October 20, 2025 • min read
Frequent urination in menopause: causes and relief
Learn why menopause can cause frequent urination and how Bloom helps women strengthen bladder control to regain confidence and control.
Written by

Senior Clinical Program Manager, Sword Bloom ·
The Sword Summary Warm-up
Don’t have time for the full workout? We’ve got you covered with a quick, high-intensity session. Here are the key takeaways:
- Urinary changes are common during menopause and can include increased frequency, urgency, or waking at night to urinate.
- These shifts happen because estrogen supports the bladder, urethra, and pelvic floor muscles, all of which help maintain bladder control and comfort.
- Understanding what causes these changes helps you take simple, effective steps to regain confidence and reduce disruptions to your day and sleep.
Bloom provides expert-guided pelvic care to help women strengthen bladder support, improve confidence, and stay comfortable, safely from home and often at no cost through their health plan.
When urinary changes start to disrupt your routine
You might first notice small changes such as waking up once or twice a night to use the bathroom, feeling like you need to go more often during the day, or worrying about finding restrooms when you are out. These patterns are very common in perimenopause and menopause, when hormone fluctuations influence how the bladder and pelvic floor function¹.
For many women, these shifts begin gradually during perimenopause, the years leading up to menopause. Hormonal fluctuations can make bladder control less predictable and may cause sensations of urgency or increased frequency, even without a full bladder¹. While this can feel frustrating, it is not unusual or permanent.
Understanding what causes these changes is the first step to managing them effectively and restoring a sense of control.
Why menopause and perimenopause can cause frequent urination
Hormonal and structural changes influence how the bladder and urinary system function. Each part of this system—the bladder, urethra, and pelvic floor muscles—depends on estrogen for elasticity and muscular tone². Estrogen receptors in these tissues help maintain flexibility, strength, and nerve sensitivity. As hormone levels decline, tissues can lose support and elasticity, affecting bladder control³.
How hormonal changes affect bladder health
Estrogen supports the flexibility and thickness of the tissues that line the bladder and urethra. It helps these areas stay hydrated and responsive. As estrogen levels decline, the lining can become thinner, the muscles less elastic, and the nerves more sensitive². These changes can lead to sensations of urgency or reduced bladder capacity³.
Nighttime urination (nocturia) becomes more common because hormonal shifts affect how the kidneys regulate fluid and sodium balance⁴.
How pelvic floor strength supports bladder control
The pelvic floor is a group of muscles that provide foundational support for the bladder and urethra. During menopause, these muscles can weaken, affecting the bladder’s ability to store urine comfortably. Weak or uncoordinated muscles may also make you feel sudden urgency when you laugh, cough, or lift something⁵.
Targeted strengthening helps restore coordination and stability. The earlier this support begins, the more effective it can be.
Hydration, caffeine, and your bladder
What and how you drink plays a major role in bladder comfort. Caffeine, alcohol, and carbonated drinks can increase activity in the bladder muscle, making urges stronger⁶. However, reducing fluids too much can backfire. Concentrated urine irritates the bladder lining and triggers more frequent urges⁷.
Simple hydration habits that help:
- Sip water throughout the day instead of drinking large amounts at once.
- Choose water or herbal teas instead of soda or coffee.
- Limit caffeine and alcohol, especially in the afternoon.
- Avoid drinking large volumes within two hours of bedtime.
Balanced hydration helps your bladder function properly, keeps urine less concentrated, and flushes potential irritants⁸.
How perimenopause affects urinary frequency
During perimenopause, estrogen levels rise and fall unpredictably, temporarily affecting the bladder and pelvic floor⁹. Some women notice periods of urgency or mild leakage that may disappear for weeks. These are not signs of infection or damage. They reflect how the bladder responds to shifting hormones and changing tissue sensitivity¹⁰. During this time, the muscles may tighten or fatigue more quickly, making bladder control feel inconsistent.
Early attention to these changes makes a real difference. Gentle pelvic strengthening, steady hydration, and regular movement help stabilize bladder pressure and prevent symptoms from persisting later in menopause¹¹. This proactive approach makes it easier to maintain comfort and confidence through the transition years.
4 ways to manage frequent urination during menopause
The good news is that urinary frequency is highly manageable with consistent habits, pelvic strengthening, and awareness of triggers. The following steps help restore comfort and control.
1. Strengthen bladder and pelvic support
The pelvic floor muscles are central to bladder control. When they activate effectively, they help the bladder fill and empty smoothly. When weak or uncoordinated, the bladder works harder, increasing urgency.
How to support these muscles:
- Practice gentle pelvic floor activation. Lightly tighten the muscles you would use to stop urine flow, then release. Focus on steady breathing.
- Build consistency. Short daily practice often leads to noticeable improvement within weeks when done correctly¹².
- Seek expert guidance. Bloom offers expert pelvic care with personalized programs designed by Women’s Health Specialists who hold Doctor of Physical Therapy degrees.
2. Revisit your hydration and daily habits
It can be tempting to drink less water when you feel like you are using the bathroom frequently, but reducing fluid intake can make symptoms worse. Concentrated urine irritates the bladder and triggers more frequent urges¹³.
Try this routine:
- Sip water consistently throughout the day rather than in large amounts at once.
- Limit caffeine, alcohol, and fizzy drinks that stimulate the bladder.
- Avoid large fluid intake within two hours of bedtime.
Hydration supports your bladder’s natural function, helps flush irritants, and reduces the sensation of urgency¹².
3. Support tissue health and hormonal balance
Estrogen supports the health of the urethra and bladder tissues. Declining estrogen can make the urethra and bladder tissues thinner and more sensitive¹⁴.
For some women, local estrogen creams or vaginal preparations prescribed by a clinician can help restore tissue health and comfort¹⁵. These options should be discussed with a healthcare provider to ensure safety and fit.
Non-hormonal support such as pelvic strengthening, hydration, and regular movement also helps maintain healthy circulation and tissue integrity around the bladder¹⁵..
4. Adjust your lifestyle for comfort and sleep
Stress, fatigue, and poor sleep can make urinary symptoms feel more intense. When you are tired, your body produces more cortisol, a stress hormone that increases inflammation and bladder sensitivity¹⁶.
Practical steps to support your body:
- Prioritize rest. A consistent bedtime routine regulates hormones and reduces nighttime urges.
- Move daily. Gentle exercise supports circulation and fluid balance.
- Manage stress. Breathing exercises, mindfulness, or short walks can relax pelvic tension.
A calm, rested body supports better bladder function and helps you feel more in control. Caring for your whole body will also help you restore your confidence.
When should you escalate bladder problems and seek care from a doctor?
Frequent urination is common, but there are times when professional evaluation is important. Speak with a clinician if you experience any of the following:
- Pain, burning, or blood in your urine
- Persistent leakage or pelvic pressure
- Sudden, complete loss of bladder control
- Fever, back pain, or chills
These symptoms may signal a urinary tract infection, inflammation, or pelvic organ prolapse. A clinician can confirm what is happening and recommend safe, effective next steps.
If your symptoms are mild but disruptive, consider an early consultation or a guided pelvic care program. Addressing bladder changes early helps prevent them from becoming chronic and protects your long-term pelvic health¹⁷.
How Bloom’s at-home care helps you reduce leakage
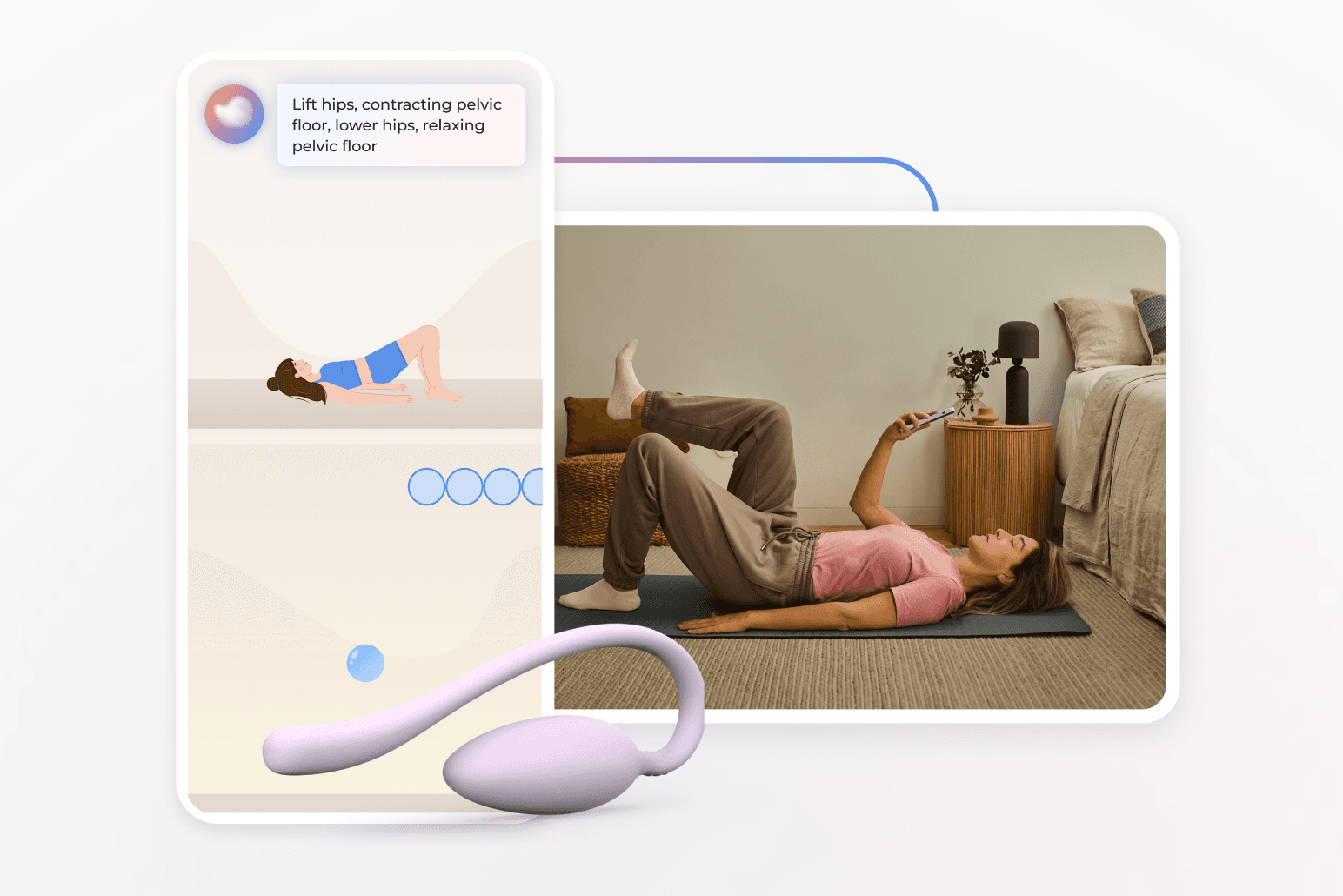
Bloom is a dedicated digital women’s health care program that helps women strengthen bladder and pelvic support safely from home.
Each member is paired with a Women’s Health Specialist with a Doctor of Physical Therapy degree, who designs a personalized care plan for each member. The plan is built based on your specific symptoms and health goals, with targeted exercises focused on pelvic strength, coordination, and confidence.
Bloom programs are designed around your schedule. Sessions last just 10–15 minutes and can be done anywhere. All you need is the Sword mobile app and the Bloom Pod, an FDA-listed biofeedback device that provides real-time guidance. Bloom is safe, discreet, and accessible to you 24/7.
Get started with Sword Bloom in 4 easy steps
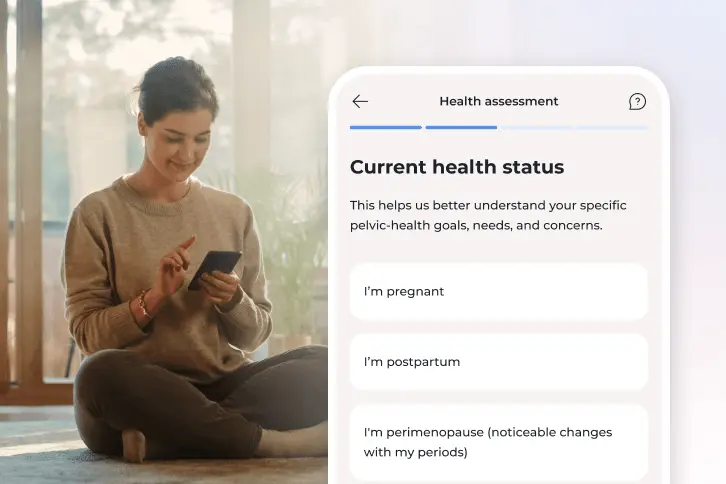
1. Tell us about you
Share your symptoms, health history, and goals so we can personalize your care.
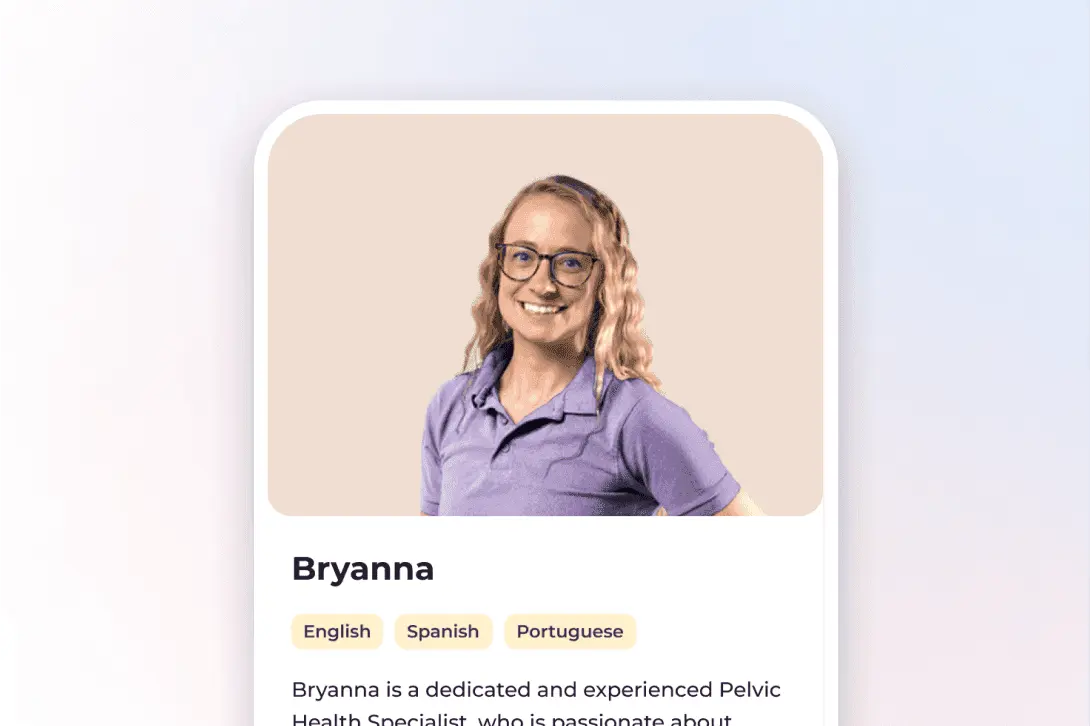
2. Meet your clinician
You’ll be matched with a Pelvic Health Specialist who will guide your recovery and adjust your plan as you go.
3. Receive your Bloom kit
We’ll ship everything you need, including the Bloom Pod, directly to your door.
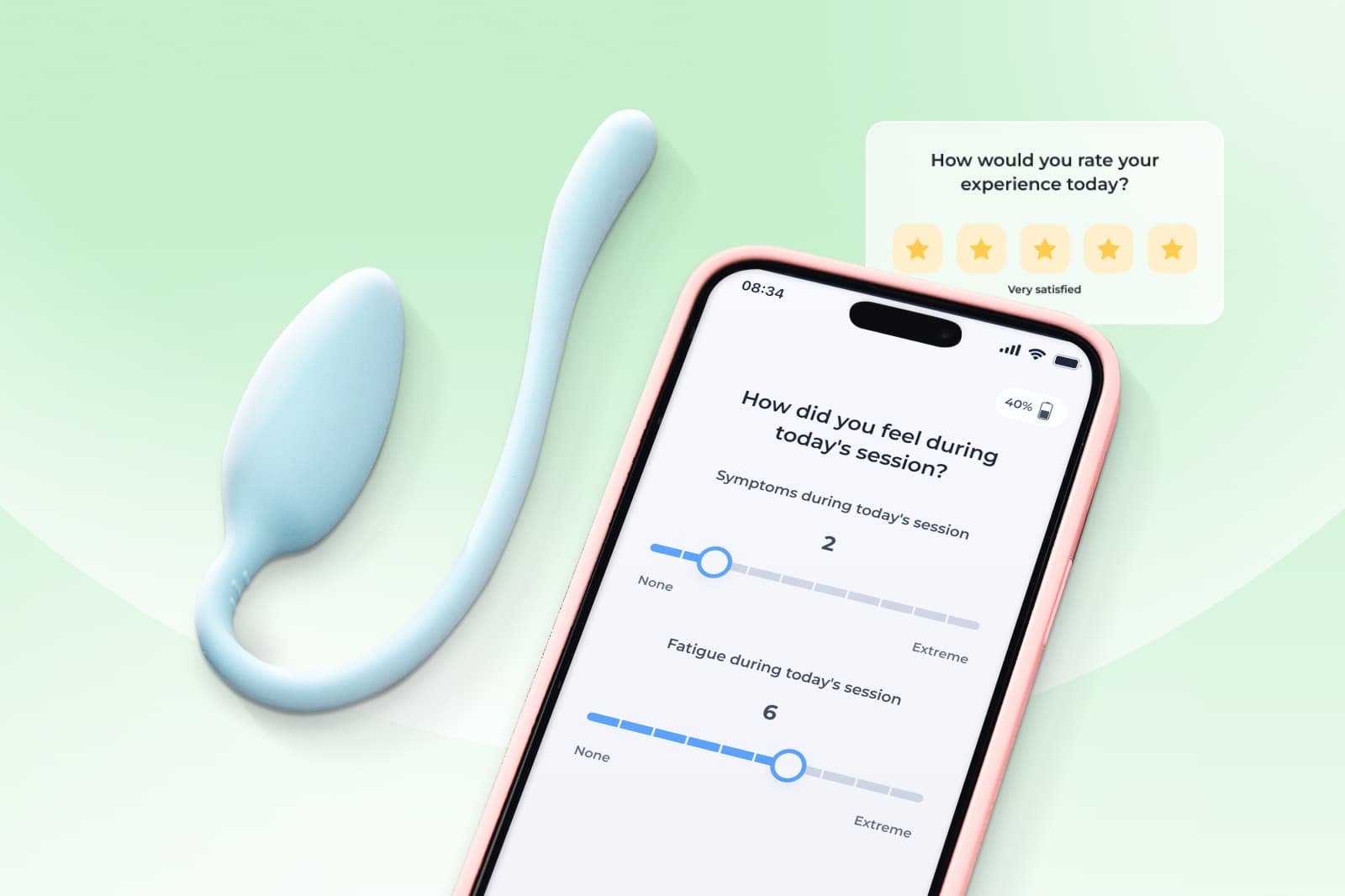
4. Begin your recovery at home
Get expert support and real-time feedback, all from the privacy of home.
Why Bloom works when traditional care is harder to reach
Many women who want help never get it. Pelvic care specialists are limited, and clinic appointments can require time off work or long travel. Others feel uncomfortable discussing private symptoms face-to-face.
Bloom removes these barriers. You can start from home, on your schedule, and stay connected with your Women’s Health Specialist through the Sword mobile app. About half of all Bloom sessions occur after working hours, and one in five take place on weekends⁶.
This flexibility makes Bloom accessible to women everywhere. Nearly half of members live in higher-deprivation areas yet achieve the same outcomes and satisfaction levels as others⁶. Bloom is safe, inclusive, and built for women of all ages.
Bloom's tens of thousands of members continually report impressive results:
- 65% report improvement in daily comfort and bladder confidence¹⁸
- 77% complete their care programs successfully¹⁹
- Members across diverse age and income groups achieve equivalent outcomes²⁰
With Bloom, care is private, empowering, and accessible. You can build strength and regain confidence on your own terms.
How to get started with Bloom to regain control of your symptoms
Bladder changes during menopause are common, but they do not have to define your daily life. With consistent care and the right support, your body can adapt and regain control. Bloom is purpose-built to make expert pelvic care accessible, discreet, and effective for women in every stage of life.
Many employers and health plans now include Bloom as a covered benefit. You may have already coverage within your health insurance to access personalized pelvic care at no cost to you.
Checking your eligibility is simple and it takes just a few clicks:
- Check to see if your insurer has coverage for Bloom.
- Enter your employer or insurance details.
- If covered, you can begin your personalized care program within days.
Join 500,000+ people using Sword to end their pain
Recover from pain from the comfort of your home with clinically-proven expert care
Footnotes
Robinson D, et al. Menopause International. 2013;19(2):69–75. https://doi.org/10.1177/1754045313485482
Robinson D, et al. Climacteric. 2021;24(4):379–387. https://doi.org/10.1080/13697137.2020.1852265
Long CY, et al. Taiwanese Journal of Obstetrics & Gynecology. 2008;47(2):178–183. https://doi.org/10.1016/S1028-4559(08)60078-1
Robinson D, et al. Menopause. 2020;27(9):1045–1053. https://doi.org/10.1097/GME.0000000000001564
Dallosso HM, et al. BJU International. 2003;92(9):931–939. https://doi.org/10.1046/j.1464-410x.2003.04528.x
Umlauf MG, et al. Menopause. 2000;7(6):356–361. https://doi.org/10.1097/00042192-200007060-00004
Thompson JA, et al. Journal of Women’s Health Physical Therapy. 2020;44(3):145–153. https://doi.org/10.1097/JWH.0000000000000153
Bø K, et al. Obstetrics & Gynecology. 2017;129(3):491–498. https://doi.org/10.1097/AOG.0000000000001909
Hashim H, Abrams P. European Urology. 2006;50(6):1306–1314. https://doi.org/10.1016/j.eururo.2006.07.016
Kavia RB, et al. BJU International. 2006;98(5):1035–1038. https://doi.org/10.1111/j.1464-410X.2006.06308.x
Park S, et al. International Neurourology Journal. 2021;25(4):314–321. https://doi.org/10.5213/inj.2142088.095
Ogata J, et al. Lower Urinary Tract Symptoms. 2016;8(2):90–96. https://doi.org/10.1111/luts.12118
Chung HS, et al. Obstetrics & Gynecology Science. 2021;64(1):42–51. https://doi.org/10.5468/ogs.20331
Hannestad YS, et al. BJOG. 2003;110(3):247–254. https://doi.org/10.1046/j.1471-0528.2003.02200.x
Bø K. Current Opinion in Obstetrics and Gynecology. 2020;32(5):395–400. https://doi.org/10.1097/GCO.0000000000000668
Bø K, et al. Obstetrics & Gynecology. 2017;129(3):491–498. https://doi.org/10.1097/AOG.0000000000001909
Parish SJ, et al. Maturitas. 2019;124:85–90. https://doi.org/10.1016/j.maturitas.2019.03.016
Robinson D, et al. Climacteric. 2021;24(4):379–387. https://doi.org/10.1080/13697137.2020.1852265
Irwin MR. Physiological Reviews. 2015;95(2):553–605. https://doi.org/10.1152/physrev.00032.2014
Sword Health. Bloom ROI Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-pelvic-health-roi
Janela D, et al. JMIR mHealth & uHealth. 2025;13:e68242. https://mhealth.jmir.org/2025/1/e68242
Sword Health. Bloom Health Equity Whitepaper. 2025. https://swordhealth.com/resources/whitepapers/bloom-health-equity