July 27, 2023 • min read
How proactive pain care prevents chronic pain
Pain is not always a stop sign. Learn how to recognize helpful versus harmful pain, modify activity, and maintain momentum during recovery.
Written by

Head of Clinical Strategy, Sword Move
Most people only think about pain when it forces them to stop. By that point, it is often costly, disruptive, and difficult to treat. A better approach is to address pain before it spirals. That is the foundation of proactive pain care, an approach centered on early education, structured assessment, and consistent healthy movement.
Instead of waiting for injuries to accumulate, proactive pain care helps people build resilience, strengthen awareness, and protect long-term wellbeing. This article explores why prevention of pain is so important, how pain education empowers people, and how proven frameworks like the PQRST pain assessment fit into the picture. You will also learn about the best program you can use to prevent pain with a proactive whole-body health plan that you can complete from the comfort of home.
Why proactive pain care has never been more important
Musculoskeletal (MSK) conditions are the number one healthcare cost driver in the United States, responsible for an estimated $381 billion in annual direct healthcare expenditures¹. Beyond the financial impact, MSK pain affects daily life, reduces productivity, and often coexists with anxiety or depression.
Research shows that nearly three in five U.S. adults experience some form of physical pain, ranging from acute discomfort to chronic conditions. About one in five adults live with chronic pain, and roughly 7–8% experience high-impact chronic pain that severely limits daily activities and work capacity. These individuals are also significantly more likely to experience depression or anxiety compared with those without chronic pain2.
In other words, pain is all too common, and pain hurts. Whether you have acute pain or chronic pain, it can be all-consuming. The impact of pain goes far and wide, affecting not just individuals, but also families, businesses, and communities.
The problem with the traditional, reactive healthcare approach to pain
In today’s world of medicine, the conversation around pain is usually about managing it. There’s a whole industry and medical speciality around helping people deal with their pain.
The traditional, reactive model has several challenges:
- Heavy reliance on medications, including opioids, for short-term relief
- Higher risk of unnecessary surgeries when early prevention is missed³
- A cycle of recurrence, as one in three people with lower back pain reinjure themselves within a year⁴
- Lost productivity and increased absenteeism for employers⁵
Proactive pain care flips the model. There is so much more you can do to prevent pain before it occurs and eliminate it (as opposed to just dealing with it) after it starts. By focusing on the prevention of pain, you can stay healthy, reduce your healthcare costs and improve the quality of life. This means focusing on education, early assessment, and consistent, safe movement.
What is pain?
Pain is a feeling, a sensation, a message from our brain that something is not right. Aching, burning, throbbing—these are all words used to describe how pain feels and how our body interprets the messages from our brain.
Acute vs chronic pain
Pain can come in many forms, but is generally grouped into two categories, as explained in this detailed acute vs chronic MSK conditions guide.
- Acute pain comes on suddenly to warn the body of an imminent threat—for instance, the sharp pain of breaking a bone or spraining an ankle. Acute pain usually resolves when the underlying cause, or threat, is no longer present.
- Chronic pain is pain that lasts longer than three months. Often the result of illnesses such as arthritis or cancer, chronic pain can occur in any part of the body and last for months or years, severely impacting quality of life for those who suffer from it.
In some cases, acute pain can evolve into chronic pain, especially if the cause of the acute pain is overlooked or not treated in a timely and appropriate manner.
The role of pain education in prevention of pain
Pain education is one of the most effective and underutilized tools in healthcare. At its core, it is about giving people the knowledge to understand how pain works, why it happens, and how they can influence it.
Effective pain education helps people:
- Understand the difference between acute and chronic pain
- Identify common triggers and early warning signs
- Recognize lifestyle factors that contribute, such as poor posture, stress, or inactivity
- Develop confidence in self-care strategies
Evidence shows that pain education reduces fear, improves coping skills, and helps people engage more effectively in treatment programs⁶. For employers and health plans, it means equipping members with the insight to act earlier, reducing claims and improving satisfaction. But you can also educate yourself on proactive healthcare and pain prevention.
Sword Move is the ideal program you can use to build whole-body strength and proactively prevent against pain and injury. Learn more about how Move works and check to see if you are already covered to enroll to get your own personalized Move program within your existing health plan.
What is the PQRST pain assessment and how do clinicians use PQRST?
Assessment is the bridge between awareness and action. The PQRST pain assessment is one of the most widely used clinical tools to evaluate pain.
- P – Provoking/Palliative: What makes the pain worse? What provides relief?
- Q – Quality: Is it sharp, dull, throbbing, burning, or stabbing?
- R – Radiates/Region: Where is the pain located? Does it spread to other areas?
- S – Severity: How intense is the pain, often rated on a 0–10 scale?
- T – Time/Timing: When did it begin? How often does it occur?
The assessment of pain with PQRST provides a structured way to capture the full experience of pain. For example, a patient might describe sharp lower back pain (Quality, Region) that worsens when lifting (Provoking), improves with rest (Palliative), rates as an “8” (Severity), and has been occurring for two weeks every evening (Time).
This detail not only guides clinical decisions but also empowers individuals. When people are educated to self-assess with frameworks like PQRST, they become active participants in their care, improving communication with providers and supporting prevention of pain.
How movement and early intervention prevent pain
Education is powerful, but it must be paired with action. Movement is the single most important behavior for preventing MSK conditions.
Low levels of physical activity are responsible for up to 50% of MSK conditions and significantly increase risk for other chronic diseases⁷. In contrast, regular physical activity:
- Prevents one in three MSK conditions⁸
- Reduces the risk of premature death by 30%⁹
- Decreases the likelihood of falls in older adults by up to 26%¹⁰
- Improves mental health, with effectiveness comparable to medication in reducing depression and anxiety¹¹
The evidence is clear: prevention of pain is possible, but it requires safe, consistent, and supported movement.
How Sword Move delivers proactive pain care at home
The challenge is that most people do not have time to attend frequent in-person programs. Sword Move solves that barrier by bringing proactive pain care into the home.
Move is the only whole-body digital solution designed to prevent MSK pain, reduce injury risk, and encourage healthier daily movement. It is built to be flexible, accessible, and clinically validated.
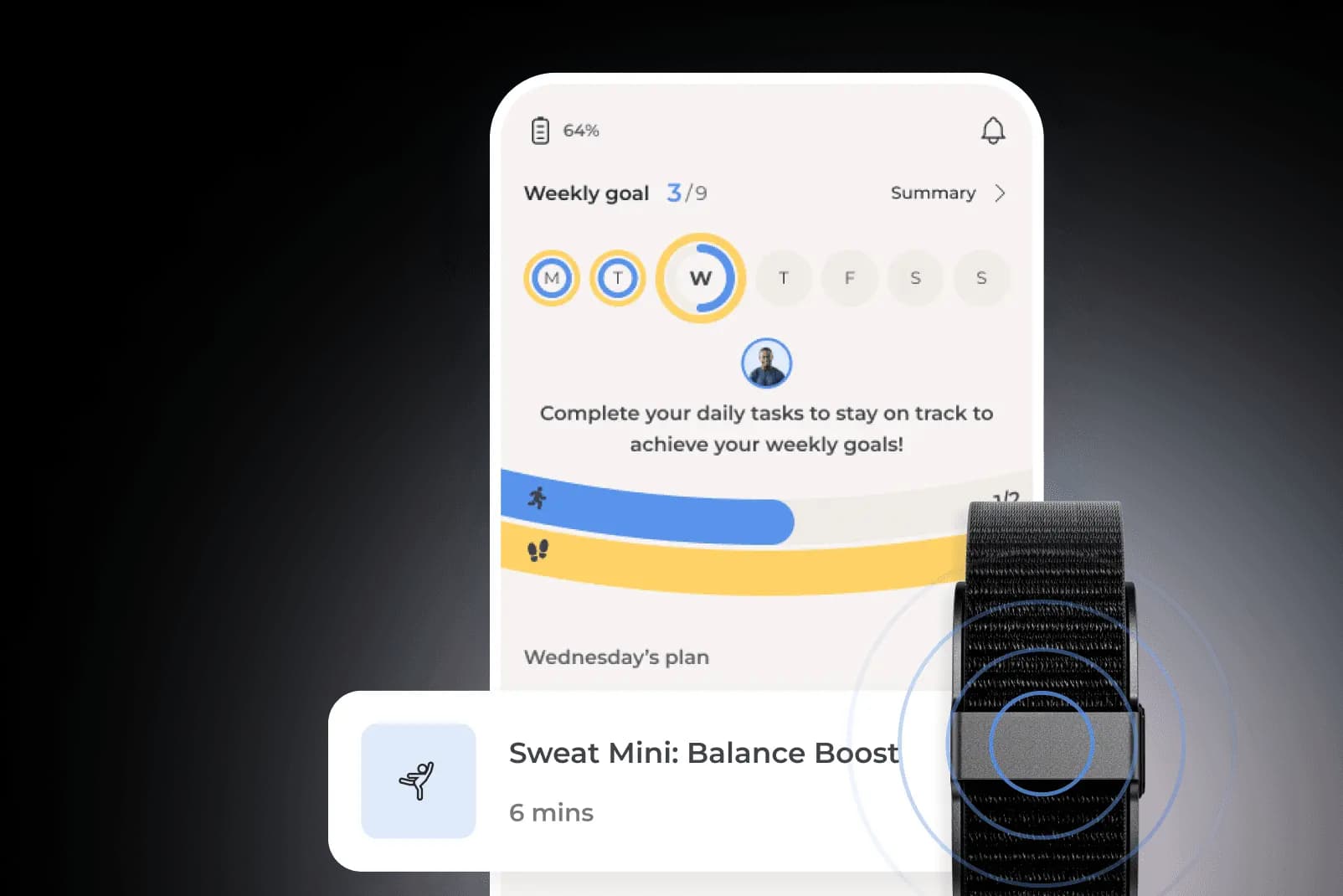
How Move works
- Members receive the Move Kit, which includes the Move Wearable, resistance bands, and step-by-step guidance.
- The Move Wearable tracks activity, steps, heart rate, and sleep, while providing real-time, accurate feedback during guided activities.
- You get a personalized Move Plan tailored by your matched Physical Health Specialists, who all hold a Doctor of Physical Therapy degree.
- Progress is tracked through regular assessments, ensuring safe and sustainable results.
- Each week, you’ll receive a new Move Plan that you can complete from home in minutes, at any time of the day or night
Move is proven to prevent pain for body and mind
- 74% of members report improved self-reported overall health quality¹²
- 49% fewer members show risk for developing anxiety disorder after using Move¹²
- 74% of members report feeling "moderately better" or "much better" overall¹²
- 69% upgraded to healthy active at 10-weeks of Move¹²
- Half of all sessions take place outside of standard hours, proving its accessibility for busy lives¹²
Move's accessible, 24/7 digital delivery model makes it so easy for anyone to take ownership of their MSK health. You can work on your personalized preventative care plan on your own terms, without having to travel to the gym or invest in any expensive equipment.
Build whole-body strength with Sword Move
With Sword Move, you can say goodbye to daily aches and pains and proactively prevent pain with lasting movement habits that actually stick. Your preventative whole-body care plan will reduce costs, improve your long-term health outcomes, and empowers you with the whole-body strength.
Move may already be covered within your existing employee benefits plan or by your health insurer at zero additional cost to you. Check today to see if you are covered and get started right away.
Recover from the comfort of home with clinically-proven care
Sword’s care programs may already be covered in your health plan at $0 cost to you.
Footnotes
Dieleman JL, Cao J, Chapin A, et al. US healthcare spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863-884. doi:10.1001/jama.2020.0734. https://jamanetwork.com/journals/jama/fullarticle/2762309
Dahlhamer J., Lucas J., Zelaya C., et al. (2018). Prevalence of chronic pain and high-impact chronic pain among adults — United States, 2016. JAMA Network Open, 1(8):e184447. doi:10.1001/jamanetworkopen.2018.4447;Koller D., et al. (2023). Association between chronic pain and risk of depression: A population-based study. JAMA Network Open, 6(1):e2251214. doi:10.1001/jamanetworkopen.2022.51214.
Eriksen J, Sjøgren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain: an epidemiological study. J Pain Symptom Manage. 2006 Sep;32(3):223-235. doi:10.1016/j.jpainsymman.2006.05.012. https://pubmed.ncbi.nlm.nih.gov/16939842/
Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Healthcare (Basel). 2022;10(8):1595. doi:10.3390/healthcare10081595. https://www.mdpi.com/2227-9032/10/8/1595
Dzakpasu FQS, Carver A, Brakenridge CJ, et al. Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021;18:159. doi:10.1186/s12966-021-01191-y. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-021-01191-y
da Silva T, Mills K, Brown BT, Herbert RD, Maher CG, Hancock MJ. Risk of recurrence of low back pain: a systematic review. Musculoskelet Sci Pract. 2023;63:102709. doi:10.1016/j.msksp.2022.102709. https://www.sciencedirect.com/science/article/pii/S2468781222001355
Traeger AC, Lee H, Hübscher M, et al. Effect of intensive patient education vs placebo patient education on outcomes in patients with acute low back pain: a randomized clinical trial. JAMA Neurol. 2015;72(12):1613-1621. doi:10.1001/jamaneurol.2015.2567. https://jamanetwork.com/journals/jamaneurology/fullarticle/2450098
Dzakpasu FQS, Carver A, Brakenridge CJ, et al. Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021;18:159. doi:10.1186/s12966-021-01191-y. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-021-01191-y
Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Am J Epidemiol. 2018;187(5):1093-1101. doi:10.1093/aje/kwx337. https://pubmed.ncbi.nlm.nih.gov/29596520/
Booth FW, Laye MJ, Roberts CK. Lifetime sedentary living accelerates some aspects of secondary aging. Compr Physiol. 2012 Apr;2(2):1143-1211. doi:10.1002/cphy.c110025. https://pubmed.ncbi.nlm.nih.gov/23798298/
Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2019;53(17):905-911. doi:10.1136/bjsports-2019-100732. https://bjsm.bmj.com/content/53/17/905
Pearce M, Garcia L, Abbas A, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. Br J Sports Med. 2023;57(15):979-989. doi:10.1136/bjsports-2022-106195. https://bjsm.bmj.com/content/57/15/979
Sword Health. Move Book of Business Results. Internal analysis, H1 2024.