October 10, 2025 • min read
The rise of virtual pelvic floor therapy adoption
Virtual pelvic therapy is growing fast. Learn what is driving adoption, and how Bloom delivers effective, personalized at-home care plans.
Written by

Senior Clinical Program Manager, Sword Bloom ·
From suffering in silence to momentum in women’s health at work
For decades, pelvic floor therapy was one of healthcare’s most underutilized interventions. Millions of women endured conditions like incontinence, prolapse, and chronic pelvic pain without treatment, often because stigma, access barriers, or lack of employer coverage stood in the way. Many were told their symptoms were “normal” after childbirth or aging. Others quietly withdrew from activities at work and home rather than seek help.
That era of silence is ending. A powerful convergence of factors including technology innovation, rising demand from employees, and employer cost pressures, is fueling the rapid adoption of virtual pelvic floor therapy. What was once seen as a niche clinical service is now emerging as a cornerstone of leading women’s health care strategies.
Pelvic floor disorders are affecting 1 in 3 women of working age
Pelvic floor disorders (PFDs) affect nearly one in three U.S. women during their lifetime,¹ with prevalence climbing to nearly one in two among postmenopausal women.² Symptoms range from urinary leakage and bowel dysfunction to painful intercourse and chronic pelvic pain.
The consequences reach far beyond discomfort. Women with PFDs are more than three times as likely to experience depression or anxiety,³ while chronic pelvic pain can reduce workplace performance by more than 60%.⁴ Surgeries for advanced conditions often exceed $29,000 per case,⁵ creating significant cost exposure for employers and health plans.
Despite this impact, women delay seeking care for an average of 6.5 years.⁶ Conditions worsen, interventions become more invasive, and workplace productivity suffers. The scale of unmet need makes pelvic health an urgent priority for benefits leaders.
Why traditional pelvic therapy models fall short
Pelvic floor therapy delivered in-clinic by trained specialists is clinically proven to reduce symptoms and prevent costly interventions. Yet access is highly limited. In the U.S., there is roughly one pelvic health therapist for every 10,000 women.⁷ Clinics are clustered in urban centers, with appointments typically offered only during working hours.
These barriers create steep drop-off rates. Fewer than one in ten women who need therapy ever complete a full in-clinic program.⁷ The burden of commuting, scheduling, and stigma means even proven therapies fail to reach the people who need them most.
This mismatch between strong clinical evidence and the access difficulties facing working women has given more momentum to digital women's health care programs.
How technology is transforming access with virtual pelvic care
The past decade has brought remarkable innovation in telehealth pelvic therapy and dedicated digital women's healthcare programs. Advances in motion sensor cameras, mobile apps, and video technology have moved therapy from clinic rooms into living rooms. The virtual delivery model overcomes so many of the access barriers that prevent women from engaging with traditional pelvic floor physical therapy.
Virtual pelvic floor therapy programs typically combine one or some of the following:
- Biofeedback devices that track pelvic floor muscle contractions and provide real-time guidance, like Sword's revolutionary Bloom Pod.
- Digital platforms that guide daily exercises, track progress, and provide secure messaging with providers.
- Telehealth consultations with licensed pelvic health specialists for coaching and education.
These advances make therapy discreet, convenient, and scalable. Instead of weekly clinic visits, members can complete 10-minute sessions from home, after hours, or on weekends. Data is shared instantly with their therapist, enabling personalized adjustments and better continuity of care.
Women are driving demand for virtual pelvic floor therapy
Cultural attitudes are shifting. Conditions like incontinence and pelvic pain were once taboo topics, but today women are more willing to speak up and demand support. Social platforms, advocacy movements, and workplace equity initiatives have accelerated this change.
Employees want benefits that reflect their lived experiences, including support beyond maternity. Menopause, pelvic health, and other issues once overlooked are now seen as essential. Employers that fail to provide solutions risk losing credibility with half their workforce.
Demand is also about performance. Women want to thrive at work without symptoms undermining confidence or focus. Addressing pelvic health directly contributes to productivity and retention.
The business case for dedicated women's health programs
Benefits leaders understand the importance of dedicated women's health programs that help their female employees bring their best self to work, helping to increase productivity, reduce absenteeism, and retain elite female performers for longer.
Virtual pelvic floor therapy addresses both the health needs of employees and the financial pressures of employers.
- Claims savings: Early therapy prevents unnecessary imaging, medications, and surgeries, reducing spend.
- Productivity gains: Employees relieved of pain and urgency regain focus at work.
- Retention: Senior women, often in leadership roles, are more likely to stay when symptoms are managed.
- Equity: Virtual-first care removes geographic and time barriers, reaching women in rural or underserved communities.
When benefits teams weigh costs against returns, the case for digital pelvic health solutions like Sword's Bloom program becomes clear.
Sword Bloom's virtual pelvic health has an industry-leading 2.9x ROI
Bloom by Sword Health is a dedicated women's health program built to deliver expert personalised care plans at scale while preserving clinical quality. For employers and health insurers, Bloom is an ideal addition to any health plan, providing dedicated coverage for women with pelvic pain, urinary incontinence, bowel and bladder disorders. The revolutionary digital delivery model allows women to access care from the comfort of home, designed to help women through all phases of life; from pregnancy and postpartum care, through to menopause and postmenopause.
At the core is the Bloom Pod, an FDA-listed intravaginal sensor that tracks muscle activity and provides real-time biofeedback through the Bloom app. Licensed Pelvic Health Specialists, each holding a Doctor of Physical Therapy degree, monitor data and guide members with personalized plans.
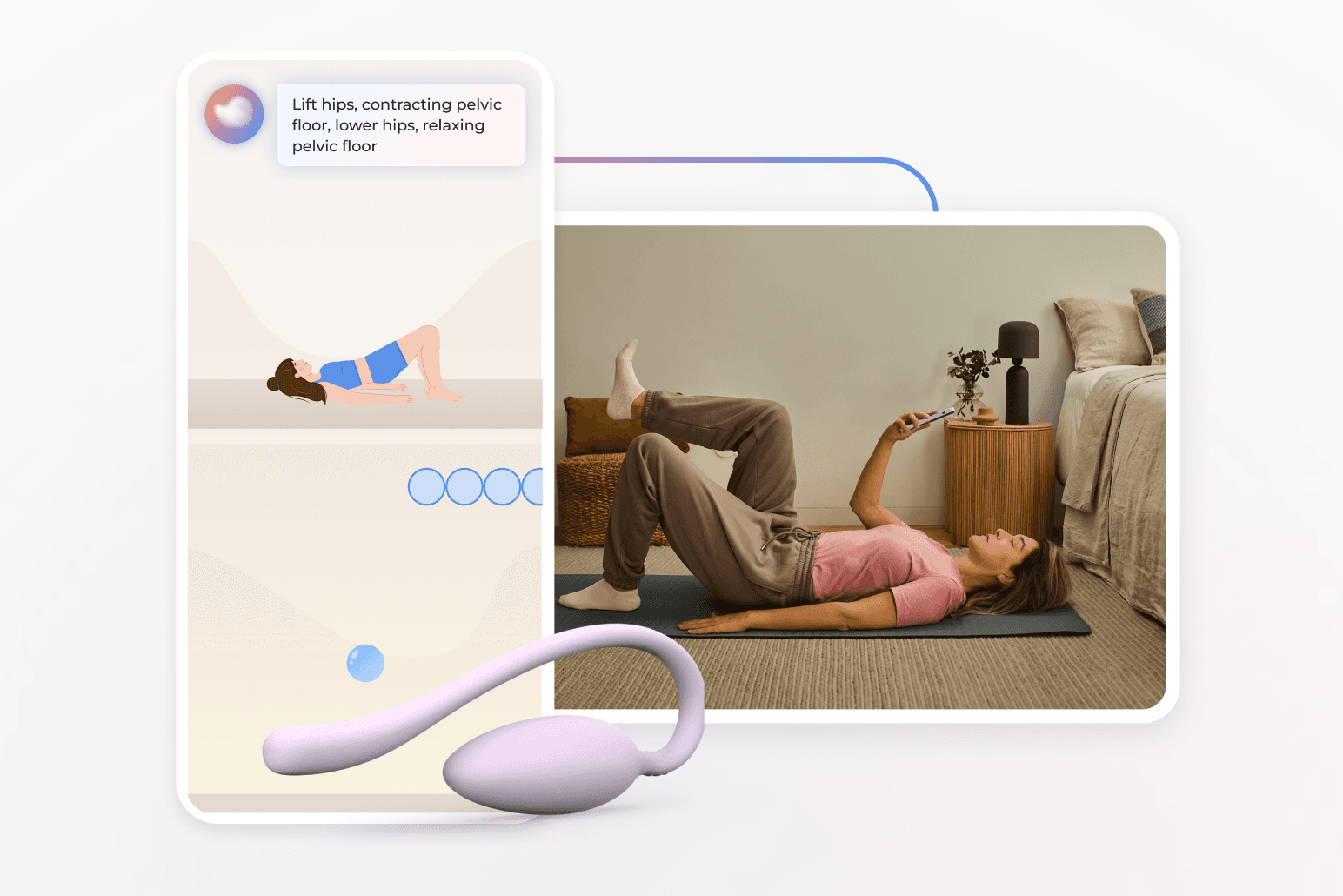
Sessions are short, discreet, and flexible. Because care is delivered virtually and members only need the Bloom pod and the Sword app, Bloom overcomes those access barriers to traditional in-clinic care. Women can work on their programs from the comfort and security of home at any time that suits their schedule. Nearly half take place outside standard business hours, and one in five happens on weekends.⁸ This leads to strong engagement and adherence levels, and better health outcomes as a result.⁸
Bloom's impressive member health outcomes
- Symptom improvement: 69% of members with moderate-to-severe conditions achieve meaningful relief.⁹
- Mental health benefits: Among members with baseline distress, 56% report improvement in anxiety and 50% report reduced depression.⁸
- High engagement and satisfaction: Average satisfaction among Bloom members is 9/10.¹⁰
- Daily confidence: Members report greater comfort, reduced disruption, and improved ability to participate fully at work and home.⁸
Bloom's proven return on investment makes for an easy choice
- Annual savings: $2,327 per member per year.¹¹
- ROI: 2.9:1 return, validated by independent actuarial review.¹¹
- Productivity: 50% improvement in productivity.⁸
- Surgery avoidance: Early therapy reduces the need for procedures averaging $29,000.⁵
- Equity impact: Nearly half of Bloom members come from high social deprivation areas yet achieve outcomes equal to peers.¹²
A turning point for women’s health at work
The rise of virtual pelvic floor therapy represents a transformation in how women’s health is supported at work. Employers have the opportunity to lead, offering solutions that are private, accessible, and clinically proven.
Bloom demonstrates what happens when technology and clinical expertise align: women regain health and confidence, while organizations save money and strengthen retention. The time to act is now, before costs escalate further. Support your elite female talent with stronger dedicated women's health benefits and start realizing the proven results.
FAQs about virtual pelvic floor therapy
What is telehealth pelvic therapy and how does it work?
Telehealth pelvic therapy is the delivery of pelvic floor therapy through digital platforms and virtual consultations. Instead of commuting to a clinic, members use secure apps and devices to complete exercises at home while receiving guidance from licensed pelvic health specialists. This model makes therapy more convenient, private, and scalable across employee populations.
How does remote pelvic PT compare to in-clinic sessions?
Remote pelvic PT provides the same clinical expertise as in-clinic sessions but removes the barriers of travel and scheduling. Members follow tailored exercise plans, use digital tools for real-time feedback, and connect with their therapist virtually for progress reviews. Adherence rates are often higher than traditional programs because therapy fits into daily life.
What is biofeedback kegel training?
Biofeedback kegel training uses a sensor device to measure pelvic floor muscle contractions during exercise. Members receive real-time feedback on whether they are engaging the muscles correctly, making the training far more effective than unsupervised exercises. Digital programs like Bloom integrate biofeedback into guided sessions, ensuring consistency and measurable progress.
Is at-home pelvic rehab safe and effective?
Yes. Clinical studies confirm that at-home pelvic rehab programs with professional oversight are safe and effective. Digital pelvic health solutions combine FDA-listed biofeedback devices, licensed therapists, and secure apps to provide comprehensive care. Members report significant improvements in symptoms, mental health, and workplace performance, while employers see cost savings and ROI.
Stop women suffering in silence with pelvic pain
Offer women life-changing support and slash claim costs with Bloom's digital pelvic care plans.
Footnotes
Kenne K, et al. Sci Rep. 2022;12:9878. doi:10.1038/s41598-022-13501-w.
Janela D, et al. JMIR mHealth & uHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Molina R, et al. Int J Gynecol Obstet. 2024;164(1):154–162. https://doi.org/10.1002/ijgo.14790
Patel KV, et al. Pain Reports. 2021;6(1):e913. https://doi.org/10.1097/PR9.0000000000000913
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi
Waetjen L, et al. Menopause. 2018;25(1):29–37. https://doi.org/10.1097/GME.0000000000000950
American Physical Therapy Association. Workforce Data Report. 2023. https://www.apta.org
Sword Health, Bloom Impact on Health Equity Whitepaper, 2024. https://swordhealth.com/insights/gated-reports/bloom-health-equity
Janela D, et al. JMIR mHealth & uHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Sword Health Member Data. Bloom member satisfaction scores (0–10 scale). Sword internal dataset, 2024.
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Sword Health. Bloom Health Equity Whitepaper. 2024. https://swordhealth.com/resources/whitepapers/Bloom_impact_on_health_equity