October 22, 2025 • min read
Understanding pelvic pain anxiety (and how to help women recover)
Learn how pelvic floor dysfunction impacts mental health and how dedicated women's health care programs can reduce physical and emotional symptoms.
Written by

Senior Clinical Program Manager, Sword Bloom ·
Pelvic health and mental wellbeing are connected
Pelvic floor dysfunction (PFD) is far more common than most people realize. One in three women in the U.S. will experience some form of PFD during her lifetime, and prevalence rises to 40–50% among postmenopausal women.¹ ² Conditions like incontinence, prolapse, and chronic pelvic pain may seem physical in nature, but their effects reach well beyond the body.
Depression is common in women with pelvic-floor dysfunction, at up to 25–35% depending on the specific condition.³ The link between pelvic floor and mental health is profound. Leaks, urgency, pain, and feelings of loss of control create constant stress. Over time, this erodes confidence, alters self-image, and fuels a cycle of shame and avoidance.
For too long, these issues have been dismissed as inevitable or “just part of aging.” The reality is that pelvic health and mental health are inseparable, and ignoring this connection has serious consequences for women and for employers who rely on them.
Pelvic pain anxiety, shame, and loss of confidence is all too common
Pelvic floor issues often manifest in everyday, unpredictable ways. A sudden leak during a presentation, a rush to the restroom in the middle of a meeting, or pain during intimacy can all leave lasting emotional scars.
Women frequently describe feeling anxious about leaving the house, exercising, or participating fully in social or professional activities. The constant “what if” leads to hypervigilance, avoidance, and in many cases, isolation.
At work, these anxieties directly impact performance. Employees may avoid travel, client-facing opportunities, or leadership roles. Shame compounds the problem, as women are often reluctant to discuss these symptoms with managers or HR, leaving them feeling unsupported and struggling in silence. When confidence erodes, career progression stalls, and some women with more chronic symptoms even consider leaving the workforce. Anxiety that begins with pelvic symptoms ripples outward into self-esteem, engagement, and long-term wellbeing.
Forward-thinking health plan managers can reverse this issue by developing specific women's healthcare programs that allow women to manage their symptoms with dedicated pelvic care.
Depression, isolation, and long-term health consequences from pelvic floor dysfunction
Chronic musculoskeletal conditions are well known drivers of depression, and pelvic health problems are no exception. Persistent pelvic pain, urinary urgency, or bowel dysfunction can lead to feelings of hopelessness. Women often report withdrawing from relationships, intimacy, and even friendships to avoid embarrassment and this added emotional burden is matched by physical consequences. Untreated symptoms worsen over time, increasing the likelihood of costly downstream interventions. In fact, surgeries for pelvic floor conditions average nearly $30,000 per case.⁴
From an organizational perspective, the toll is clear. Employees with unmanaged pelvic floor disorders take more sick days, show reduced engagement, and in many cases leave the workforce entirely. In fact, research demonstrates that 62.1% of people with chronic pelvic pain report reduced work productivity5. Losing skilled employees in their most productive years represents a financial and cultural loss few organizations can afford.
Why pelvic health and mental health are linked for women at work
When pelvic health is left out of health benefits strategies, employers miss a critical driver of mental wellbeing. The connection is not abstract. So many women have to deal with the challenges of pelvic floor dysfunction in workplaces everywhere, every day. Women with unmanaged symptoms are more likely to report depression and anxiety, fueling higher rates of mental health claims and prescriptions.³
Retention is another major risk. Around one in six women (17%) have considered leaving work because of unmanaged menopause-related symptoms.10 For women in leadership, these exits or disengagement can undermine senior-talent pipelines and compound gender-equity challenges.
Pelvic health is so closely related to mental health for women in the workplace. When employees are supported with effective, dedicated pelvic care programs, both their physical and emotional wellbeing improve, and so does their performance and retention.
A whole-person approach to pelvic health care stops women suffering in silence
Addressing pelvic health requires more than just treating symptoms in isolation. A whole-person approach recognizes that bladder leaks, pelvic pain, and prolapse affect both the body and the mind.
Digital-first women's health programs make this holistic care possible. By delivering therapy privately and flexibly, they reduce stigma and make it easier for women to engage consistently.
Evidence confirms this model works: in peer-reviewed studies, digital pelvic health programs achieved 77.6% completion rates, with average satisfaction of 8.6 out of 10.⁶ Engagement of this scale is virtually unheard of in traditional clinic settings, where adherence often falls below 50%.
Clinical outcomes are equally strong. In a 2025 JMIR study, 59.5% of members achieved meaningful improvement in symptoms, with significant reductions in both anxiety (76%) and depression (54%).⁷ These results highlight how addressing pelvic health directly alleviates mental health burdens.
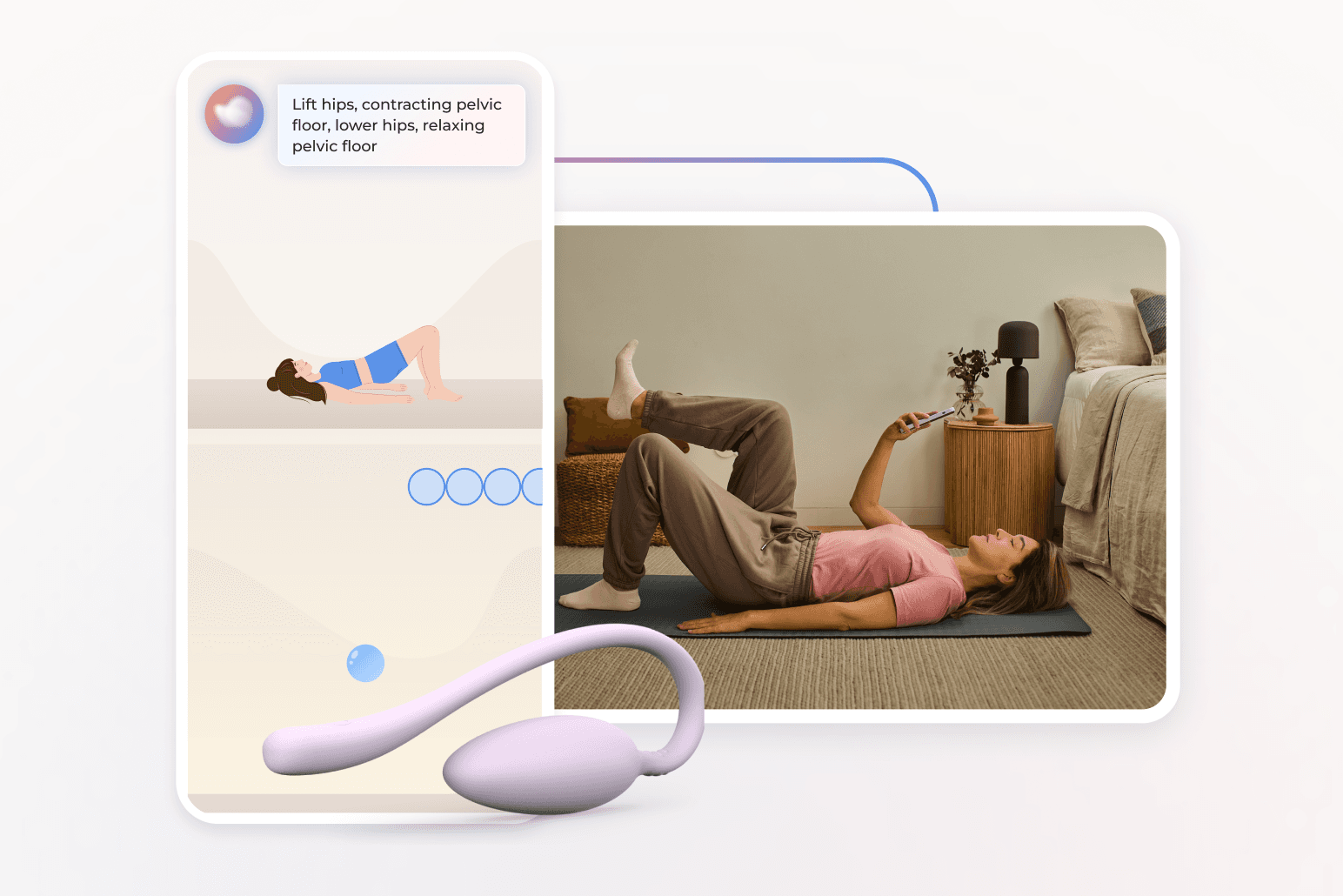
Bloom offers expert digital pelvic health care from home
Bloom by Sword Health was created to solve the very challenges that keep women from seeking care. Too often, traditional models require lengthy wait times, awkward conversations, or long commutes to clinics. Many women simply opt out, suffering in silence while symptoms worsen.
Bloom eliminates these barriers. It delivers pelvic health therapy into women’s homes, with a program built for privacy, flexibility, and expert guidance. This makes care approachable for women who might otherwise avoid it, while also giving employers and health plans confidence that their investment will be used. By adding Bloom into a health benefits plan, organizations can deliver effective women's health care that is accessible, equitable, and clinically-validated.
How Bloom works step-by-step to end pelvic pain
Bloom combines technology and human expertise to deliver care in a way that is both personal and scalable:
- Specialist onboarding: Each member is matched with a Women's Health Specialist who holds a Doctorate in Physical Therapy.
- Personalized plan: The specialist designs a therapy plan tailored to each woman’s symptoms, goals, and life stage.
- The Bloom Pod: Members receive an FDA-listed device that measures pelvic floor muscle contraction and relaxation, providing real-time biofeedback.
- Digital guidance: Through the Sword app, women follow short guided sessions, track progress, and receive continuous support.
- Flexibility: Sessions are private and can be completed anytime. Half occur after work hours, and 22% on weekends.⁸
- Continuous support: Specialists adjust plans as members progress, offering encouragement and accountability.
This model combines clinical rigor with the convenience employees need to actually complete care.
Bloom's proven health outcomes for women
61%
of women with moderate-to-severe symptoms achieve meaningful improvement.⁹
9/10
The average member satisfaction rating of Bloom members⁹
56%
of Bloom members report a reduction in anxiety
50%
average improvement in productivity after nine sessions using Bloom
The organizational case for Bloom's women's health care
Employers and health plans face increasing pressure to show ROI on every benefit. With Bloom, the case is straightforward:
- Healthcare savings: Bloom reduces costly surgeries and unnecessary imaging, cutting pelvic-specific spend by $2,276 per member per year.⁹
- Mental health outcomes: By addressing pelvic dysfunction, Bloom reduces depression and anxiety, lowering mental health claims and pharmacy costs.⁷
- Productivity and retention: With symptoms under control, employees are more focused, engaged, and less likely to leave.
- Equity and inclusion: Nearly half of Bloom members live in moderate-to-high social deprivation areas, yet achieve equivalent outcomes to peers, closing longstanding gaps in care.⁸
Whole-person pelvic care is no longer optional. It is a strategic lever for workforce health, equity, and financial resilience.
Start offering Bloom now to help your team manage pelvic pain and anxiety
Pelvic floor dysfunction is not just a medical issue. It is a driver of mental health, productivity, and workforce stability. Employers that ignore it risk higher costs, stalled careers, and the loss of talented women.
Bloom changes this trajectory. By combining expert clinical care with digital convenience, it gives women relief from both physical symptoms and emotional burdens. For organizations, Bloom delivers measurable ROI while advancing equity and inclusion.
Stop women suffering in silence with pelvic pain
Offer women life-changing support and slash claim costs driven by pelvic health conditions with Bloom's digital pelvic care plans.
Footnotes
Kenne K, et al. Sci Rep. 2022;12:9878. doi:10.1038/s41598-022-13501-w.
Janela D, et al. JMIR mHealth UHealth. 2025;13:e68242. doi:10.2196/68242. https://mhealth.jmir.org/2025/1/e68242
Peinado Molina RA et al. Prevalence of depression & anxiety in women with pelvic floor dysfunctions: systematic review & meta-analysis. Int J Gynecol Obstet. 2024. https://doi.org/10.1002/ijgo.15719
Lamin, E., Parrillo, L.M., Newman, D.K., Smith, A.L. Pelvic Floor Muscle Training: Underutilization in the USA. Current Urology Reports. 2016;17:10. https://doi.org/10.1007/s11934-015-0572-0
Hutton D, Mustafa A, Patil S et al. The burden of Chronic Pelvic Pain (CPP): Costs and quality of life of women and men with CPP treated in outpatient referral centres. PLoS One. 2023;18(2):e0269828. https://doi.org/10.1371/journal.pone.0269828
Janela D, et al. JMIR mHealth UHealth. 2025;13:e68242. doi:10.2196/68242. https://mhealth.jmir.org/2025/1/e68242
Janela D, et al. JMIR mHealth UHealth. 2025;13:e68242. doi:10.2196/68242. https://mhealth.jmir.org/2025/1/e68242
Sword Health, Bloom Impact on Health Equity Whitepaper, 2024. https://swordhealth.com/insights/gated-reports/bloom-health-equity
Sword Health, Bloom ROI Whitepaper, 2025, validated by Risk Strategies Consulting. https://swordhealth.com/insights/gated-reports/bloom-pelvic-health-roi
CIPD “Menopause in the workplace: Employee experiences in 2023”. Simply Health