand to keep you accountable to your exercise plan, and to escalate your situation to a doctor if your symptoms warrant this action.
Bloom’s results speak for themselves:
- 65% of women report meaningful improvement in daily life¹⁵.
- 56% experience higher productivity and 50% report less anxiety¹⁵.
- 77% complete their program, exceeding typical in-person adherence rates¹⁶.
These outcomes show that consistent, guided pelvic care can reduce the impact of your symptoms and help you to manage and prevent stomach discomfort – all from the privacy of your home.
Get started with Sword Bloom in 4 easy steps
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
See if Bloom is already covered by your health plan
Menopause may bring new sensations, but discomfort does not have to define this stage of life. Your body is not failing; it is adapting. With the right understanding and support, you can move through this phase feeling informed, capable, and hopeful.
Bloom helps you take control of your pelvic and core health from home. Through personalized guidance, private sessions, and expert feedback, Bloom helps women reduce abdominal and pelvic discomfort while building strength, confidence, and trust in their bodies.
You do not have to wait or wonder if what you are feeling is “normal.” You can start improving your comfort and confidence today. Check to see if your health plan has coverage for Bloom and you might be able to get started at $0 cost to you.
Checking your eligibility is simple:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Heitkemper M, et al. Menopause and gastrointestinal symptoms: A population-based study. Menopause. 2021;28(3):234–242. https://doi.org/10.1097/GME.0000000000001700
Jackson S, et al. Hormonal influences on gastrointestinal motility. Gastroenterology Clinics of North America. 2019;48(4):765–777. https://doi.org/10.1016/j.gtc.2019.08.004
Nygaard I, et al. Pelvic floor function and its impact on abdominal and digestive symptoms. International Urogynecology Journal. 2020;31(5):913–921. https://doi.org/10.1007/s00192-019-04083-5
Matsuo K, et al. Postprandial walking improves gastrointestinal motility. World Journal of Gastroenterology. 2022;28(12):1281–1290. https://doi.org/10.3748/wjg.v28.i12.1281
Zhang Y, et al. Dietary fiber and gastrointestinal health. Nutrients. 2021;13(12):4383. https://doi.org/10.3390/nu13124383
Mehling WE, et al. Diaphragmatic breathing and pain reduction in chronic conditions. Pain Medicine. 2020;21(6):1111–1120. https://doi.org/10.1093/pm/pnz325
Khandelwal C, et al. Hormonal changes and pelvic floor dysfunction: A review. Obstetrics and Gynecology Clinics of North America. 2020;47(4):529–540. https://doi.org/10.1016/j.ogc.2020.08.003