Fresh health insights

Weight loss drugs and muscle loss: MSK risks to avoid
Weight loss drugs are rewriting the obesity care playbook. GLP-1s like semaglutide, liraglutide, and others are helping members lose weight, improve metabolic markers, and avoid high-risk interventions like surgery. Many employers and health plans have fast-tracked these medications into formularies as a cornerstone of chronic condition management. But there’s one effect that most treatment programs overlook and it’s not related to fat loss.
August 20, 2025 • 11 min read

Semaglutide and muscle loss: what health plans need to know
Semaglutide and muscle loss: what health plans need to know Semaglutide has transformed the obesity treatment landscape. Originally approved as a diabetes drug, it’s now among the most widely prescribed GLP-1 medications for weight management, often more commonly known by brand names like Ozempic, Wegovy, and Rybelsus. With outcomes that include 10%–15% total body weight loss and improved cardiometabolic markers¹, it’s no surprise health plans are rapidly expanding coverage. Semaglutide offers a powerful new lever to address obesity-related costs and long-term risk.
July 21, 2025 • 10 min read

GLP-1 preauthorization: Using movement plans for sustained weight loss
GLP-1 medications have redefined obesity care for employers and health plans. These powerful drugs support members at high metabolic risk with significant short-term weight loss. But without behavior change and muscle preservation, long-term success can become more elusive. Many patients on GLP-1s experience rebound weight gain and muscle deterioration, which presents an increased risk of musculoskeletal conditions and downstream costs₁³. Employers and health plans have a promising treatment that is effective in supporting fast weight loss. However, without positive behavior change to accompany a GLP-1 prescription, the healthy habit of regular physical activity is missing.
July 21, 2025 • 9 min read
Why effective employer perks matter more than ever to employees
In today's fiercely competitive labor market, the perks and benefits an employer offers are often the deciding factor for top-tier candidates weighing multiple job offers. With remote work, global hiring, and salary transparency eroding traditional hiring advantages, perks have become a key differentiator. But not all perks are created equal. Organizations must distinguish between shallow, performative perks and those that deliver meaningful, measurable value to employees and the business. The shift in worker expectations is real and data-backed. According to MetLife's 2023 Employee Benefits Trends Study, 61% of employees say that benefits are the deciding factor in accepting a new job offer.¹ Even more striking, nearly 73% of workers say they would stay longer at a company that offers high-quality health benefits.²
August 19, 2025 • 9 min read

Wellness programs that boost employee productivity
The line between wellness and performance has never been thinner. In today’s workplace, where hybrid schedules blur boundaries and job expectations run high, employee health is no longer just a nice-to-have. It’s a strategic lever. Benefits leaders know this. They’ve spent years investing in wellness platforms that promise mindfulness, fitness, and better sleep. But the real question is: are those programs actually driving productivity?
August 21, 2025 • 13 min read
Enhancing employee engagement through health benefits
Employee engagement is more than a cultural buzzword. For enterprise organizations, it’s a proven driver of performance, retention, and business growth. But keeping teams motivated and committed requires more than pizza Fridays or inspirational Slack messages. This demands real support. Preventative healthcare benefits that allow employees to bring their best self to work provide an effective return on investment for proative employers. Meaningful, effective healthcare benefits are valuable for employers and employees alike. In a world where health, work, and home life constantly overlap, employees expect their employers to offer more than generic wellness perks.
August 21, 2025 • 8 min read

Digital care is transforming health benefits with measurable ROI
Healthcare innovation is no longer about building more hospitals. It’s about removing the barriers that keep people from getting the care they need, when they need it. The traditional care model, while foundational, has not kept pace with the shifting demands of today’s increasingly hybrid, dispersed, and time-strapped workforce. Employees are looking for health solutions that are convenient, personalized, and deliver real results. That’s why digital care has emerged as one of the most transformative developments in modern health. It’s not just a shift in delivery method, it’s a strategic pivot that improves engagement, accelerates recovery, and produces measurable cost savings for employers. What was once considered an optional or supplementary model of care is now becoming the standard for innovation-driven employers. In this article, we explore why digital healthcare delivers stronger ROI, how it solves the usage and outcome gaps in traditional models, and why Sword Health leads the way with a proven, data-backed digital MSK care solution that drives value at scale.
August 21, 2025 • 10 min read
All about workplace health
How Digital Physical Therapy Improves Employee Retention
Did you know that fear of pain can be more disabling than pain itself? Half of American adults suffer from musculoskeletal (MSK) pain, negatively impacting job satisfaction and quality of life. Pain makes it difficult to even show up to work. Nearly 28% of people in the workplace will take leave for MSK pain over the course of a year. Patients who suffer the two most common conditions of low back and neck pain have an average return to work of 7 days.
September 27, 2022 • 5 min read
How to evaluate and select the best digital MSK vendors
Musculoskeletal (MSK) disorders are one of the most expensive and under-addressed cost centers facing U.S. healthcare providers. MSK disorders affect 1 in 2 Americans and cost over $190 billion per year, more than heart disease, cancer, or mental health conditions. For employers and health plans, MSK claims are often among the top 3 cost drivers. And for members, chronic pain reduces quality of life, drives absenteeism, and often leads to costly downstream interventions. That’s why digital MSK solutions have surged in popularity. The promise is compelling: better access, which drives stronger engagement, delivers better outcomes, and therefore lowers overall healthcare costs.
August 13, 2020 • 6 min read
5 Reasons Why MSK Care is a Top Priority for Employers
You’ve likely seen numerous digital health solutions that promise to lower medical spend. You’ve probably zeroed in on the top conditions with significant digital solutions in the marketplace: musculoskeletal (MSK), mental health, and diabetes. For most companies, prioritizing MSK care over other digital health solutions will drive the biggest benefits for your employees and your bottom line when it comes to savings. Given the multitude of vendors, platforms, and solutions available, prioritization can be a daunting task. How do you choose from among the thousands of digital health tools? What combination of condition focus and solution selection will drive the best outcomes for your population and the biggest return for your business?
September 19, 2022 • 5 min read
Tackling the #1 driver of employers’ health costs: MSK
The phrase ‘musculoskeletal disorder’ may not ring a bell — but the feeling might. The term refers to any type of pain in the muscles or joints, from chronic pain to injuries to post-surgical pain. Many of us have suffered from a musculoskeletal (MSK) issue at some point in our lives. In fact, one in two Americans is struggling with an MSK condition right now. And it’s causing economic ripples, especially in the workplace.
January 20, 2020 • 6 min read
More from Sword: Ask a physical therapist

Ask a PT: when is the best time to do my exercises?
Before I joined Sword Health, I worked in brick-and-mortar clinics. I never worked weekends, and rarely worked past 6 pm. My schedule was great...for me. But for my patients, it was a real challenge. Attending a physical therapy appointment might require leaving work early or slipping out at lunch. Even patients with more flexible schedules would sometimes lament about finding childcare or arranging transportation. A thirty-minute appointment could easily take an hour or even 90 minutes once travel was taken into account. When I was in a clinic, the “best” time for a patient to do their exercises was the time that worked for me, not for them. Sword's virtual model gives our members the power to do their exercises when AND where it's most convenient for them. Now that I work remotely for Sword, I’m able to help our members figure out the best time to do their exercises at home. Now, when my members ask me when they should do their exercises, I tell them - the best time is when you’ll actually do them!
February 11, 2021 • 6 min read

Ask a PT: Does walking really help with pain?
If you’ve ever stood on the sidelines of a sporting event, you’ve likely witnessed many falls, trips and tackles. Whether the players are small children or professional athletes, the advice from the coach may have simply been to “walk it off.” While that is not always the best solution after an acute injury, walking can be a really effective way to manage chronic pain. Motion is lotion. Movement increases blood flow, which brings nutrients to our tissues. It also helps those that don’t have blood flow, like cartilage. Cartilage lines our joints, absorbing impact. It’s surrounded by a liquid which provides it with nutrients, flowing in and out of it like a sponge. Exercise, like walking, causes loading that fills and squeezes that sponge, particularly in the joints of our legs and spine.
August 13, 2020 • 4 min read

Ask a PT: What Is Causing My Shoulder Pain?
When your shoulder hurts, it can be difficult to tell exactly what’s gone wrong. You’ve probably heard of pinched nerves and rotator cuff tears. Perhaps you’ve also heard about shoulders being ‘impinged’ or ‘frozen.’ It’s not easy to keep these various shoulder conditions straight, especially when they all cause similar pain symptoms. The first step towards fixing a problem is identifying it. This article, written by a team of Doctors of Physical Therapy, is designed to help you figure out what’s causing your shoulder pain — so you can begin the process of healing it. We will dive into the five most common causes of shoulder pain and how to differentiate them. Cervical refers to the neck, and radiculopathy is pain that radiates to another body part. Hence, cervical radiculopathy: a pinched nerve in the neck, which can cause radiating pain affecting the shoulder. It occurs when the cervical spine becomes damaged due to sudden injury or degeneration over time, and squeezes or puts pressure on a nearby nerve.
February 20, 2024 • 6 min read
Meet our editors

Sword Editorial Team
Experts in pain, movement, and digital health
The Sword Editorial Team brings together expert clinicians, researchers, and health writers dedicated to clear, evidence-based insights on pain, movement, and digital care. The team is always focused on Sword’s mission to free the world from pain and draws on backgrounds in physical therapy, pelvic health, mental health, behavioral science, and health policy.

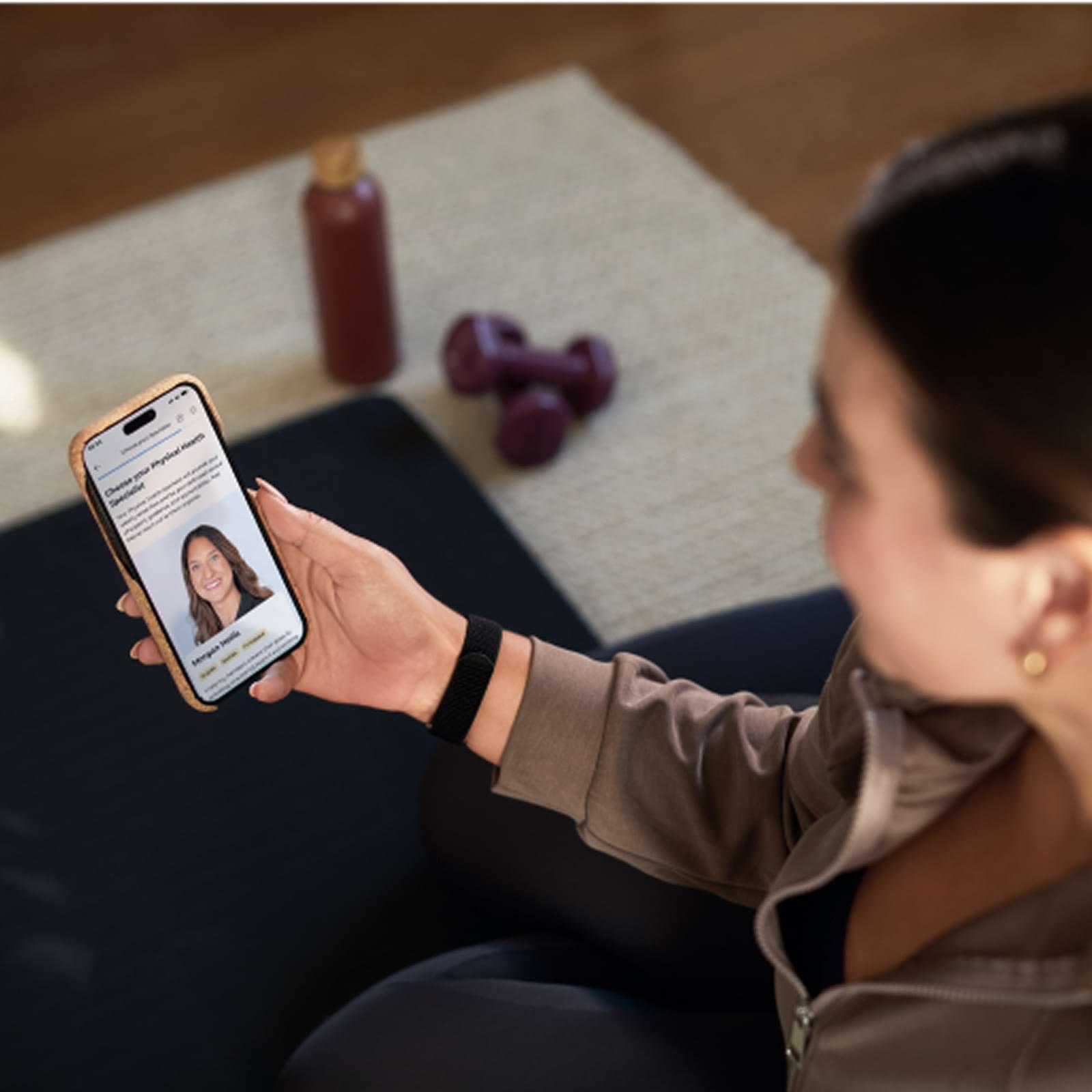
Megan Hill, PT, DPT
Director, Clinical Specialists, Doctor of Physical Therapy
Megan specializes in musculoskeletal rehabilitation and chronic pain management. After a knee injury from the Chicago Marathon led her to discover the power of PT firsthand, she dedicated her career to helping others regain strength and movement. Megan holds a Doctor of Physical Therapy from the University of Illinois at Chicago and a BA in psychology from Duke University.

Dr. Fernando Correia, M.D.
Founding Team & SVP Clinical & Regulatory Affairs
Dr. Fernando Correia is a physician specializing in Neurology and a member of the company’s founding team. He leads clinical validation and medical affairs at Sword, with his work driven by his belief that technology and human connection can make high-quality, evidence-based care accessible for all.







