Latest articles
Fresh healthcare insights

Healthcare revenue cycle management explained
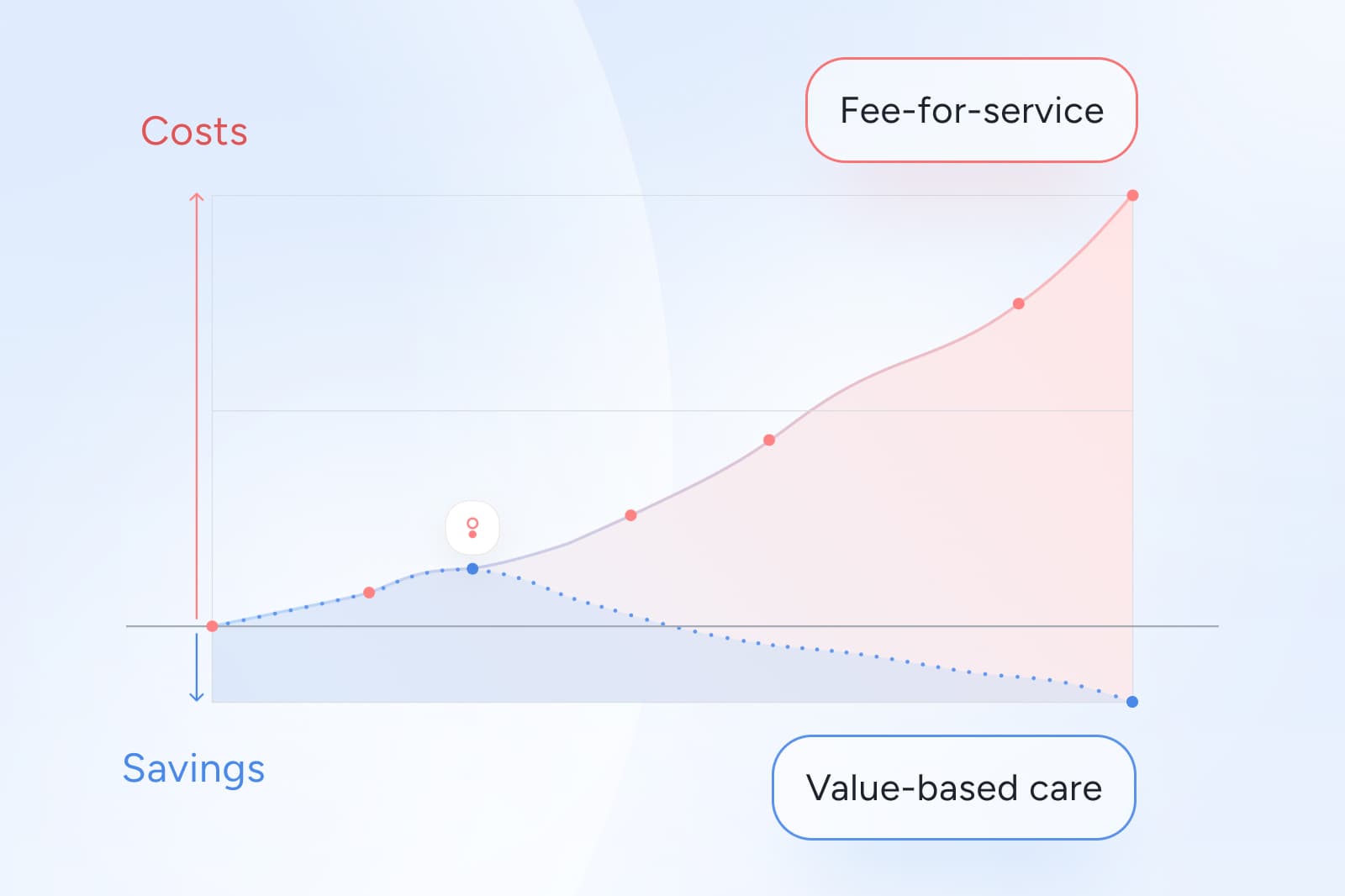
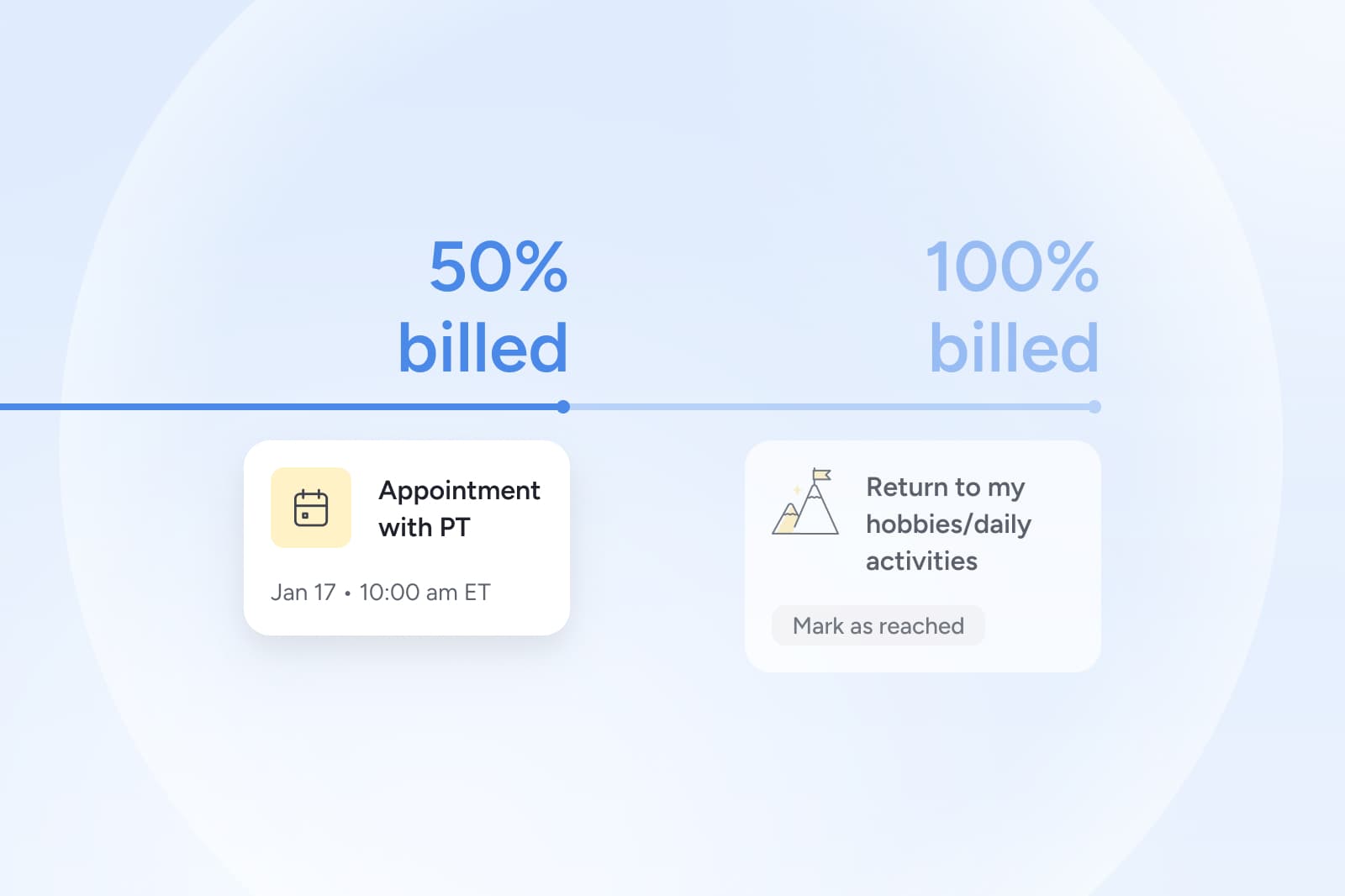
See how healthcare revenue cycle management works, why fee-for-service drives waste, and how value-based care simplifies billing and accountability.
February 20, 2026 • 10 min read
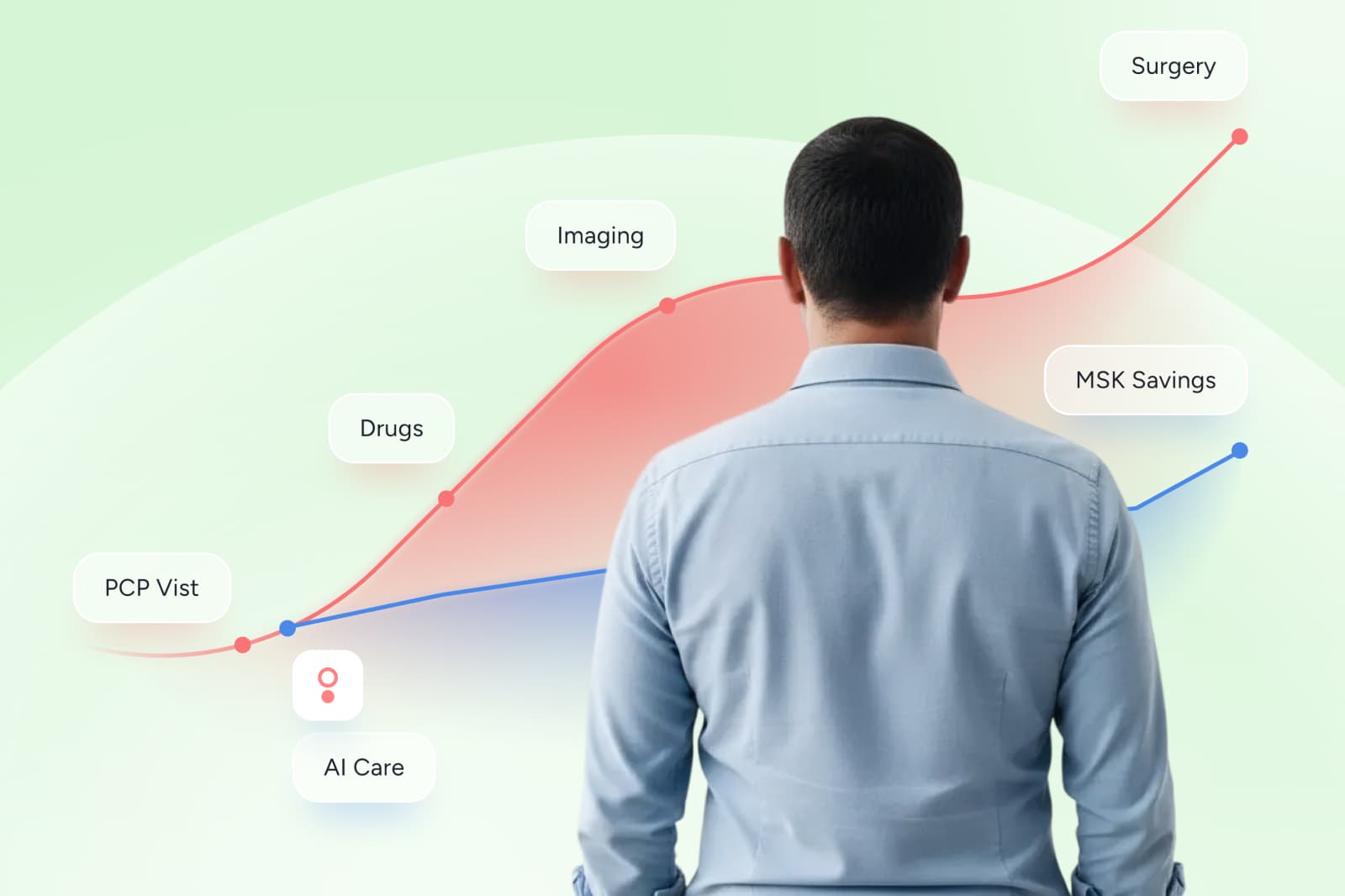
The future of value-based care
Explore the next wave of value-based healthcare trends, from AI-Care to outcome-based pricing and employer-driven models, plus what “future-ready” looks like.
February 19, 2026 • 7 min read

Value-based care programs: real-world examples buyers can trust
Three value-based care program examples in practice, with buyer lessons employers and health plans can use in MSK to make outcomes auditable and pricing clear.
February 19, 2026 • 6 min read
Value-based contracting: 8-step healthcare buyer checklist
A practical guide to value-based contracting in healthcare to help you understand contract clauses that define outcomes, payment triggers, risk sharing, reporting, and audit rights.
February 19, 2026 • 8 min read
Value-based payment and reimbursement explained
Understand the major value-based payment models and what they mean for risk, cash flow, and forecasting in MSK and beyond.
February 19, 2026 • 7 min read

Why leading employers are adding dedicated menopause benefits at work
Offering menopause benefits at work is a cost-effective strategy for retention, productivity, and measurable savings. Here’s what leading employers do and how to evaluate it.
February 18, 2026 • 8 min read

The cost of menopause that employers cannot ignore
The cost of menopause shows up in claims, productivity, and retention. Learn where spend concentrates, why pelvic symptoms matter, and what measurable support looks like.
February 18, 2026 • 8 min read
For employers
Workplace health advice
How digital physical therapy improves employee retention
Benefits that work keep people. Learn which health programs drive retention and how MSK support improves satisfaction, productivity, and culture.
October 24, 2025
GLP-1 employer healthcare costs: lower spend with better outcomes
Learn how GLP-1 programs raise costs and why movement is the key to protecting outcomes and lowering employer spend.
October 23, 2025
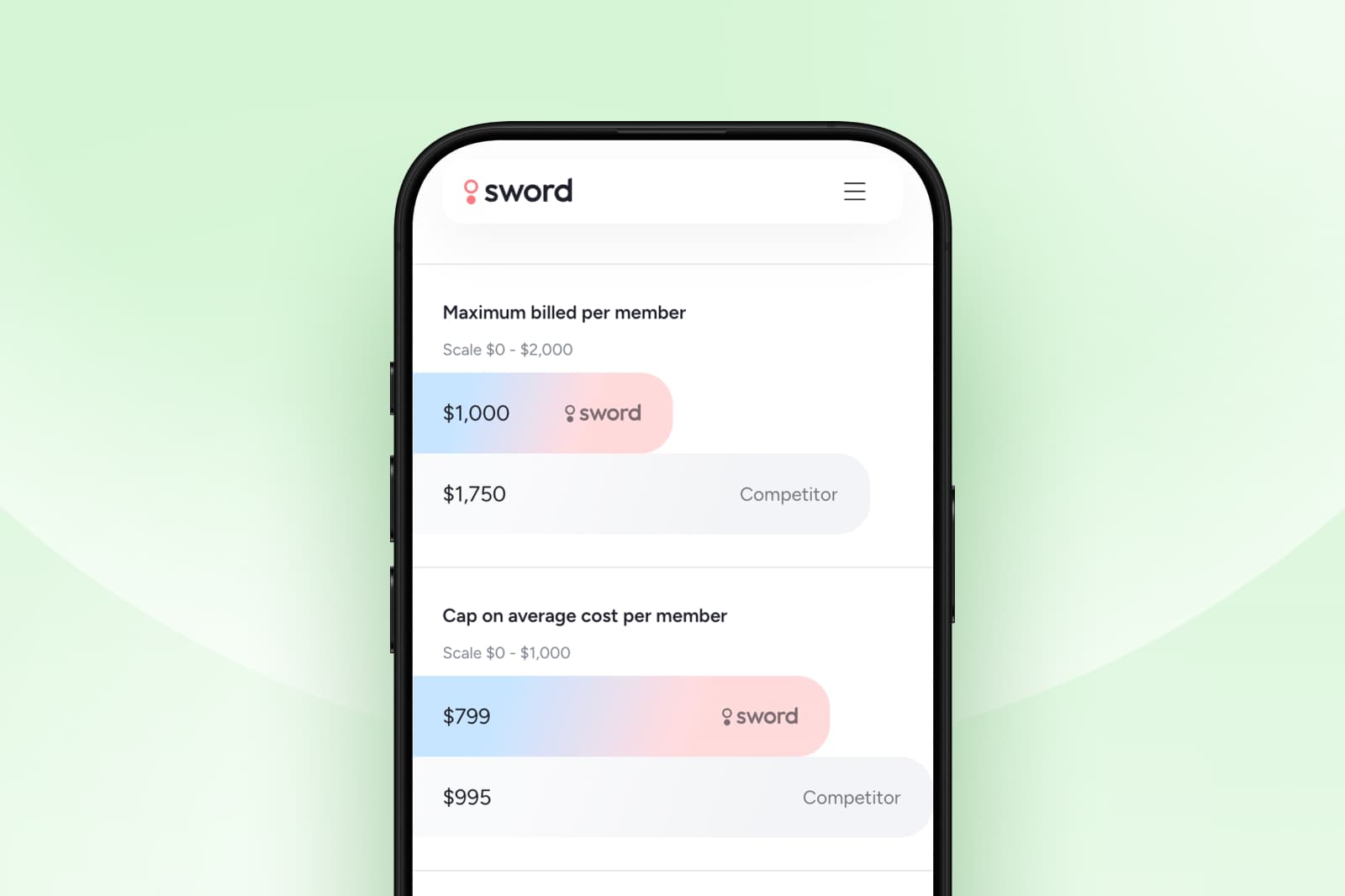
How to evaluate and select the best digital MSK vendors
Find out how to evaluate the best MSK healthcare provider for your company when there are so many choices.
October 24, 2025
Reduce MSK costs with more effective digital MSK care plans
Find out why employers and benefits buyers must make reducing MSK costs a priority, and why digital MSK plans offer stronger ROI.
October 24, 2025
Expert guidance
From the experts: Ask a physical therapist

Ask a PT: Does walking really help with pain?
Megan Hill, Doctor of Physical Therapy, details a walking plan that anyone with pain can manage.
August 13, 2020
Ask a PT: What Is Causing My Shoulder Pain?
Discover the five most common causes of shoulder pain and how to tell them apart.
November 1, 2023

Ask a PT: when is the best time to do my exercises?
Megan Hill, Dr. of Physical Therapy, explores how and when to fit exercise into your busy schedule.
February 11, 2021
Healthcare contributors
Meet Sword's expert authors
Vijay Yanamadala
Chief Medical Officer at Sword Health

Megan Hill
Director, Clinical Specialists

Morgan Hollis
Head of Clinical Strategy, Sword Move

Liz Santo
Senior Clinical Program Manager, Sword Bloom ·

Jennesa Atherton
Head of Clinical Affairs, Sword Bloom

Fernando Correia
SVP Clinical & Regulatory Affairs at Sword Health