October 20, 2025 • min read
How to manage perimenopause symptoms with confidence
Learn how to manage, reduce, and even prevent pain and discomfort during perimenopause. Discover what’s normal, why symptoms occur, and when you should escalate for medical support.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
Perimenopause is the gradual transition leading up to menopause, often beginning in your 40s but sometimes earlier. During this stage, estrogen and progesterone levels fluctuate, causing physical and emotional changes that may feel unfamiliar.
- Common signs of perimenopause: include irregular periods, cramps, bloating, fatigue, mood shifts, and pelvic pressure. These changes are part of the body’s natural hormonal rhythm and not something to fear.
- Advice to manage perimenopause: while perimenopause affects everyone differently, tracking your cycle and symptoms can help you recognize patterns and feel more in control. Regular movement, good nutrition, hydration, and rest support balance. Emotional health matters too; mindfulness, open conversations, or short relaxation breaks can reduce stress and help you feel grounded.
- When to get medical support: It’s important to seek guidance if you notice persistent pain, heavy bleeding, urinary changes, or fatigue that interferes with daily life. Early support can make this phase smoother and prevent ongoing discomfort.
Perimenopause is an overlooked phase of menopause
It might start with a missed period, a night of restless sleep, or cramps that feel unfamiliar. These subtle changes often cause confusion, but they are a natural sign that your body is entering perimenopause.
Perimenopause typically begins in a woman’s 40s, although some experience it earlier⁷. Despite how common it is, many women do not realize how much their mood, energy, and comfort can shift during this stage. Understanding what is happening helps you feel more in control and better prepared to support your health. Once you understand the “why,” it becomes easier to find the “how,” and the right support can make all the difference.
What is perimenopause?
Perimenopause is the transition before menopause when estrogen and progesterone levels begin to fluctuate⁸. These hormonal changes affect much more than your cycle. They can influence mood, sleep, digestion, bone density, and even the muscles that support your bladder and pelvic organs⁸.
You may notice that your periods become irregular or your flow changes. You may experience new sensations, such as heat at night, tenderness, or irritability that comes and goes⁹.You might even experience more frequent cramps during perimenopause and an increase in joint pain during this period. These are all normal physiological responses to changing hormone levels.
This stage is not an illness but a natural transition. With the right information and support, most women can navigate perimenopause with comfort and confidence.
What are the early signs and symptoms of perimenopause?
Every woman’s experience is unique, but these are some of the most common signs:
- Irregular or heavier menstrual cycles
- Cramps or bloating between periods
- Breast tenderness or water retention
- Hot flashes or night sweats⁹
- Fatigue or 'brain fog'
- Mood fluctuations or increased anxiety⁹
- Vaginal dryness or discomfort during intimacy
- Pelvic heaviness, bladder leaks, or bowel changes
Hormonal changes can also affect the pelvic floor, leading to sensations of pressure or mild leakage¹¹. One in three women experience pelvic floor dysfunction¹, and about 32% report urinary incontinence². These symptoms are common but manageable with the right care.
Remember every woman’s experience of perimenopause is different
No two experiences of perimenopause look the same. Some women notice minimal changes, while others feel that their bodies have transformed. Lifestyle, genetics, and stress levels can all influence how symptoms appear¹⁰.
Estrogen fluctuations affect connective tissue and muscle tone, including the pelvic floor. This can create both physical and emotional symptoms. You may feel less steady in your body or more easily fatigued. Recognizing that these changes are normal helps you respond with compassion and confidence.
When you understand what your body is doing, you can meet it with patience instead of frustration. That understanding is a form of self-care in itself.
When to seek care and why early support matters
Many women delay seeking care for perimenopause symptoms. Research shows it takes an average of 6.5 years for women to seek help for pelvic floor symptoms, even when those symptoms interfere with daily life¹². Early support helps manage discomfort before it affects well-being and productivity.
You should seek guidance if you experience:
- Heavy or prolonged bleeding
- Ongoing pelvic pressure or discomfort
- Bladder leakage or urinary urgency
- Pain during intimacy
- Noticeable mood changes, sleep disruption, or fatigue
Even mild symptoms are worth addressing. Seeking care early helps prevent complications and supports long-term well-being.
What to expect and how to stay healthy during perimenopause
Perimenopause is a natural stage of life, not a sign that something is wrong. It’s a gradual transition as your hormones shift, and while some changes may feel new or unexpected, they are a normal part of your body’s evolution. Understanding what’s happening can help you respond with confidence instead of concern.
1. Support your physical health: Gentle, regular movement such as walking, yoga, or low-impact strength training helps maintain bone density, circulation, and muscle tone. Focus on nutrient-rich foods that include calcium, magnesium, lean protein, and omega-3 fats to support energy and hormone balance. Prioritize hydration and consistent sleep, and consider moderating caffeine or alcohol if they worsen sleep or hot flashes.
2. Care for your emotional well-being: Mood changes and anxiety are common during hormonal transition, but they don’t define this stage of life. Talking about your experience with trusted people or a healthcare provider can help normalize what you’re feeling. Many women also find that practices like mindfulness, breathing exercises, or journaling help bring calm and stability.
3. Know that pelvic care programs can reduce symptoms: For too long, women were told to simply “push through” perimenopause symptoms. Today, dedicated women’s health programs are changing that. Evidence-based pelvic care options are designed to help relieve discomfort, improve muscle function, and restore confidence.
How Bloom supports you through perimenopause
Bloom is a digital women’s health care program created to support women in every life stage, including perimenopause.
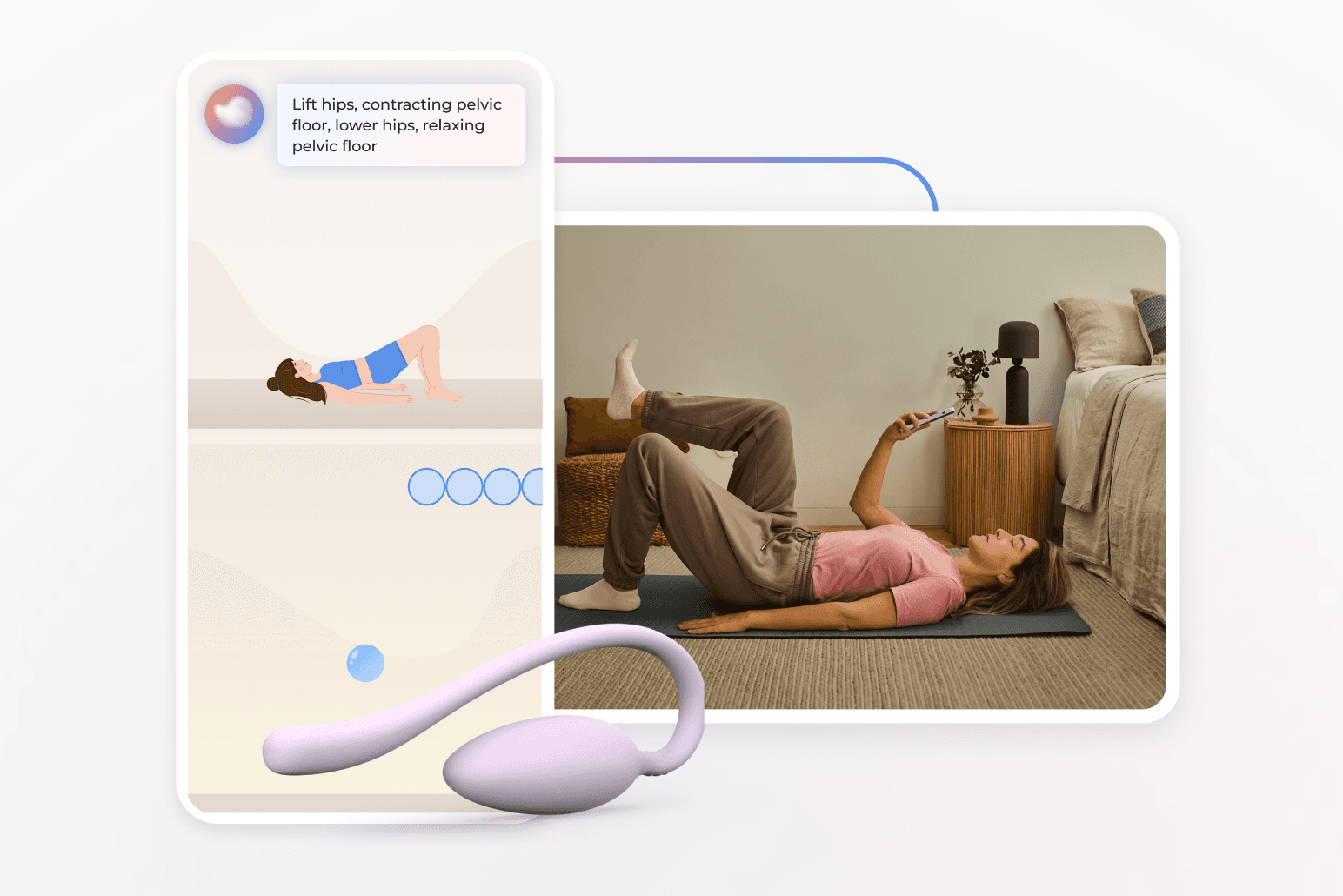
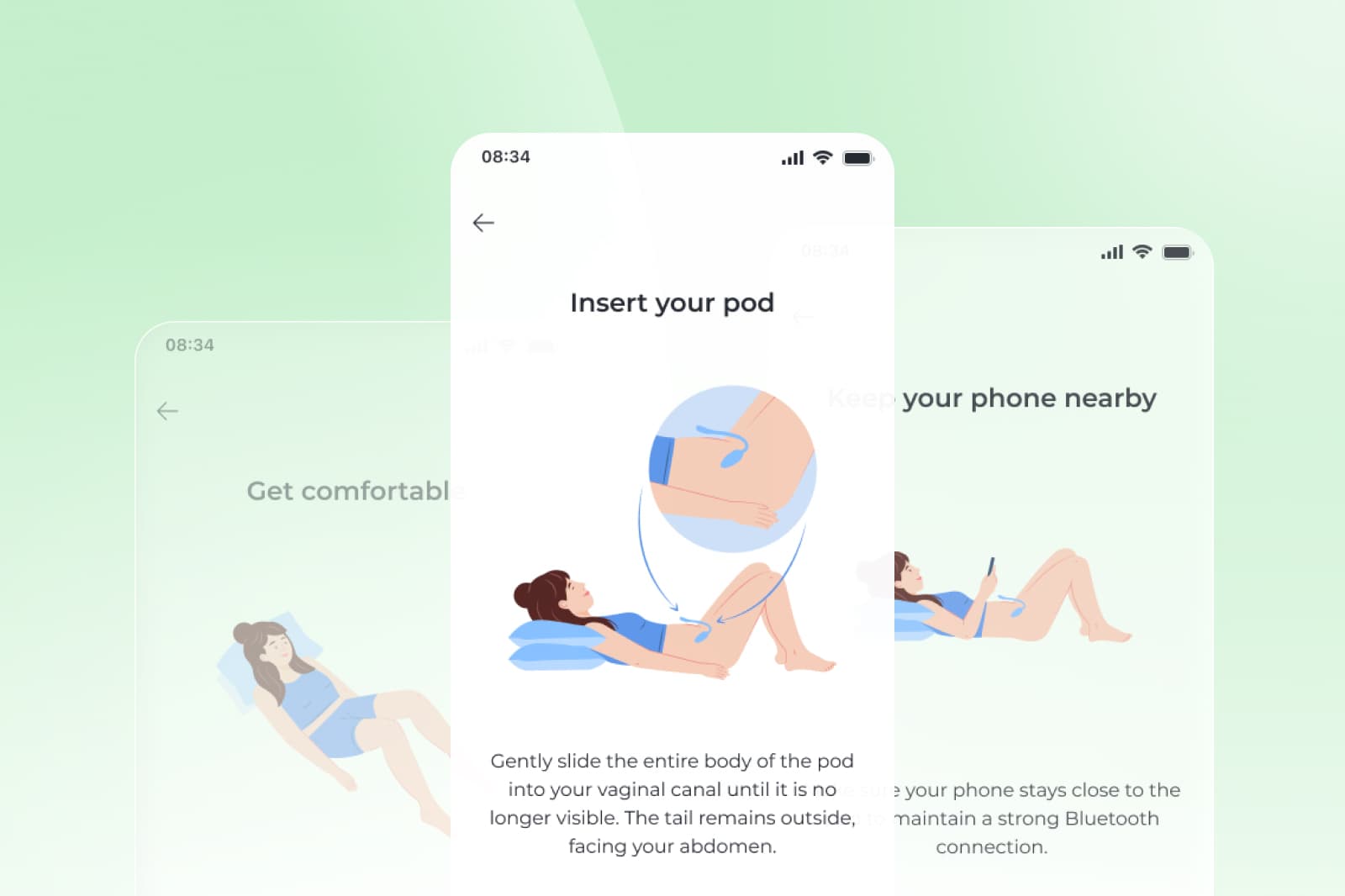
Members are paired with a Women’s Health Specialist holding a Doctor of Physical Therapy degree, who designs a personalized pelvic care plan. Through the Sword Health app, members complete customized sessions that fit easily into their day. The optional Bloom Pod, a safe, FDA-listed biofeedback sensor, measures muscle movement and provides real-time feedback.
Each session takes about 10 to 15 minutes and can be done anywhere, anytime. Programs evolve based on your goals and progress. Bloom’s impact is measurable and significant:
- 65% of women report meaningful improvement in daily life³
- 56% experience better productivity and 50% report reduced anxiety⁴
- 77% complete their program, far exceeding typical in-person adherence rates⁵
Small, consistent steps lead to big change, especially when guided by an expert who understands women’s health.
Get started with Sword Bloom in 4 easy steps
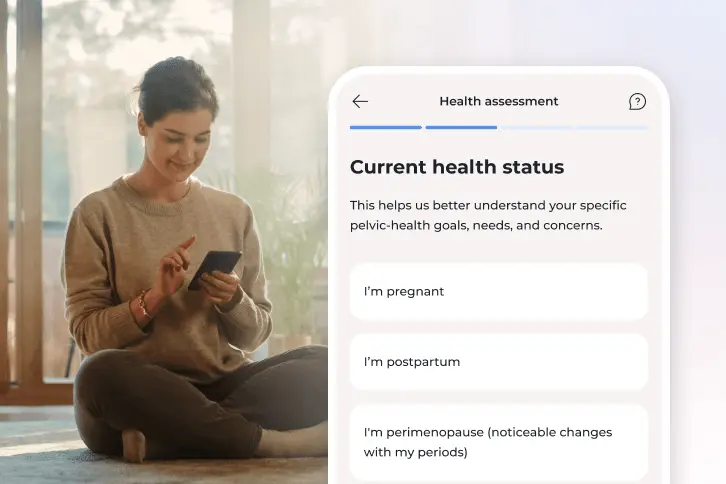
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
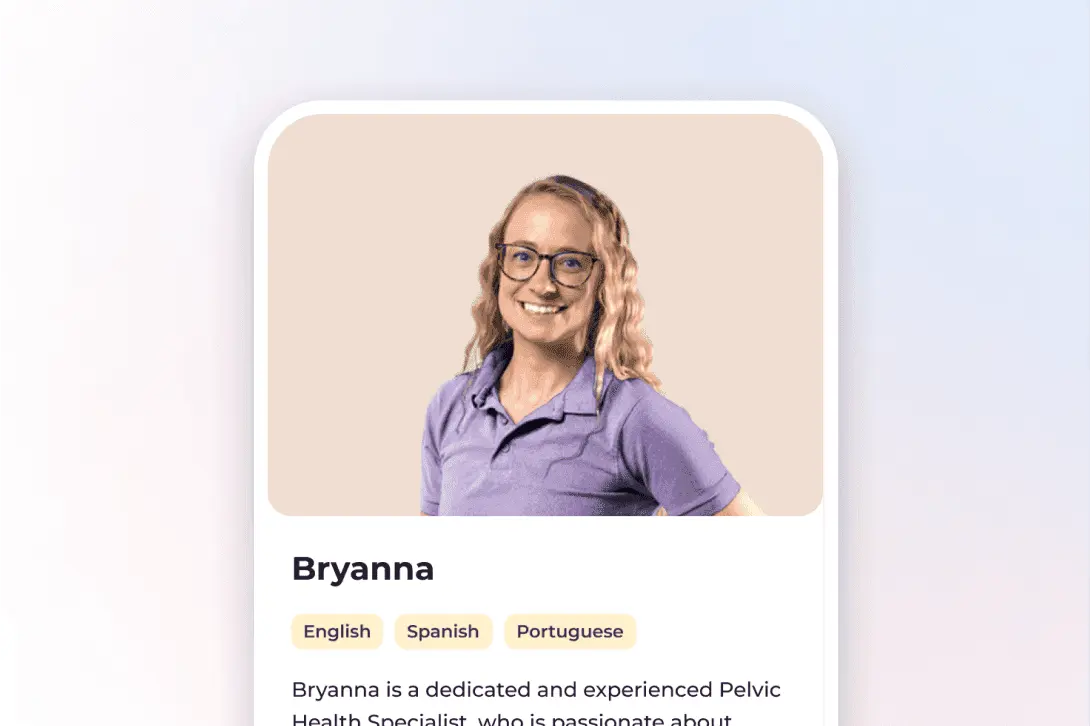
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Why Bloom works when traditional care is harder to reach
Many women who want help never get it. Pelvic care specialists are limited, and clinic appointments can require time off work or long travel. Others feel uncomfortable discussing private symptoms face-to-face.
Bloom removes these barriers. You can start from home, on your schedule, and stay connected with your Women’s Health Specialist through the Sword mobile app. About half of all Bloom sessions occur after working hours, and one in five take place on weekends⁶.
This flexibility makes Bloom accessible to women everywhere. Nearly half of members live in higher-deprivation areas yet achieve the same outcomes and satisfaction levels as others⁶. Bloom is safe, inclusive, and built for women of all ages.
How to get started with Bloom to better manage your symptoms
Many employers and health plans now include Bloom as a covered benefit¹¹. You may have already coverage within your health insurance to access personalized pelvic and musculoskeletal care at no cost to you.
Checking your eligibility is simple:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Kenne DR, et al. Scientific Reports. 2022;12:9878. https://doi.org/10.1038/s41598-022-13501-w
Kołodyńska G, et al. Menopause Review. 2019;18(2):56–63. https://doi.org/10.5114/pm.2019.87605
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Janela D, et al. JMIR mHealth & uHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Janela D, et al. Healthcare. 2024;12(2):141. https://www.mdpi.com/2227-9032/12/2/141
Sword Health. Bloom Health-Equity Whitepaper. 2024. https://swordhealth.com/resources/whitepapers/bloom-impact-on-health-equity
Avis NE, et al. JAMA Internal Medicine. 2015;175(4):531–539. https://doi.org/10.1001/jamainternmed.2014.806
Angelou K, et al. Cureus. 2020;12(4):e7586. https://doi.org/10.7759/cureus.7586
Freeman EW, et al. Menopause. 2014;21(6):602–611. https://doi.org/10.1097/GME.0000000000000149
Dennerstein L, et al. Psychoneuroendocrinology. 2007;32(Suppl 1):S57–S64. https://doi.org/10.1016/j.psyneuen.2007.03.011
Bø K, et al. Neurourology and Urodynamics. 2018;37(7):2271–2272. https://doi.org/10.1002/nau.23709
Lukacz ES, et al. Urologic Nursing. 2005;25(2):109–115. https://pubmed.ncbi.nlm.nih.gov/15900979